Tuesday Poster Session
Category: Liver
P5880 - From Fatty Liver to Fewer Tumors: GI Cancer Risk in MASLD After Bariatric Surgery
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MK
Meghana Kakarla, MD
Infirmary Health
Mobile, AL
Presenting Author(s)
Meghana Kakarla, MD1, Giovannie Isaac-Coss, MD2, Ashvath Pillai, 3, Nancy Reau, MD, FACG2
1Infirmary Health, Mobile, AL; 2Rush University Medical Center, Chicago, IL; 3SSPM Medical College and Lifetime Hospital, Navi Mumbai, Maharashtra, India
Introduction: MASLD affects ~25% of adults globally and is increasingly linked to GI and liver cancers. In obese MASLD patients, evidence shows bariatric surgery improves liver histology and metabolism, but long-term cancer risk remains unclear. This study used national data to assess post-surgical cancer risk in this high-risk metabolic group.
Methods: We conducted a retrospective cross-sectional analysis of the National Inpatient Sample (2018–2021), identifying MASLD via ICD-10 codes (K76.0, K75.81). Bariatric surgery history was defined by Z98.84 and Z98.89, excluding those who underwent bariatric procedures during index hospitalization. GI/hepatobiliary cancers were identified using ICD-10 codes (C22.0, C18, C25, C15, C16). Multivariable logistic regression adjusted for age, sex, obesity, diabetes, hypertension, insurance, and income. Survey weights and clustering generated national estimates. Subgroup analysis was stratified by cancer type.
Results: Of 454,054 MASLD hospital admissions from 2018–2021 included 11,602 patients (2.6%) who underwent bariatric surgery. The bariatric surgery group included more female patients (79.4% vs. 52.7%) and patients who were younger (mean age 52.5 vs. 56.0 years). Unadjusted analysis showed 52% lower odds of cancer in the bariatric group (OR 0.48, 95% CI: 0.40–0.58, p< 0.001), which remained significant after adjustment (aOR 0.72, 95% CI: 0.59–0.87, p=0.001). Subgroup analysis demonstrated significantly reduced odds of hepatocellular carcinoma (aOR 0.63, 95% CI: 0.45–0.89, p=0.008) and colon cancer (aOR 0.51, 95% CI: 0.34–0.79, p=0.002). No significant associations were observed for pancreatic (aOR 0.92, 95% CI: 0.59–1.43, p=0.70), esophageal (aOR 0.21, 95% CI: 0.03–1.19, p=0.08), or gastric cancers (aOR 1.42, 95% CI: 0.83–2.43, p=0.20).
Discussion: This national study of hospitalized MASLD patients found that prior bariatric surgery was associated with significantly reduced odds of gastrointestinal and hepatobiliary cancers—particularly hepatocellular (aOR 0.63) and colorectal cancer (aOR 0.51). These findings align with known metabolic benefits of surgery, including improved insulin sensitivity, reduced inflammation, and microbiome changes. No significant associations were seen for pancreatic, gastric, or esophageal cancers, suggesting organ-specific effects. While causality cannot be inferred due to the cross-sectional design, results support bariatric surgery as a potential cancer-modifying intervention in high-risk metabolic populations.
