Tuesday Poster Session
Category: Liver
P5887 - Impact of Malnutrition on Clinical Outcomes in Hepatocellular Carcinoma Patients With Gastrointestinal Bleeding: A Propensity Score-Matched Population-Based Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Kevin Robinson, MD
Jefferson Einstein Hospital
Philadelphia, PA
Presenting Author(s)
Kevin Robinson, MD1, Colton Jones, MD1, Warren Robinson, MBBS2, Karecia Byfield, MBBS1, Irhoboudu D. Atogwe, MD1, Fnu Deepali, MD1, Jabari Munroe, MD3, Victor Navarro, MD4
1Jefferson Einstein Hospital, Philadelphia, PA; 2Kingston Public Hospital, Jamaica, Kingston, Kingston, Jamaica; 3Decatur Memorial Hospital, Decatur, IL; 4Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Malnutrition is a risk factor for adverse outcomes in a variety of clinical scenarios. This modifiable risk factor has the potential to significantly impact overall prognosis in patients with hepatocellular carcinoma. Our study aims to evaluate the impact of malnutrition on clinical outcomes in hepatocellular carcinoma (HCC) patients with concurrent gastrointestinal (GI) bleeding.
Methods: We utilized data from the Global Collaborative Network TrinetX platform for statistical analysis and cohort identification. Participants aged 18 and older were identified using relevant ICD-10 CM codes. Cohorts were stratified into 2 groups: Cohort 1 comprised of patients with HCC, GI bleeding, and concomitant malnutrition. Cohort 2 was comprised of patients with HCC and GI bleeding but without malnutrition. Cohorts were propensity score matched based on demographics and comorbidities. The primary aim was to assess clinical outcomes including the incidence of sepsis, all-cause mortality, spontaneous bacterial peritonitis (SBP), need for transfusion, hepatic encephalopathy (HE), myocardial infarction, pulmonary embolism, and hepatorenal syndrome (HRS) over a 5-year period. Patients with outcomes before the study window were excluded from the analysis. Multivariate logistic regression analysis was used to measure the association, and estimates were presented as risk ratios with 95% confidence interval.
Results: After propensity score matching, 4,923 participants were included in each cohort. In cohort 1, 69.1% were male, 60% were White, and the mean age was 69.7 years (SD +/- 11.1). In cohort 2, 68.9% were male, 61% were White and the mean age was 69.7 years (SD +/- 11.3). Participants admitted with malnutrition had a statistically significantly higher risk of sepsis (RR:1.483, 95% CI: 1.324-1.661), all-cause mortality (RR:1.165, 95% CI:1.118-1.213), SBP (RR:1.309, 95% CI:1.080-1.587), need for transfusion (RR:1.429, 95% CI:1.260-1.621), HE (RR:1.205, 95% CI:1.076-1.350), myocardial infarction (RR:1.305, 95% CI:1.074-1.586), and HRS (RR:1.549, 95% CI:1.297-1.849) when compared to those without malnutrition (Table 1).
Discussion: Malnutrition significantly increases mortality, risk of SBP and sepsis, HE, HRS, myocardial infarction, and need for transfusions in HCC patients with GI bleeding. This underscores the importance of comprehensive nutritional assessment and optimization of nutritional status in these patients.
