Tuesday Poster Session
Category: Liver
P5890 - Hepatic Steatosis Is Associated With Amplified Hypoglycemia and Diabetic Ketoacidosis Risk in Type 2 Diabetes: A Multicenter Propensity-Matched Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sudheer Dhoop, MD
University of Toledo College Medicine and Life Sciences
Toledo, Ohio
Presenting Author(s)
Sudheer Dhoop, MD1, Mohammed Abu-Rumaileh, MD2, Keith Burns, MD1, Monica Tincopa, MD3, Mona Hassan, MD4
1University of Toledo College Medicine and Life Sciences, Toledo, OH; 2The University of Toledo, Toledo, OH; 3UCSD, San Diego, CA; 4Division of Gastroenterology & Hepatology, Toledo, OH
Introduction: Metabolic-associated steatotic liver disease (MASLD) affects ≈30 % of U.S. adults and frequently overlaps with type-2 diabetes mellitus (T2DM). MASLD has been linked to cardiovascular events, but whether the hepatic steatosis, independent of shared cardiometabolic risk-factors (CMRFs), worsens glycemic control is unclear. We aim to assess whether hepatic steatosis increases risk of life threatening T2DM complications such as hypoglycemia and diabetic ketoacidosis.
Methods: Using the TriNetX U.S. network we performed a retrospective, propensity-matched cohort study. Adults with T2DM plus ≥1 CMRF (over-weight/obesity, hypertension or dyslipidemia) were allocated to (i) MASLD—ICD-10 code for fatty liver/NASH and ALT > 35 U L⁻¹, versus (ii) Metabolic-abnormalities-only (MA)—same CMRFs but no steatosis codes and ALT ≤ 25 U L⁻¹. Individuals with type-1 diabetes, advanced CKD, any cirrhosis, viral or alcoholic liver disease or documented alcohol use were excluded. Covariates (sex, race/ethnicity, diabetes complications, BMI, HbA1c strata, anti-diabetic drugs, social determinants) were balanced 1:1 with greedy nearest-neighbor matching (caliper 0.1, pooled SMD < 0.1). Primary and secondary outcomes were 5-year (y) time-to-first ICD-coded severe hypoglycemia and diabetic ketoacidosis (DKA). Proportional-hazards assumptions were tested; adjusted hazard-ratios (aHR) derived from time-dependent Cox models.
Results: 15,462 MASLD and 1,030,406 MA met criteria; after matching each cohort had 13,641 patients (mean age 55.5 y, 41 % men, 57 % BMI ≥ 30 kg/m²). Despite the MA group being older with higher baseline HbA1c, MASLD carried greater 5-y risk of severe hypoglycemia: 8.35 % vs 7.07 % (aHR 1.19, 95 % CI 1.08–1.30, p < 0.001) and DKA: 6.95 % vs 5.09 % (aHR 1.40, 95 % CI 1.26–1.55, p < 0.001). Kaplan–Meier curves diverged early and widened steadily.
Discussion: Hepatic steatosis independently amplifies the risks of severe hypoglycemia and DKA in T2DM, corroborating physiologic principles that fatty liver impairs glycemic control. Recognizing MASLD as more than incidental supports early screening and use of liver-directed treatments such as resmetirom and GLP-1 receptor agonists and judicious de-escalation of hypoglycemic drugs such as insulin and sulfonylureas. Despite its retrospective, code-based design, this study strengthens the case for prospective trials with imaging-validated steatosis metrics and continuous glucose monitoring to see whether reducing liver fat yields fewer glycemic crises.