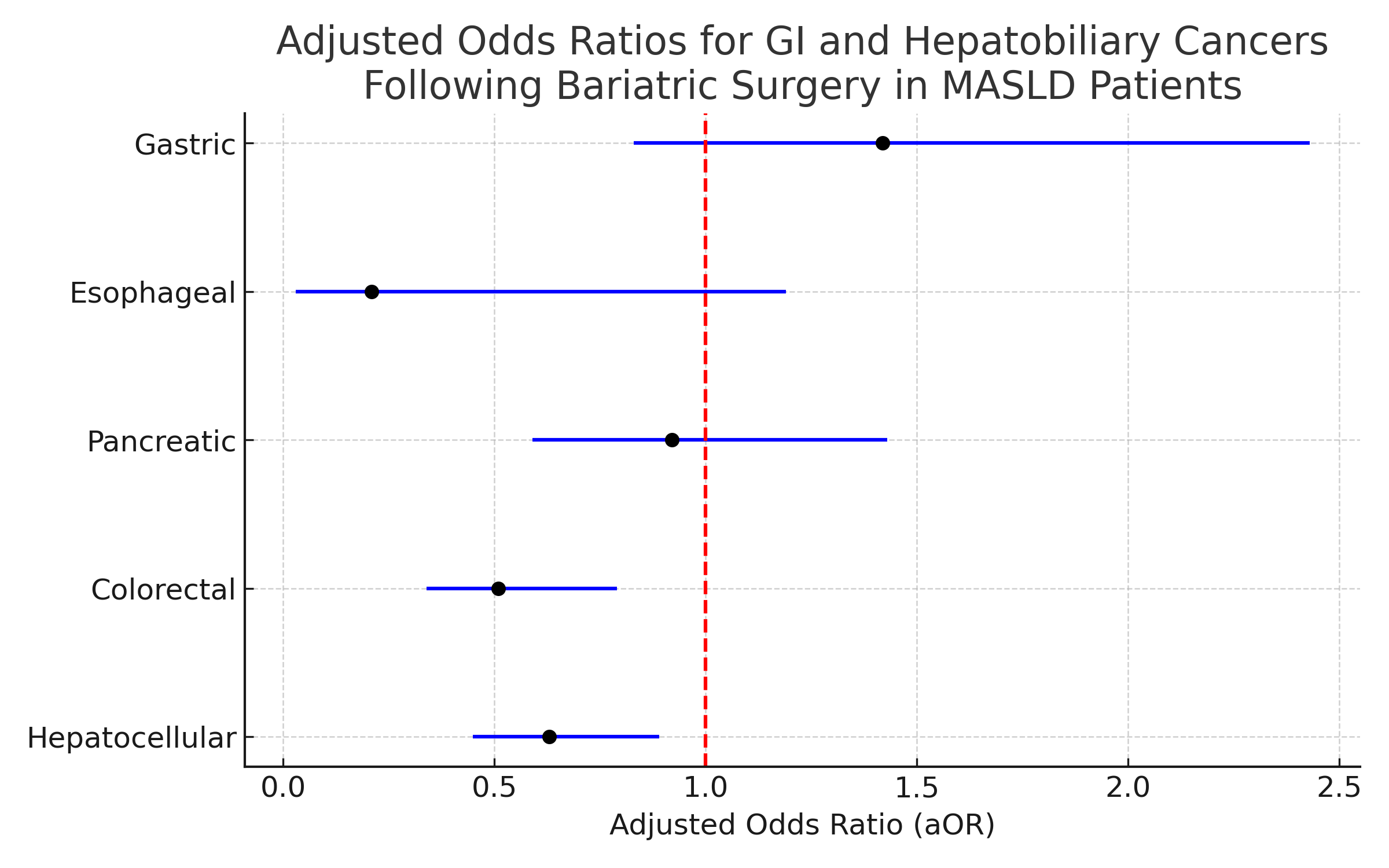
Figure: Forest plot of adjusted odds ratios (aOR) for gastrointestinal and hepatobiliary cancers in MASLD patients with prior bariatric surgery
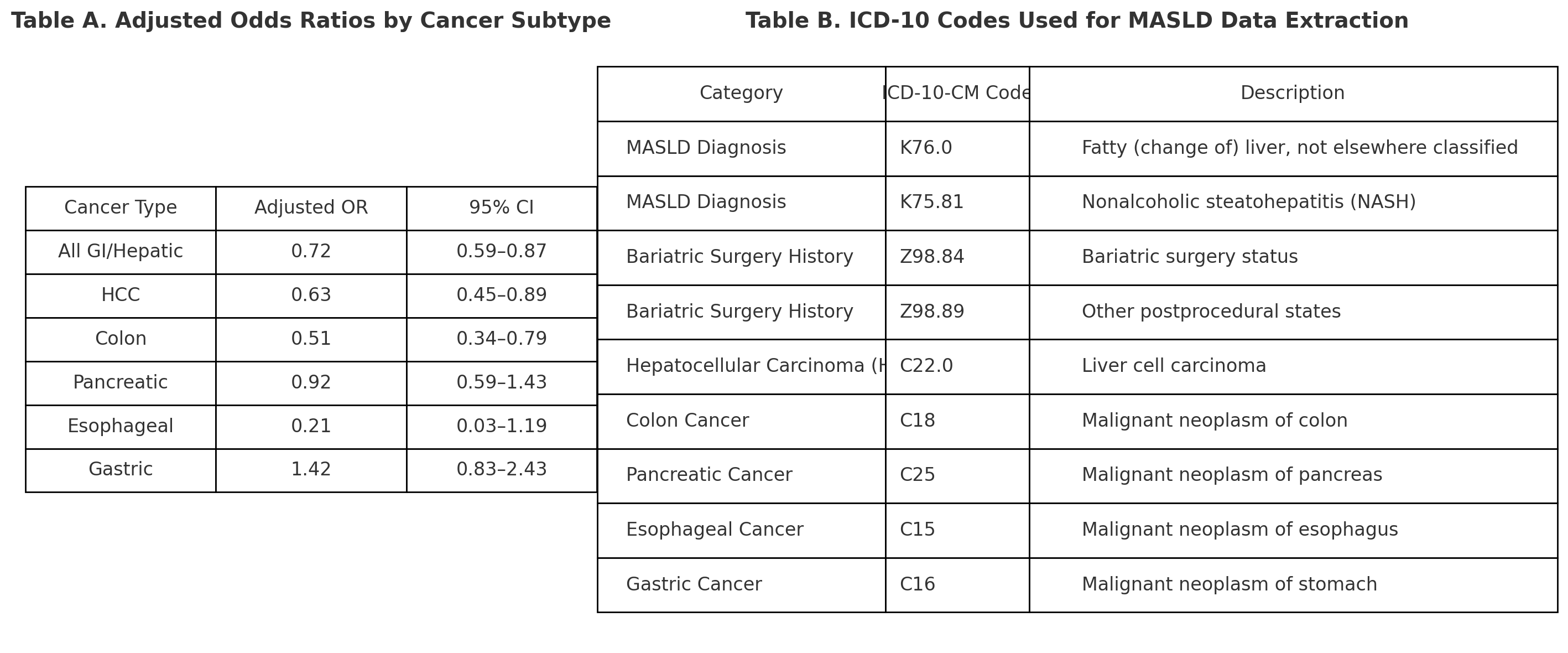
Figure: Table A: Adjusted cancer odds by subtype
Table B: ICD-10 codes used
Disclosures:
Meghana Kakarla indicated no relevant financial relationships.
Giovannie Isaac-Coss indicated no relevant financial relationships.
Ashvath Pillai indicated no relevant financial relationships.
Nancy Reau: AbbVie – Grant/Research Support. Arbutus – Advisor or Review Panel Member. Gilead – Advisory Committee/Board Member, Grant/Research Support. Salix – Advisory Committee/Board Member, Grant/Research Support. VIR – Advisory Committee/Board Member, Grant/Research Support.
Meghana Kakarla, MD1, Giovannie Isaac-Coss, MD2, Ashvath Pillai, 3, Nancy Reau, MD, FACG2. P5880 - From Fatty Liver to Fewer Tumors: GI Cancer Risk in MASLD After Bariatric Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Infirmary Health, Mobile, AL; 2Rush University Medical Center, Chicago, IL; 3SSPM Medical College and Lifetime Hospital, Navi Mumbai, Maharashtra, India
Introduction: MASLD affects ~25% of adults globally and is increasingly linked to GI and liver cancers. In obese MASLD patients, evidence shows bariatric surgery improves liver histology and metabolism, but long-term cancer risk remains unclear. This study used national data to assess post-surgical cancer risk in this high-risk metabolic group.