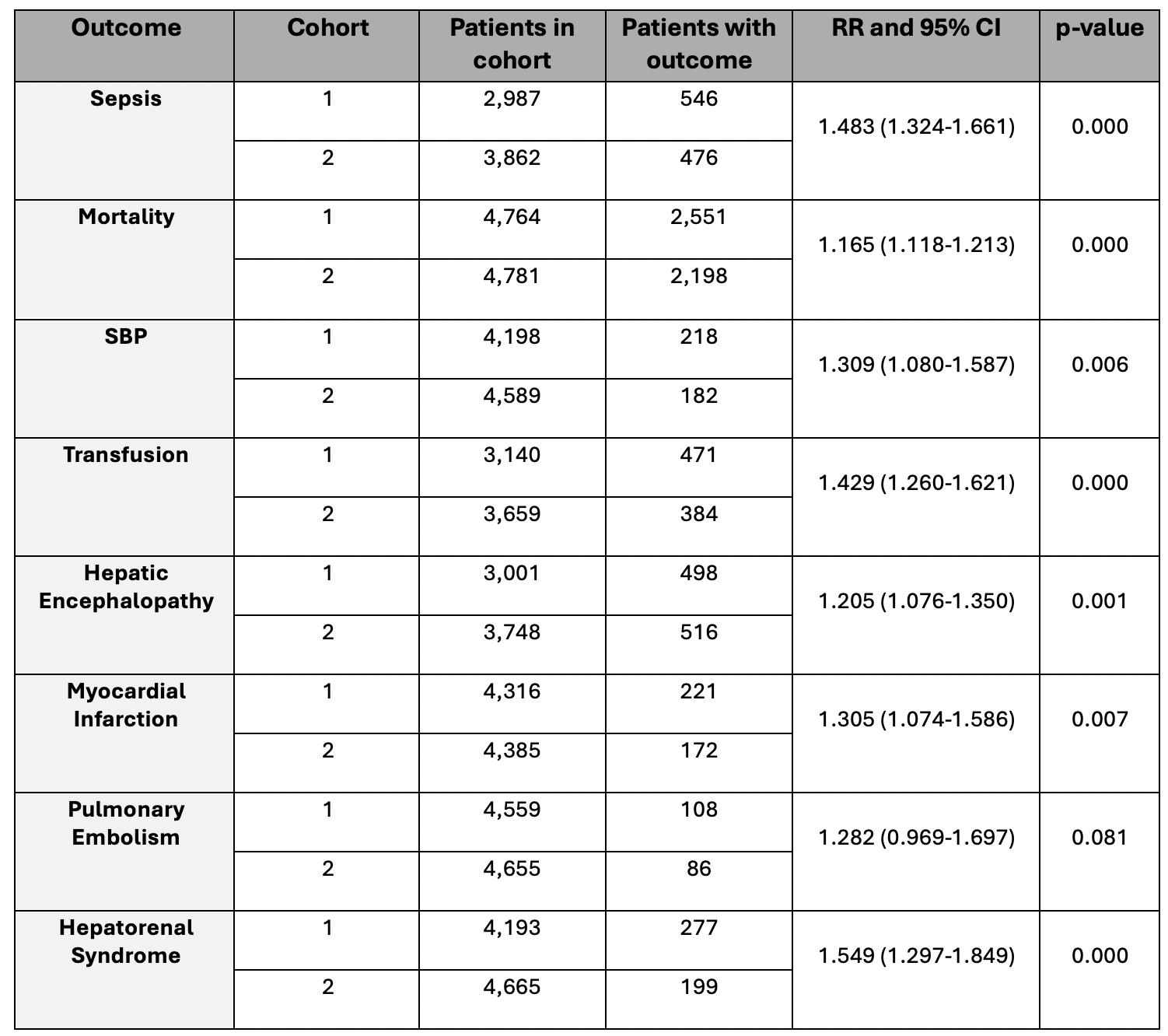
Figure: Table 1: Clinical Outcomes in Cohort 1 and Cohort 2 After Propensity Score Matching
Disclosures:
Kevin Robinson indicated no relevant financial relationships.
Colton Jones indicated no relevant financial relationships.
Warren Robinson indicated no relevant financial relationships.
Karecia Byfield indicated no relevant financial relationships.
Irhoboudu Atogwe indicated no relevant financial relationships.
Fnu Deepali indicated no relevant financial relationships.
Jabari Munroe indicated no relevant financial relationships.
Victor Navarro indicated no relevant financial relationships.
