Tuesday Poster Session
Category: Liver
P5884 - Cirrhosis and Cardiac Rhythm: Investigating the Impact of Cirrhosis on Atrial Fibrillation-Related Mortality in the United States
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Islam Rajab, MD
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Islam Rajab, MD1, Abdalhakim Shubietah, MD2, Ahmed Abuhasna, DO2, Mohammad Ghannam, MD3, Hamid U.. Rahman, MD2, Mohamed S. Elgendy, MBBCh4, Mohammad Alqadi, MD5, Mohammad O. Abdelhafez, MD6, Qutaiba Qafisheh, MD5, Muath A. Baniowda, MD7, Abdallah Hussein, MD8, Hosam I. Taha, MBBCh4, Ameer Awashra, MD9, Emmanuel Olumuyide, MD2, Walid Baddoura, MD1
1St. Joseph's University Medical Center, Paterson, NJ; 2Advocate Illinois Masonic Medical Center, Chicago, IL; 3Brookdale University Hospital Medical Center, New York, NY; 4Tanta University, Tanta, Al Gharbiyah, Egypt; 5University of Toledo, Toledo, OH; 6Al-Quds University, Jerusalem, Palestinian Territories; 7University of Missouri Kansas City School of Medicine, Kansas City, MO; 8Virtua Our Lady of Lourdes Hospital, Camden, NJ; 9An-Najah National University, Nablus, Palestinian Territories
Introduction: Cirrhosis promotes atrial fibrillation (AF) through systemic inflammation, autonomic dysfunction, and volume shifts associated with portal hypertension. While these mechanisms suggest a heightened cardiovascular risk, the impact of cirrhosis on AF-related mortality remains unclear.
Methods: Retrospective analysis of CDC WONDER data (1999–2020) identified AF (ICD‑10 I48) as the underlying cause, with cirrhosis (ICD‑10 K70.2–K76.7, I85–I86.4) as a contributing cause. We calculated age‑adjusted mortality rates (AAMRs; direct method; 2000 U.S. standard; 11 strata) and crude mortality rates per 100,000, stratified by year, sex, race/Hispanic origin, age group, place of death, urbanization (2013 NCHS), and state, applying CDC suppression rules for confidentiality.
Results: Between 1999 and 2020, AF-related mortality among cirrhotic decedents rose markedly, corresponding to an APC of 9.65% per year (1999–2020; 95% CI 8.40–11.87; p < 0.000001). Sex-stratified analyses showed APCs of 9.16% (95% CI 7.76–11.54; p < 0.000001) in males and 9.58% (95% CI 8.28–11.58; p < 0.000001) in females; the overall AAMR was 0.0447 per 100,000 in males and 0.0218 per 100,000 in females. By race, White decedents experienced an APC of 9.23% per year (1999–2020; 95% CI 7.93–11.43; p < 0.000001) and an AAMR of 0.0365, while Black AAMRs peaked at 0.0472 in 2019 before declining to 0.0361 in 2020. American Indian/Alaska Native and Asian/Pacific Islander decedents exhibited AAMRs of 0.0361 and 0.0233, respectively. Hispanic decedents had an AAMR of 0.0294 versus 0.0278 in non-Hispanics. State AAMRs varied from 0.0113 (LA) to 0.0649 (OR), and urban rates from 0.0218 (large central metros) to 0.0431 (small metros). Inpatient and at-home deaths comprised 49.0% and 23.7%, respectively. Crude mortality rose with age, from 0.0102 (45–54 years) to 0.463 (≥ 85 years).
Discussion: AF-related mortality in cirrhotic decedents rose 9.65% annually from 1999–2020—far exceeding the 3–5% increase seen in the general population—and suggests a contribution from cirrhosis-driven hemodynamic and inflammatory changes. APCs were similar by sex despite higher male AAMRs. Steeper increases in White versus more variable trends in Black patients, higher rates in small metros and states like Oregon, and a predominance of inpatient (49.0%) and at home (23.7%) deaths point to disparities in detection, care access, and regional cirrhosis etiologies, while age-related rises reflect demographic shifts in AF and cirrhosis prevalence.