Methods: We conducted a retrospective cross-sectional analysis of the National Inpatient Sample (2018–2021), identifying MASLD via ICD-10 codes (K76.0, K75.81). Bariatric surgery history was defined by Z98.84 and Z98.89, excluding those who underwent bariatric procedures during index hospitalization. GI/hepatobiliary cancers were identified using ICD-10 codes (C22.0, C18, C25, C15, C16). Multivariable logistic regression adjusted for age, sex, obesity, diabetes, hypertension, insurance, and income. Survey weights and clustering generated national estimates. Subgroup analysis was stratified by cancer type.
Results: Of 454,054 MASLD hospital admissions from 2018–2021 included 11,602 patients (2.6%) who underwent bariatric surgery. The bariatric surgery group included more female patients (79.4% vs. 52.7%) and patients who were younger (mean age 52.5 vs. 56.0 years). Unadjusted analysis showed 52% lower odds of cancer in the bariatric group (OR 0.48, 95% CI: 0.40–0.58, p< 0.001), which remained significant after adjustment (aOR 0.72, 95% CI: 0.59–0.87, p=0.001). Subgroup analysis demonstrated significantly reduced odds of hepatocellular carcinoma (aOR 0.63, 95% CI: 0.45–0.89, p=0.008) and colon cancer (aOR 0.51, 95% CI: 0.34–0.79, p=0.002). No significant associations were observed for pancreatic (aOR 0.92, 95% CI: 0.59–1.43, p=0.70), esophageal (aOR 0.21, 95% CI: 0.03–1.19, p=0.08), or gastric cancers (aOR 1.42, 95% CI: 0.83–2.43, p=0.20).
