Tuesday Poster Session
Category: Liver
P5950 - Trends and Predictors of In-Hospital Mortality in Acute-on-Chronic Liver Failure: A Nationwide Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mansi Mody, MBBS (she/her/hers)
M.P. Shah Government Medical College
Bharuch, Gujarat, India
Presenting Author(s)
Mansi Mody, MBBS1, Apoorva Doshi, MD2, Vishal Doshi, MBBS3, Sushrut Ingawale, MD4, Jenish Patel, MBBS5
1M.P. Shah Government Medical College, Bharuch, Gujarat, India; 2Jacobi Medical Center, New York City, NY; 3Seth Gordhandas Sundardas Medical College and KEM Hospital, Bharuch, Gujarat, India; 4Quinnipiac University - Frank H. Netter, MD School of Medicine / St. Vincent's Medical Center, Bridgeport, CT; 5M . P . Shah Government Medical College, Surat, Gujarat, India
Introduction: Acute-on-chronic liver failure (ACLF) is a serious complication of chronic liver disease, characterized by acute decompensation and multi-organ failure. Despite its rising prevalence in recent years, recent data on hospitalization outcomes for ACLF remain limited.
Methods: Using the Nationwide Inpatient Sample (2016–2020), we identified hospitalized patients aged ≥18 years with ACLF based on the North American Consortium for the Study of End-Stage Liver Disease criteria, defined as cirrhosis with ≥2 organ failures (respiratory failure requiring mechanical ventilation, shock, grade ≥3 hepatic encephalopathy, or renal failure requiring dialysis or replacement therapy).
Our primary outcome was in-hospital mortality (IHM). We used the Cochrane-Armitage test to assess overall and etiology-specific trends in IHM. Additionally, survey-weighted multivariable logistic regression was conducted to identify predictors of IHM, including etiology, demographic characteristics, and comorbidity burden (Charlson Comorbidity Index [CCI]), with hospital characteristics included as covariates.
Results: We analyzed a total of 32,311 ACLF adult hospitalizations, with mean age 58 (SD, ± 12) years, 61% male and 62% non-Hispanic White, 43% Medicare beneficiaries, and 52% having alcoholic liver disease (ALD) as the underlying etiology (Table 1). The overall IHM rate was 50.3%. Although ACLF related to viral hepatitis had the highest IHM (51.6%), the differences in mortality across etiologies were not statistically significant.
The overall IHM rate increased significantly from 2016 to 2020, with the most notable rise occurring between 2019-2020 (48.2% to 51.6%). A similar trend was observed in ALD (47.7% to 50%, p < 0.05). Notably, the greatest increase in IHM occurred among patients with ACLF due to other etiologies (50.7% in 2016 to 55.2% in 2020; p < .001) (Figure 1.A).
After multivariable adjustment, ALD (OR 1.61 [95% CI: 1.56–1.67]), other etiologies (OR 1.23[1.18–1.13]), CCI 4–6 (OR 1.35[1.30–1.39]), CCI ≥7 (OR 1.75[1.69–1.81]), AA race (OR 1.07[1.03–1.11]), and no insurance (OR 1.16[1.09–1.22]) were significantly associated with increased odds of IHM among ACLF admissions (Figure 1.B).
Discussion: We report a rising trend in IHM among ACLF admissions in the US, particularly in ALD and ACLF due to other etiologies. Additionally, AA race, lack of insurance, ALD, other etiologies, and a high comorbidity burden were associated with higher odds of IHM, underscoring the urgent need to address these disparities.