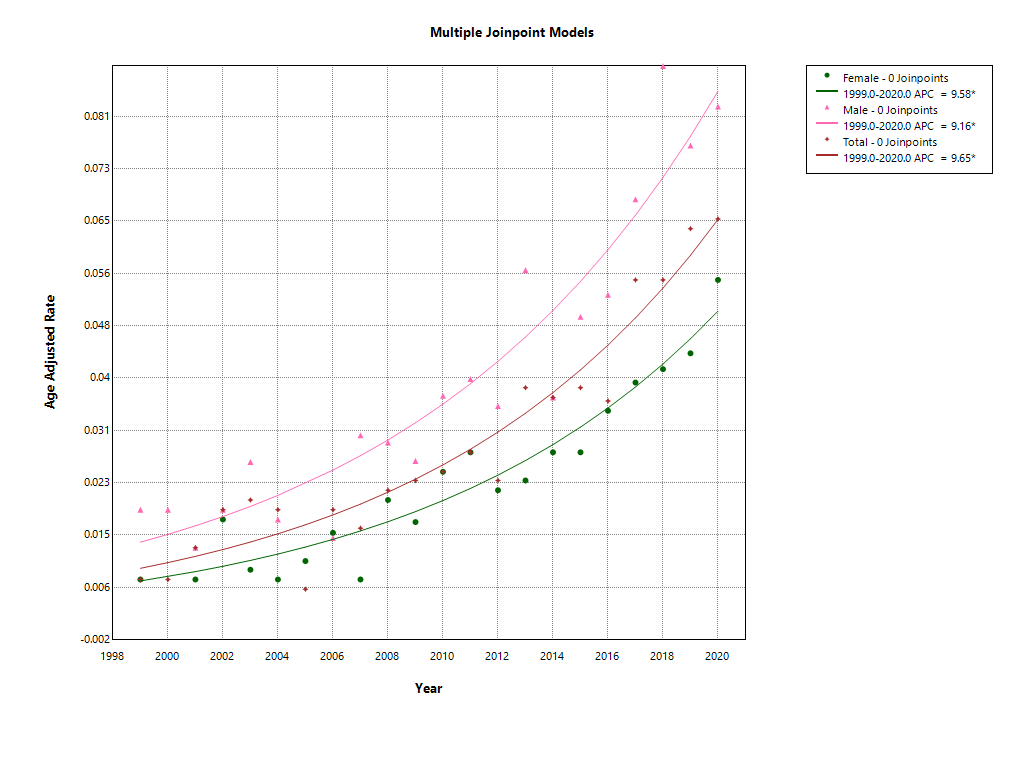
Figure: Figure 1. Age-adjusted AF mortality rates per 100,000 in cirrhotic decedents (1999–2020) by sex and overall (APCs: total 9.65%, male 9.16%, female 9.58%).
Disclosures:
Islam Rajab indicated no relevant financial relationships.
Abdalhakim Shubietah indicated no relevant financial relationships.
Ahmed Abuhasna indicated no relevant financial relationships.
Mohammad Ghannam indicated no relevant financial relationships.
Hamid Rahman indicated no relevant financial relationships.
Mohamed S. Elgendy indicated no relevant financial relationships.
Mohammad Alqadi indicated no relevant financial relationships.
Mohammad O. Abdelhafez indicated no relevant financial relationships.
Qutaiba Qafisheh indicated no relevant financial relationships.
Muath A. Baniowda indicated no relevant financial relationships.
Abdallah Hussein indicated no relevant financial relationships.
Hosam I. Taha indicated no relevant financial relationships.
Ameer Awashra indicated no relevant financial relationships.
Emmanuel Olumuyide indicated no relevant financial relationships.
Walid Baddoura indicated no relevant financial relationships.