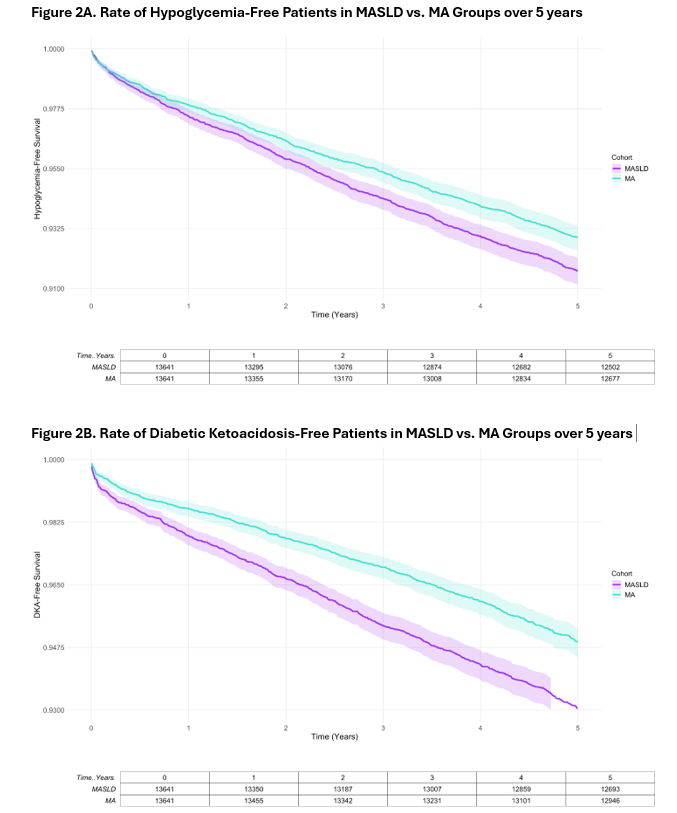
Figure: Table 1. Post Propensity Matched Baseline for MASLD and Metabolic Association (MA) only groups.
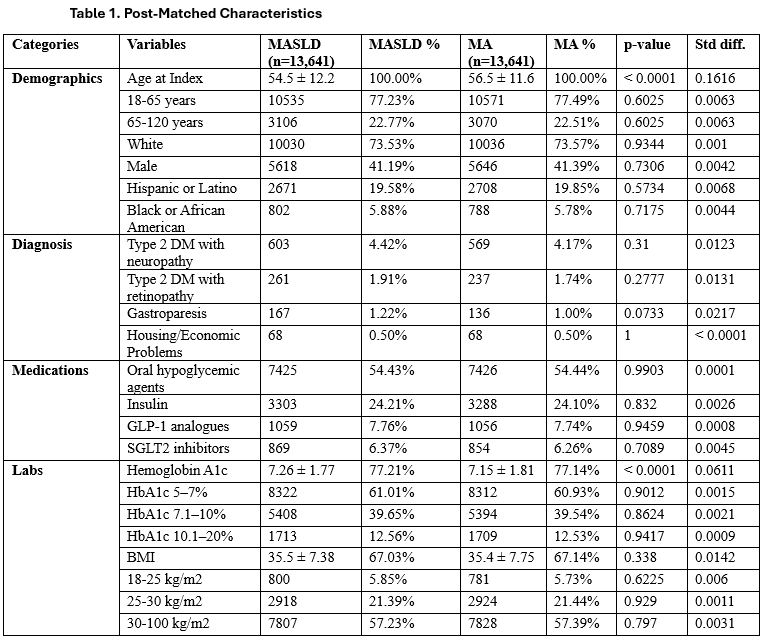
Figure: Figure 1. Kaplan–Meier Curves for Five-Year Hypoglycemia-Free and DKA-Free Survival in MASLD versus Metabolic-Association Only Cohorts.
Disclosures:
Sudheer Dhoop indicated no relevant financial relationships.
Mohammed Abu-Rumaileh indicated no relevant financial relationships.
Keith Burns indicated no relevant financial relationships.
Monica Tincopa indicated no relevant financial relationships.
Mona Hassan indicated no relevant financial relationships.