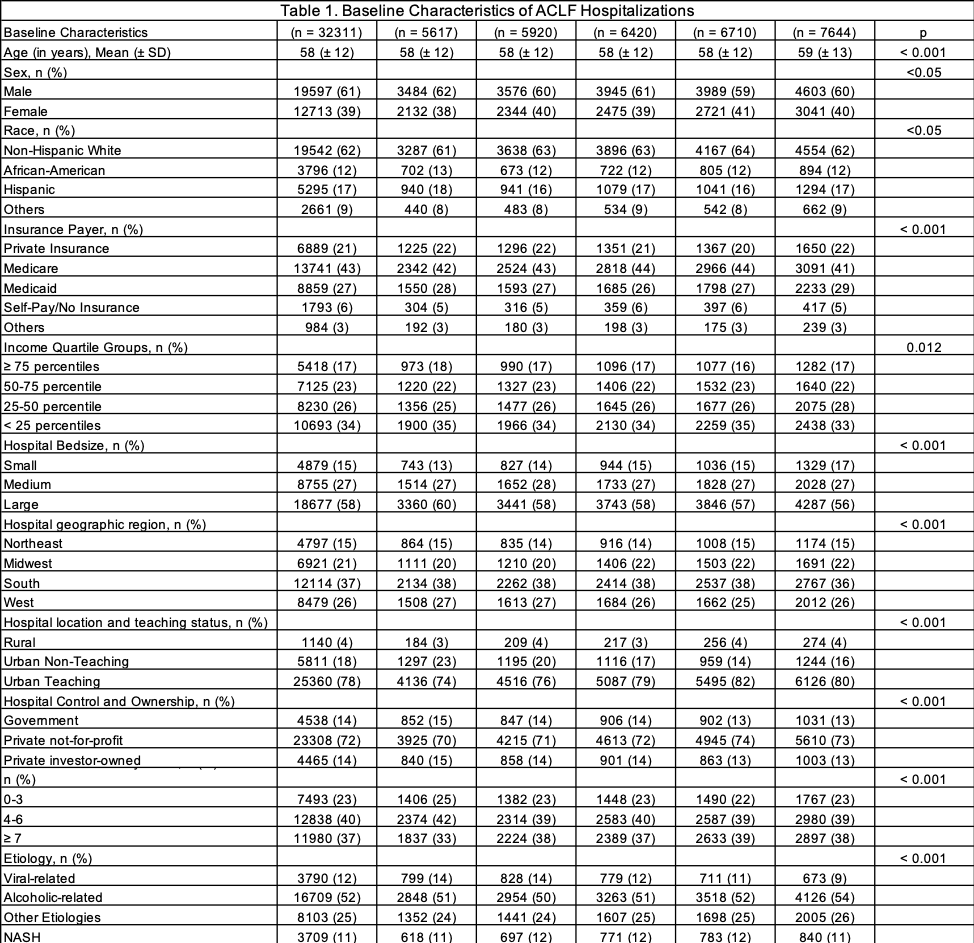
Figure: Table 1. Baseline Characteristics of ACLF Hospitalizations
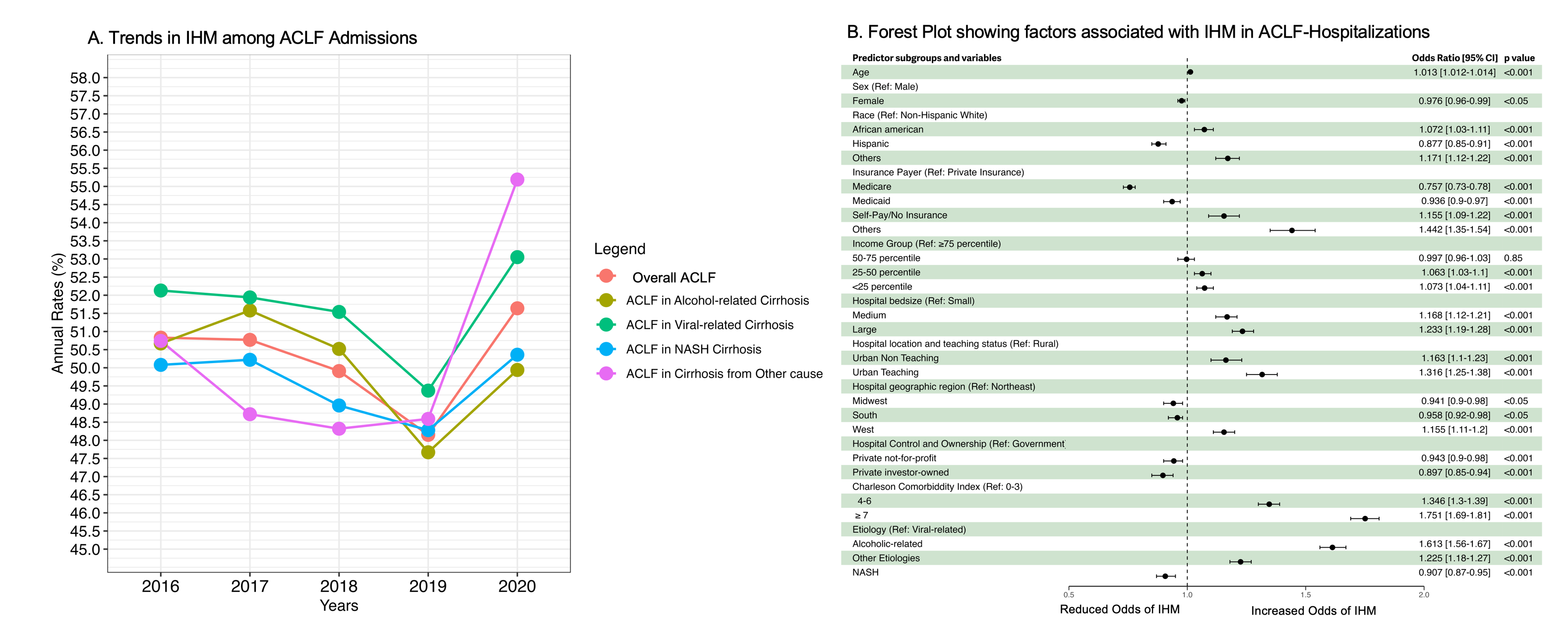
Figure: Figure 1. A: Trends in IHM among ACLF Admissions. B: Forest Plot showing factors associated with IHM in ACLF-Hospitalizations.
Disclosures:
Mansi Mody indicated no relevant financial relationships.
Apoorva Doshi indicated no relevant financial relationships.
Vishal Doshi indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Jenish Patel indicated no relevant financial relationships.
Mansi Mody, MBBS1, Apoorva Doshi, MD2, Vishal Doshi, MBBS3, Sushrut Ingawale, MD4, Jenish Patel, MBBS5. P5950 - Trends and Predictors of In-Hospital Mortality in Acute-on-Chronic Liver Failure: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1M.P. Shah Government Medical College, Bharuch, Gujarat, India; 2Jacobi Medical Center, New York City, NY; 3Seth Gordhandas Sundardas Medical College and KEM Hospital, Bharuch, Gujarat, India; 4Quinnipiac University - Frank H. Netter, MD School of Medicine / St. Vincent's Medical Center, Bridgeport, CT; 5M . P . Shah Government Medical College, Surat, Gujarat, India
Introduction: Acute-on-chronic liver failure (ACLF) is a serious complication of chronic liver disease, characterized by acute decompensation and multi-organ failure. Despite its rising prevalence in recent years, recent data on hospitalization outcomes for ACLF remain limited.
Methods: Using the Nationwide Inpatient Sample (2016–2020), we identified hospitalized patients aged ≥18 years with ACLF based on the North American Consortium for the Study of End-Stage Liver Disease criteria, defined as cirrhosis with ≥2 organ failures (respiratory failure requiring mechanical ventilation, shock, grade ≥3 hepatic encephalopathy, or renal failure requiring dialysis or replacement therapy).
Our primary outcome was in-hospital mortality (IHM). We used the Cochrane-Armitage test to assess overall and etiology-specific trends in IHM. Additionally, survey-weighted multivariable logistic regression was conducted to identify predictors of IHM, including etiology, demographic characteristics, and comorbidity burden (Charlson Comorbidity Index [CCI]), with hospital characteristics included as covariates.
Results: We analyzed a total of 32,311 ACLF adult hospitalizations, with mean age 58 (SD, ± 12) years, 61% male and 62% non-Hispanic White, 43% Medicare beneficiaries, and 52% having alcoholic liver disease (ALD) as the underlying etiology (Table 1). The overall IHM rate was 50.3%. Although ACLF related to viral hepatitis had the highest IHM (51.6%), the differences in mortality across etiologies were not statistically significant.