Islam Rajab, MD1, Abdalhakim Shubietah, MD2, Ahmed Abuhasna, DO2, Mohammad Ghannam, MD3, Hamid U.. Rahman, MD2, Mohamed S. Elgendy, MBBCh4, Mohammad Alqadi, MD5, Mohammad O. Abdelhafez, MD6, Qutaiba Qafisheh, MD5, Muath A. Baniowda, MD7, Abdallah Hussein, MD8, Hosam I. Taha, MBBCh4, Ameer Awashra, MD9, Emmanuel Olumuyide, MD2, Walid Baddoura, MD1. P5884 - Cirrhosis and Cardiac Rhythm: Investigating the Impact of Cirrhosis on Atrial Fibrillation-Related Mortality in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2Advocate Illinois Masonic Medical Center, Chicago, IL; 3Brookdale University Hospital Medical Center, New York, NY; 4Tanta University, Tanta, Al Gharbiyah, Egypt; 5University of Toledo, Toledo, OH; 6Al-Quds University, Jerusalem, Palestinian Territories; 7University of Missouri Kansas City School of Medicine, Kansas City, MO; 8Virtua Our Lady of Lourdes Hospital, Camden, NJ; 9An-Najah National University, Nablus, Palestinian Territories
Introduction: Cirrhosis promotes atrial fibrillation (AF) through systemic inflammation, autonomic dysfunction, and volume shifts associated with portal hypertension. While these mechanisms suggest a heightened cardiovascular risk, the impact of cirrhosis on AF-related mortality remains unclear.
Methods: Retrospective analysis of CDC WONDER data (1999–2020) identified AF (ICD‑10 I48) as the underlying cause, with cirrhosis (ICD‑10 K70.2–K76.7, I85–I86.4) as a contributing cause. We calculated age‑adjusted mortality rates (AAMRs; direct method; 2000 U.S. standard; 11 strata) and crude mortality rates per 100,000, stratified by year, sex, race/Hispanic origin, age group, place of death, urbanization (2013 NCHS), and state, applying CDC suppression rules for confidentiality.
Results: Between 1999 and 2020, AF-related mortality among cirrhotic decedents rose markedly, corresponding to an APC of 9.65% per year (1999–2020; 95% CI 8.40–11.87; p < 0.000001). Sex-stratified analyses showed APCs of 9.16% (95% CI 7.76–11.54; p < 0.000001) in males and 9.58% (95% CI 8.28–11.58; p < 0.000001) in females; the overall AAMR was 0.0447 per 100,000 in males and 0.0218 per 100,000 in females. By race, White decedents experienced an APC of 9.23% per year (1999–2020; 95% CI 7.93–11.43; p < 0.000001) and an AAMR of 0.0365, while Black AAMRs peaked at 0.0472 in 2019 before declining to 0.0361 in 2020. American Indian/Alaska Native and Asian/Pacific Islander decedents exhibited AAMRs of 0.0361 and 0.0233, respectively. Hispanic decedents had an AAMR of 0.0294 versus 0.0278 in non-Hispanics. State AAMRs varied from 0.0113 (LA) to 0.0649 (OR), and urban rates from 0.0218 (large central metros) to 0.0431 (small metros). Inpatient and at-home deaths comprised 49.0% and 23.7%, respectively. Crude mortality rose with age, from 0.0102 (45–54 years) to 0.463 (≥ 85 years).
Discussion: AF-related mortality in cirrhotic decedents rose 9.65% annually from 1999–2020—far exceeding the 3–5% increase seen in the general population—and suggests a contribution from cirrhosis-driven hemodynamic and inflammatory changes. APCs were similar by sex despite higher male AAMRs. Steeper increases in White versus more variable trends in Black patients, higher rates in small metros and states like Oregon, and a predominance of inpatient (49.0%) and at home (23.7%) deaths point to disparities in detection, care access, and regional cirrhosis etiologies, while age-related rises reflect demographic shifts in AF and cirrhosis prevalence.