Sudheer Dhoop, MD1, Mohammed Abu-Rumaileh, MD2, Keith Burns, MD1, Monica Tincopa, MD3, Mona Hassan, MD4. P5890 - Hepatic Steatosis Is Associated With Amplified Hypoglycemia and Diabetic Ketoacidosis Risk in Type 2 Diabetes: A Multicenter Propensity-Matched Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Toledo College Medicine and Life Sciences, Toledo, OH; 2The University of Toledo, Toledo, OH; 3UCSD, San Diego, CA; 4Division of Gastroenterology & Hepatology, Toledo, OH
Introduction: Metabolic-associated steatotic liver disease (MASLD) affects ≈30 % of U.S. adults and frequently overlaps with type-2 diabetes mellitus (T2DM). MASLD has been linked to cardiovascular events, but whether the hepatic steatosis, independent of shared cardiometabolic risk-factors (CMRFs), worsens glycemic control is unclear. We aim to assess whether hepatic steatosis increases risk of life threatening T2DM complications such as hypoglycemia and diabetic ketoacidosis.
Methods: Using the TriNetX U.S. network we performed a retrospective, propensity-matched cohort study. Adults with T2DM plus ≥1 CMRF (over-weight/obesity, hypertension or dyslipidemia) were allocated to (i) MASLD—ICD-10 code for fatty liver/NASH and ALT > 35 U L⁻¹, versus (ii) Metabolic-abnormalities-only (MA)—same CMRFs but no steatosis codes and ALT ≤ 25 U L⁻¹. Individuals with type-1 diabetes, advanced CKD, any cirrhosis, viral or alcoholic liver disease or documented alcohol use were excluded. Covariates (sex, race/ethnicity, diabetes complications, BMI, HbA1c strata, anti-diabetic drugs, social determinants) were balanced 1:1 with greedy nearest-neighbor matching (caliper 0.1, pooled SMD < 0.1). Primary and secondary outcomes were 5-year (y) time-to-first ICD-coded severe hypoglycemia and diabetic ketoacidosis (DKA). Proportional-hazards assumptions were tested; adjusted hazard-ratios (aHR) derived from time-dependent Cox models.
Results: 15,462 MASLD and 1,030,406 MA met criteria; after matching each cohort had 13,641 patients (mean age 55.5 y, 41 % men, 57 % BMI ≥ 30 kg/m²). Despite the MA group being older with higher baseline HbA1c, MASLD carried greater 5-y risk of severe hypoglycemia: 8.35 % vs 7.07 % (aHR 1.19, 95 % CI 1.08–1.30, p < 0.001) and DKA: 6.95 % vs 5.09 % (aHR 1.40, 95 % CI 1.26–1.55, p < 0.001). Kaplan–Meier curves diverged early and widened steadily.
Discussion: Hepatic steatosis independently amplifies the risks of severe hypoglycemia and DKA in T2DM, corroborating physiologic principles that fatty liver impairs glycemic control. Recognizing MASLD as more than incidental supports early screening and use of liver-directed treatments such as resmetirom and GLP-1 receptor agonists and judicious de-escalation of hypoglycemic drugs such as insulin and sulfonylureas. Despite its retrospective, code-based design, this study strengthens the case for prospective trials with imaging-validated steatosis metrics and continuous glucose monitoring to see whether reducing liver fat yields fewer glycemic crises.