The overall IHM rate increased significantly from 2016 to 2020, with the most notable rise occurring between 2019-2020 (48.2% to 51.6%). A similar trend was observed in ALD (47.7% to 50%, p < 0.05). Notably, the greatest increase in IHM occurred among patients with ACLF due to other etiologies (50.7% in 2016 to 55.2% in 2020; p < .001) (Figure 1.A).
After multivariable adjustment, ALD (OR 1.61 [95% CI: 1.56–1.67]), other etiologies (OR 1.23[1.18–1.13]), CCI 4–6 (OR 1.35[1.30–1.39]), CCI ≥7 (OR 1.75[1.69–1.81]), AA race (OR 1.07[1.03–1.11]), and no insurance (OR 1.16[1.09–1.22]) were significantly associated with increased odds of IHM among ACLF admissions (Figure 1.B).
Discussion: We report a rising trend in IHM among ACLF admissions in the US, particularly in ALD and ACLF due to other etiologies. Additionally, AA race, lack of insurance, ALD, other etiologies, and a high comorbidity burden were associated with higher odds of IHM, underscoring the urgent need to address these disparities.
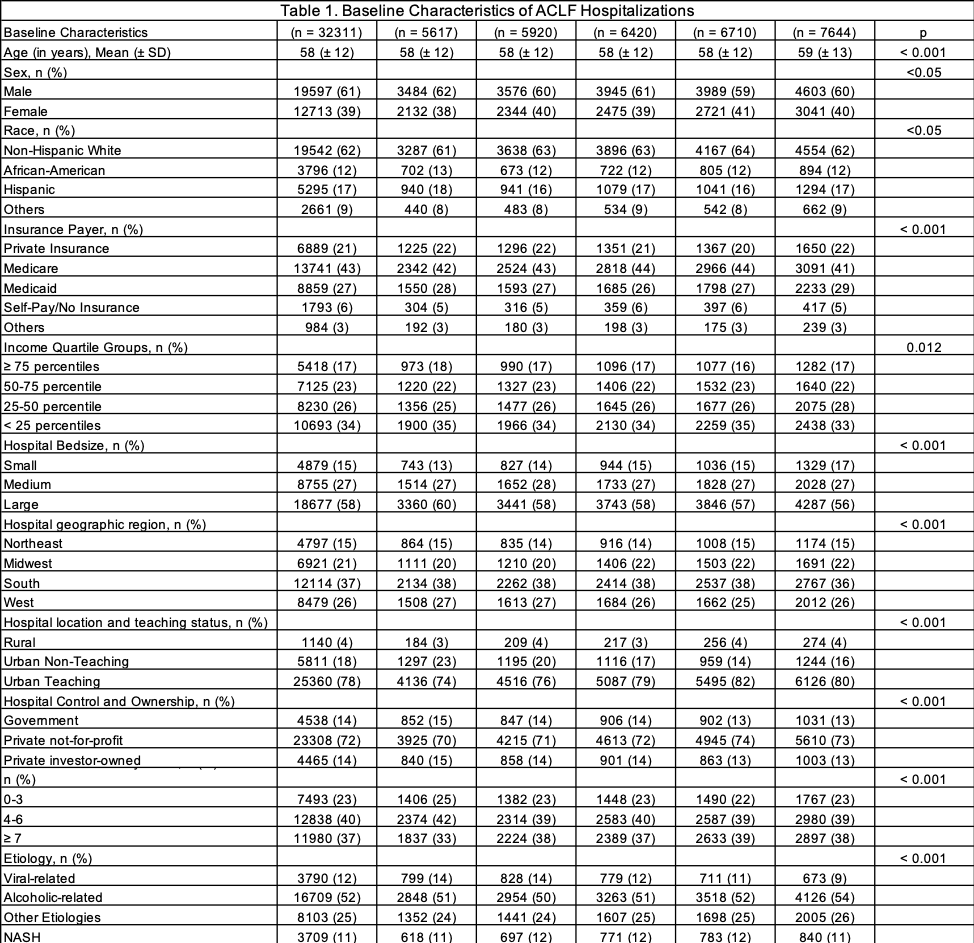
Figure: Table 1. Baseline Characteristics of ACLF Hospitalizations
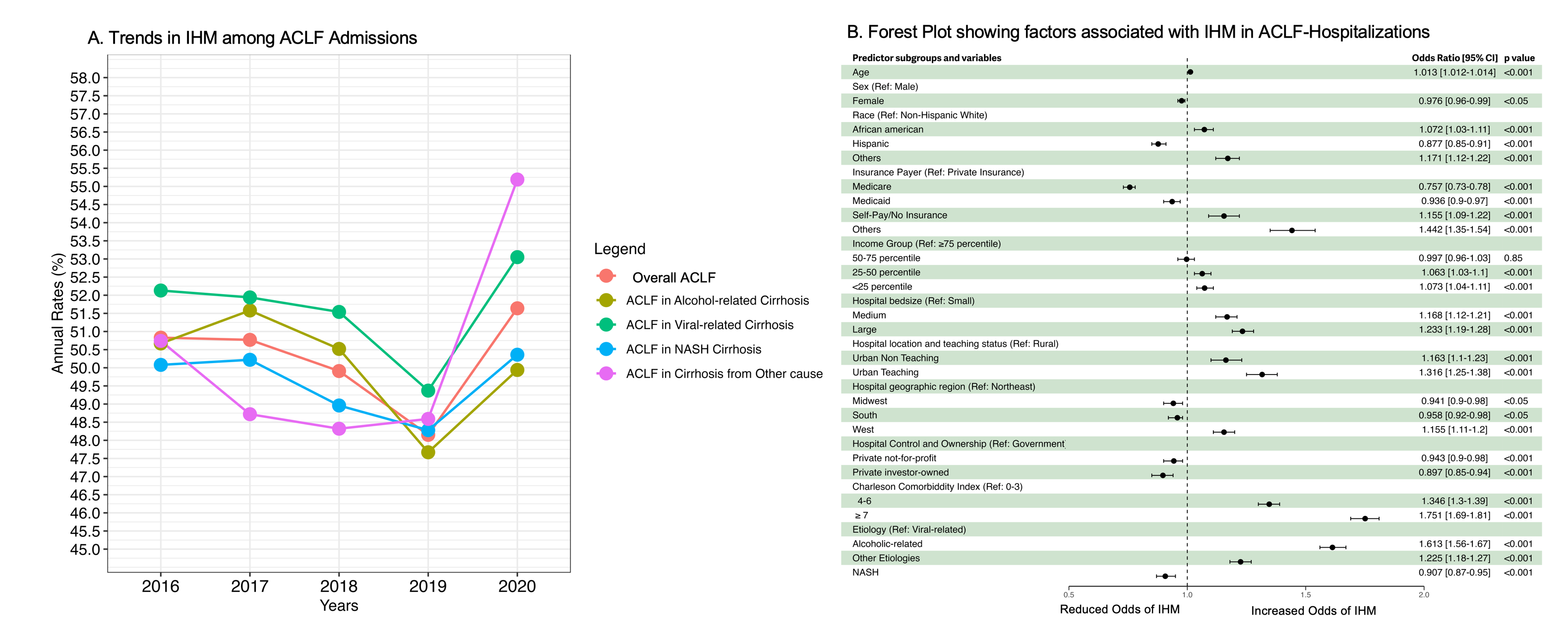
Figure: Figure 1. A: Trends in IHM among ACLF Admissions. B: Forest Plot showing factors associated with IHM in ACLF-Hospitalizations.
Disclosures:
Mansi Mody indicated no relevant financial relationships.
Apoorva Doshi indicated no relevant financial relationships.
Vishal Doshi indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Jenish Patel indicated no relevant financial relationships.
Mansi Mody, MBBS1, Apoorva Doshi, MD2, Vishal Doshi, MBBS3, Sushrut Ingawale, MD4, Jenish Patel, MBBS5. P5950 - Trends and Predictors of In-Hospital Mortality in Acute-on-Chronic Liver Failure: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