Kevin Robinson, MD1, Colton Jones, MD1, Warren Robinson, MBBS2, Karecia Byfield, MBBS1, Irhoboudu D. Atogwe, MD1, Fnu Deepali, MD1, Jabari Munroe, MD3, Victor Navarro, MD4. P5887 - Impact of Malnutrition on Clinical Outcomes in Hepatocellular Carcinoma Patients With Gastrointestinal Bleeding: A Propensity Score-Matched Population-Based Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jefferson Einstein Hospital, Philadelphia, PA; 2Kingston Public Hospital, Jamaica, Kingston, Kingston, Jamaica; 3Decatur Memorial Hospital, Decatur, IL; 4Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Malnutrition is a risk factor for adverse outcomes in a variety of clinical scenarios. This modifiable risk factor has the potential to significantly impact overall prognosis in patients with hepatocellular carcinoma. Our study aims to evaluate the impact of malnutrition on clinical outcomes in hepatocellular carcinoma (HCC) patients with concurrent gastrointestinal (GI) bleeding.
Methods: We utilized data from the Global Collaborative Network TrinetX platform for statistical analysis and cohort identification. Participants aged 18 and older were identified using relevant ICD-10 CM codes. Cohorts were stratified into 2 groups: Cohort 1 comprised of patients with HCC, GI bleeding, and concomitant malnutrition. Cohort 2 was comprised of patients with HCC and GI bleeding but without malnutrition. Cohorts were propensity score matched based on demographics and comorbidities. The primary aim was to assess clinical outcomes including the incidence of sepsis, all-cause mortality, spontaneous bacterial peritonitis (SBP), need for transfusion, hepatic encephalopathy (HE), myocardial infarction, pulmonary embolism, and hepatorenal syndrome (HRS) over a 5-year period. Patients with outcomes before the study window were excluded from the analysis. Multivariate logistic regression analysis was used to measure the association, and estimates were presented as risk ratios with 95% confidence interval.
Results: After propensity score matching, 4,923 participants were included in each cohort. In cohort 1, 69.1% were male, 60% were White, and the mean age was 69.7 years (SD +/- 11.1). In cohort 2, 68.9% were male, 61% were White and the mean age was 69.7 years (SD +/- 11.3). Participants admitted with malnutrition had a statistically significantly higher risk of sepsis (RR:1.483, 95% CI: 1.324-1.661), all-cause mortality (RR:1.165, 95% CI:1.118-1.213), SBP (RR:1.309, 95% CI:1.080-1.587), need for transfusion (RR:1.429, 95% CI:1.260-1.621), HE (RR:1.205, 95% CI:1.076-1.350), myocardial infarction (RR:1.305, 95% CI:1.074-1.586), and HRS (RR:1.549, 95% CI:1.297-1.849) when compared to those without malnutrition (Table 1).
Discussion: Malnutrition significantly increases mortality, risk of SBP and sepsis, HE, HRS, myocardial infarction, and need for transfusions in HCC patients with GI bleeding. This underscores the importance of comprehensive nutritional assessment and optimization of nutritional status in these patients.