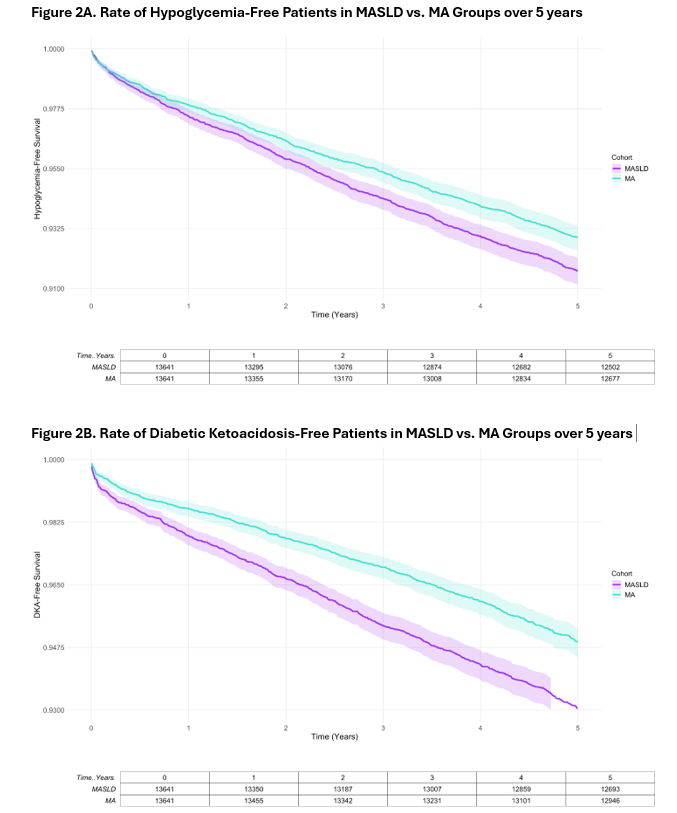
Figure: Table 1. Post Propensity Matched Baseline for MASLD and Metabolic Association (MA) only groups.
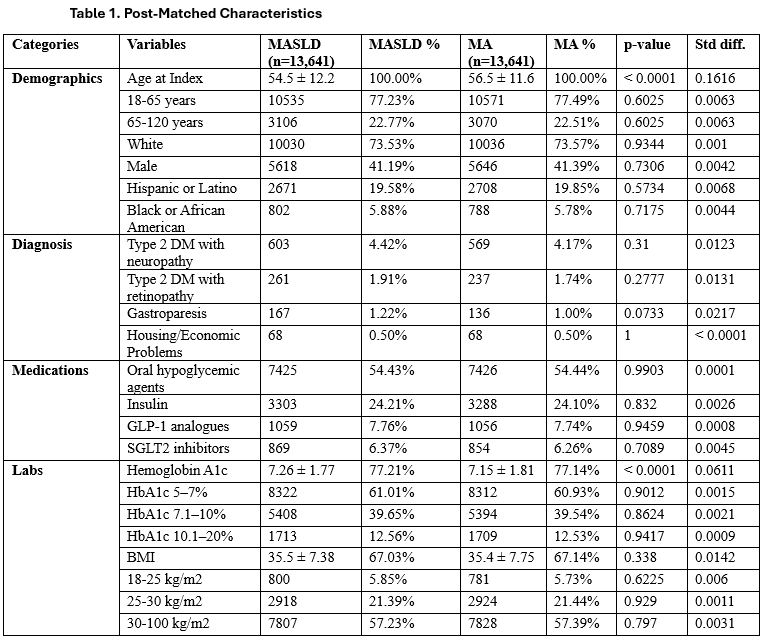
Figure: Figure 1. Kaplan–Meier Curves for Five-Year Hypoglycemia-Free and DKA-Free Survival in MASLD versus Metabolic-Association Only Cohorts.
Disclosures:
Sudheer Dhoop indicated no relevant financial relationships.
Mohammed Abu-Rumaileh indicated no relevant financial relationships.
Keith Burns indicated no relevant financial relationships.
Monica Tincopa indicated no relevant financial relationships.
Mona Hassan indicated no relevant financial relationships.
Sudheer Dhoop, MD1, Mohammed Abu-Rumaileh, MD2, Keith Burns, MD1, Monica Tincopa, MD3, Mona Hassan, MD4. P5890 - Hepatic Steatosis Is Associated With Amplified Hypoglycemia and Diabetic Ketoacidosis Risk in Type 2 Diabetes: A Multicenter Propensity-Matched Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