Discussion: This national study of hospitalized MASLD patients found that prior bariatric surgery was associated with significantly reduced odds of gastrointestinal and hepatobiliary cancers—particularly hepatocellular (aOR 0.63) and colorectal cancer (aOR 0.51). These findings align with known metabolic benefits of surgery, including improved insulin sensitivity, reduced inflammation, and microbiome changes. No significant associations were seen for pancreatic, gastric, or esophageal cancers, suggesting organ-specific effects. While causality cannot be inferred due to the cross-sectional design, results support bariatric surgery as a potential cancer-modifying intervention in high-risk metabolic populations.
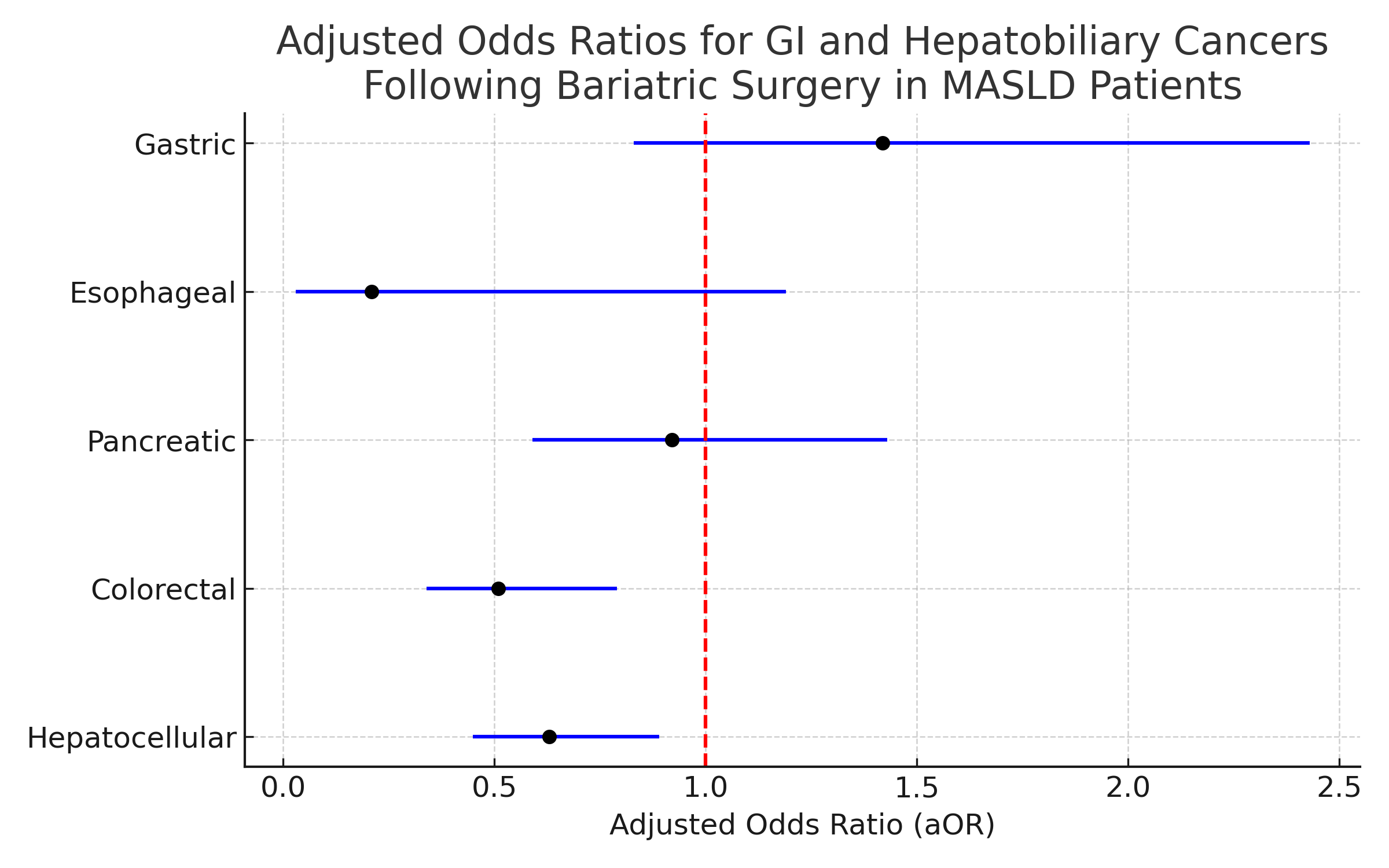
Figure: Forest plot of adjusted odds ratios (aOR) for gastrointestinal and hepatobiliary cancers in MASLD patients with prior bariatric surgery