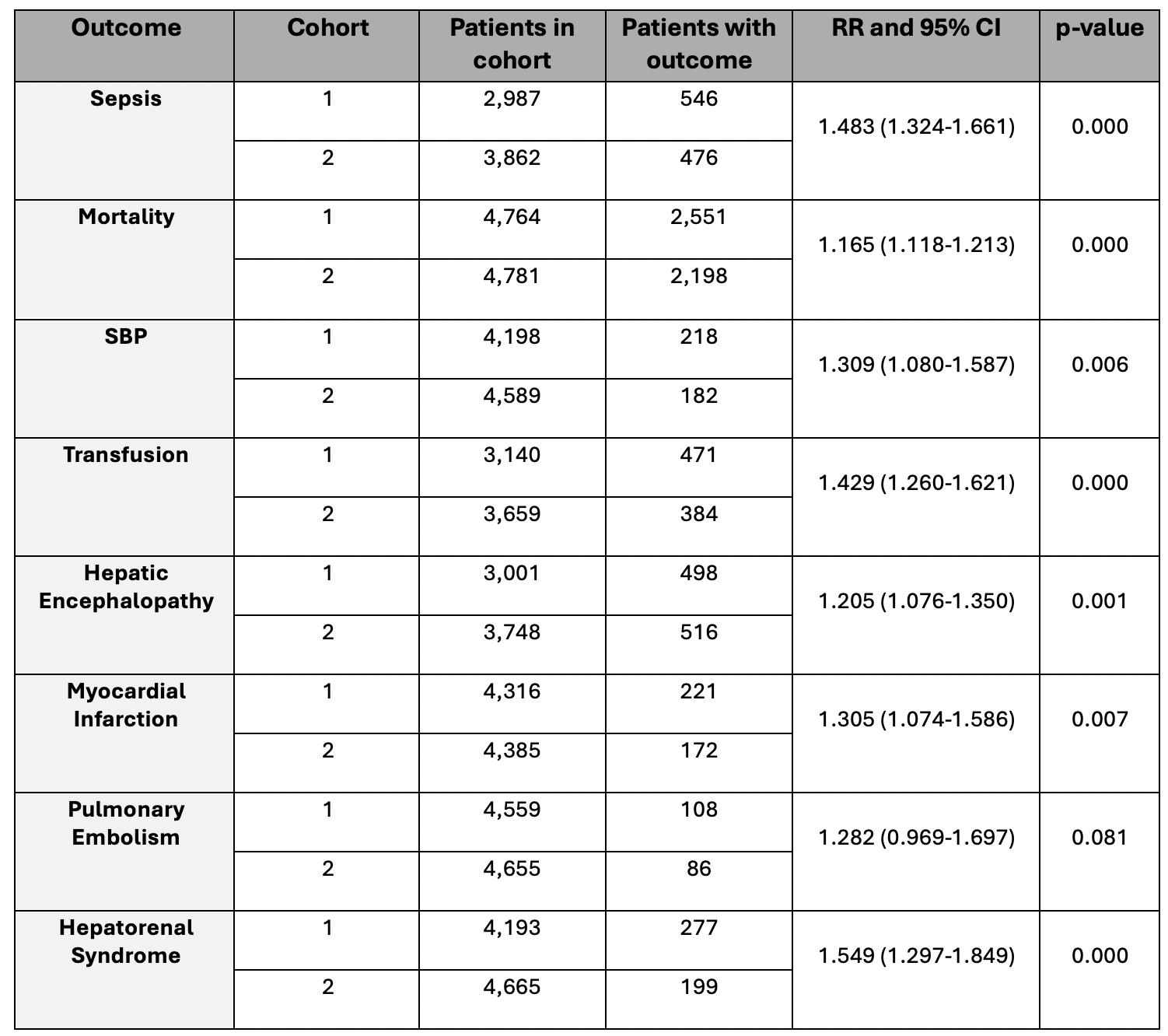
Figure: Table 1: Clinical Outcomes in Cohort 1 and Cohort 2 After Propensity Score Matching
Disclosures:
Kevin Robinson indicated no relevant financial relationships.
Colton Jones indicated no relevant financial relationships.
Warren Robinson indicated no relevant financial relationships.
Karecia Byfield indicated no relevant financial relationships.
Irhoboudu Atogwe indicated no relevant financial relationships.
Fnu Deepali indicated no relevant financial relationships.
Jabari Munroe indicated no relevant financial relationships.
Victor Navarro indicated no relevant financial relationships.
Kevin Robinson, MD1, Colton Jones, MD1, Warren Robinson, MBBS2, Karecia Byfield, MBBS1, Irhoboudu D. Atogwe, MD1, Fnu Deepali, MD1, Jabari Munroe, MD3, Victor Navarro, MD4. P5887 - Impact of Malnutrition on Clinical Outcomes in Hepatocellular Carcinoma Patients With Gastrointestinal Bleeding: A Propensity Score-Matched Population-Based Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