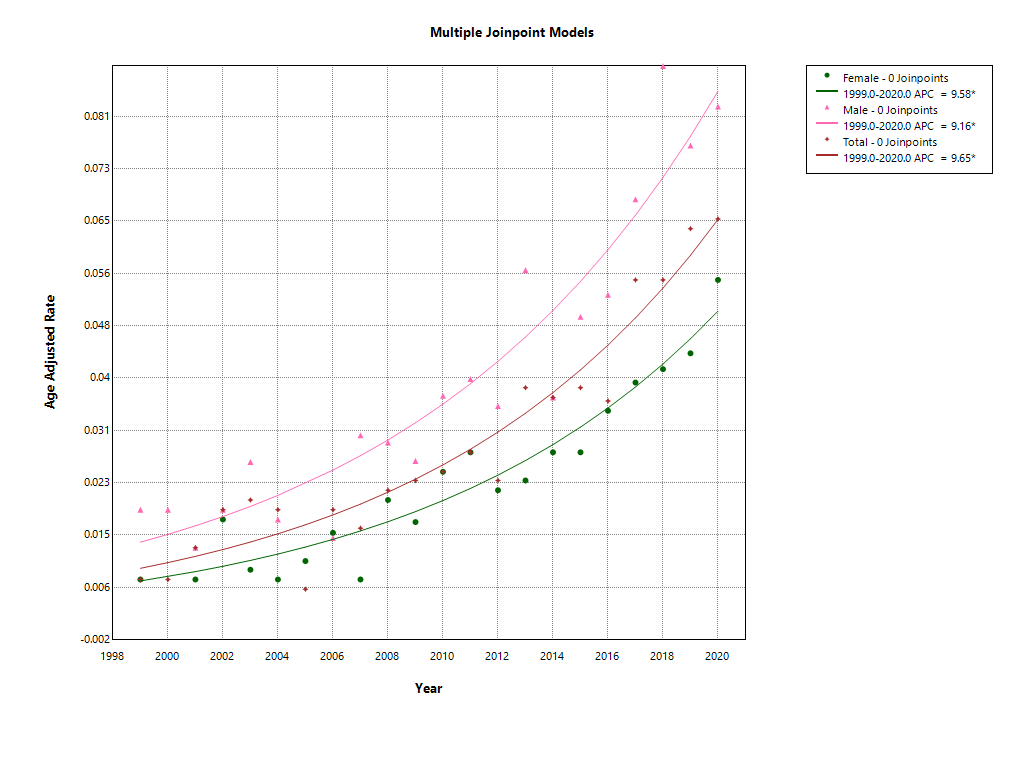
Figure: Figure 1. Age-adjusted AF mortality rates per 100,000 in cirrhotic decedents (1999–2020) by sex and overall (APCs: total 9.65%, male 9.16%, female 9.58%).
Disclosures:
Islam Rajab indicated no relevant financial relationships.
Abdalhakim Shubietah indicated no relevant financial relationships.
Ahmed Abuhasna indicated no relevant financial relationships.
Mohammad Ghannam indicated no relevant financial relationships.
Hamid Rahman indicated no relevant financial relationships.
Mohamed S. Elgendy indicated no relevant financial relationships.
Mohammad Alqadi indicated no relevant financial relationships.
Mohammad O. Abdelhafez indicated no relevant financial relationships.
Qutaiba Qafisheh indicated no relevant financial relationships.
Muath A. Baniowda indicated no relevant financial relationships.
Abdallah Hussein indicated no relevant financial relationships.
Hosam I. Taha indicated no relevant financial relationships.
Ameer Awashra indicated no relevant financial relationships.
Emmanuel Olumuyide indicated no relevant financial relationships.
Walid Baddoura indicated no relevant financial relationships.
Islam Rajab, MD1, Abdalhakim Shubietah, MD2, Ahmed Abuhasna, DO2, Mohammad Ghannam, MD3, Hamid U.. Rahman, MD2, Mohamed S. Elgendy, MBBCh4, Mohammad Alqadi, MD5, Mohammad O. Abdelhafez, MD6, Qutaiba Qafisheh, MD5, Muath A. Baniowda, MD7, Abdallah Hussein, MD8, Hosam I. Taha, MBBCh4, Ameer Awashra, MD9, Emmanuel Olumuyide, MD2, Walid Baddoura, MD1. P5884 - Cirrhosis and Cardiac Rhythm: Investigating the Impact of Cirrhosis on Atrial Fibrillation-Related Mortality in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