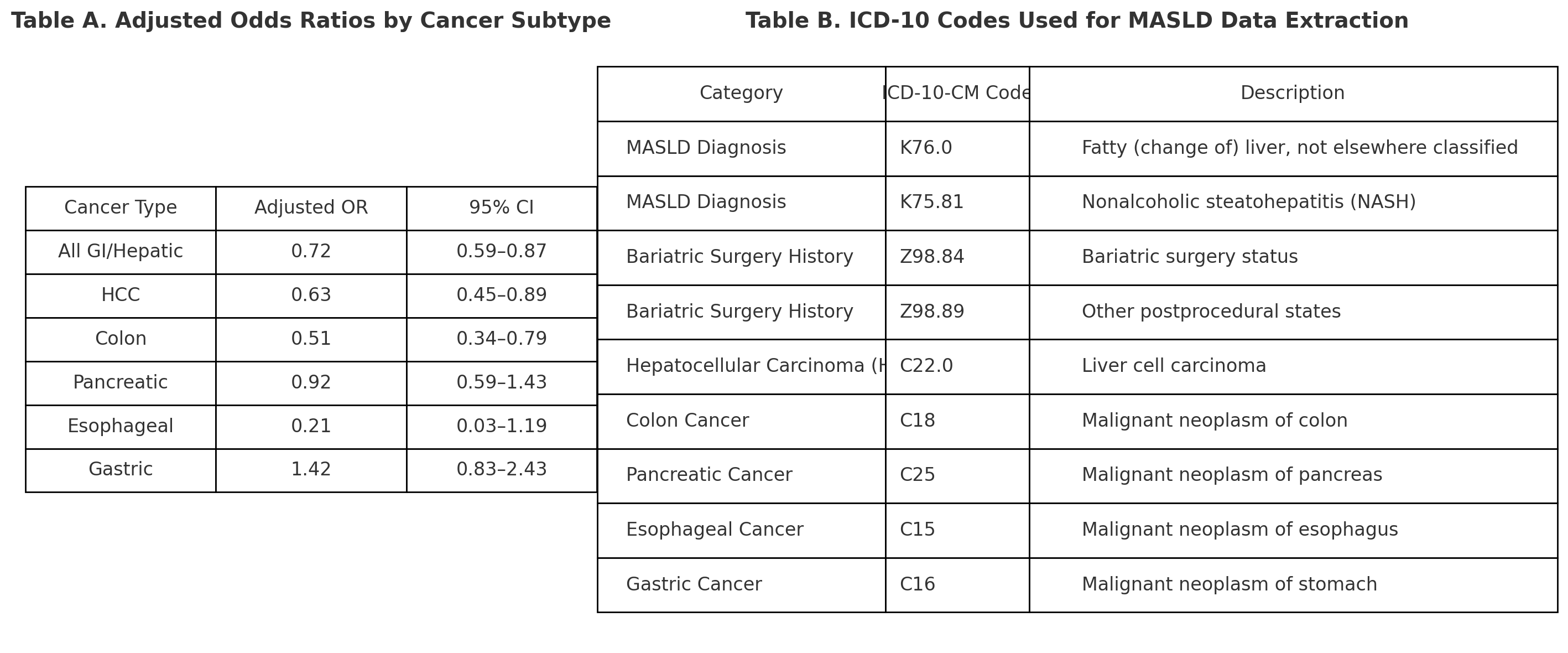
Figure: Table A: Adjusted cancer odds by subtype
Table B: ICD-10 codes used
Disclosures:
Meghana Kakarla indicated no relevant financial relationships.
Giovannie Isaac-Coss indicated no relevant financial relationships.
Ashvath Pillai indicated no relevant financial relationships.
Nancy Reau: AbbVie – Grant/Research Support. Arbutus – Advisor or Review Panel Member. Gilead – Advisory Committee/Board Member, Grant/Research Support. Salix – Advisory Committee/Board Member, Grant/Research Support. VIR – Advisory Committee/Board Member, Grant/Research Support.
Meghana Kakarla, MD1, Giovannie Isaac-Coss, MD2, Ashvath Pillai, 3, Nancy Reau, MD, FACG2. P5880 - From Fatty Liver to Fewer Tumors: GI Cancer Risk in MASLD After Bariatric Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
