Tuesday Poster Session
Category: Liver
P5944 - Porto-Sinusoidal Vascular Disease in End-Stage Kidney Disease: A Distinct Clinical Phenotype With Implications for Transplant Evaluation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alexander Imas, MD
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Alexander Imas, MD1, James Crismale, MD2, Thomas Schiano, MD3
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Hospital, New York, NY; 3Dept of Abdominal Transplantation Recanati/Miller Transplantation Institute/Division of Liver Diseases, Mt Sinai Hospital, NY, New York, NY
Introduction: Porto-sinusoidal vascular disease (PSVD) is a cause of non-cirrhotic portal hypertension defined by characteristic histology. Differentiating PSVD from cirrhosis is critical due to differences in prognosis and management. While several PSVD risk factors are known, the relationship between end-stage kidney disease (ESKD) requiring kidney replacement therapy and PSVD remains unclear. We aimed to assess the prevalence of ESKD among patients with biopsy-proven PSVD and compare clinical, histologic, and outcome features between those with and without ESKD.
Methods: We conducted a retrospective study of liver biopsies from 2011–2020 at a single center to identify patients with histologic features of PSVD. Those with ESKD on hemodialysis or peritoneal dialysis were matched by age and sex to PSVD controls without ESKD. Patients with evidence of other chronic liver diseases on biopsy or prior transplant were excluded. Clinical data, imaging, histology, portal hypertensive complications, mortality, and transplant outcomes were compared.
Results: Of 755 patients with PSVD histology, 51 (6.8%) had ESKD and were matched with 37 controls. ESKD patients were less often female (20% vs 59%, p< 0.01) and had more comorbidities (hypertension, diabetes, heart failure, HIV; all p< 0.01). A greater proportion had no PSVD risk factors aside from ESKD (51% vs 19%, p< 0.01). ESKD patients more frequently presented with ascites (43% vs 19%, p=0.052) and had ascites on imaging (70% vs 35%, p=0.002), while controls were more often referred for abnormal imaging or labs. Rates of varices and portal hypertensive bleeding were similar. Median HVPG did not differ (3.5 vs 4.5 mmHg, p=0.20). Over ~4.5 years of follow-up, new ascites developed more often in ESKD patients (18% vs 3%, p=0.03). Mortality was higher in the ESKD group (29% vs 3%, p< 0.01), driven by infection and respiratory failure, not portal hypertension. Five ESKD patients underwent kidney transplant after PSVD diagnosis with favorable outcomes.
Discussion: ESKD may be an underrecognized risk factor for PSVD, possibly linked to inflammation, hemodynamic shifts, or prothrombotic states. ESKD-associated PSVD shows a distinct clinical profile with more ascites but fewer classic portal hypertensive complications. Identifying PSVD in ESKD is critical, as it may support candidacy for kidney transplant alone, avoiding simultaneous liver-kidney transplantation.
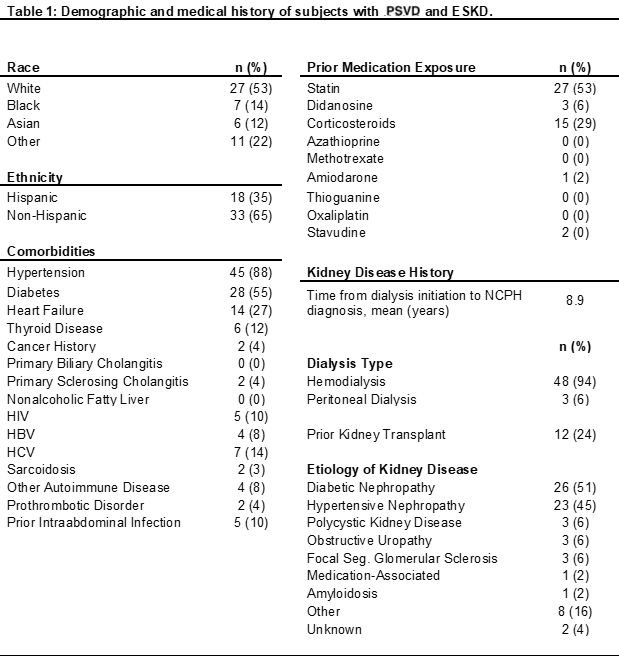
Figure: Demographic and medical history of subjects with PSVD and ESKD
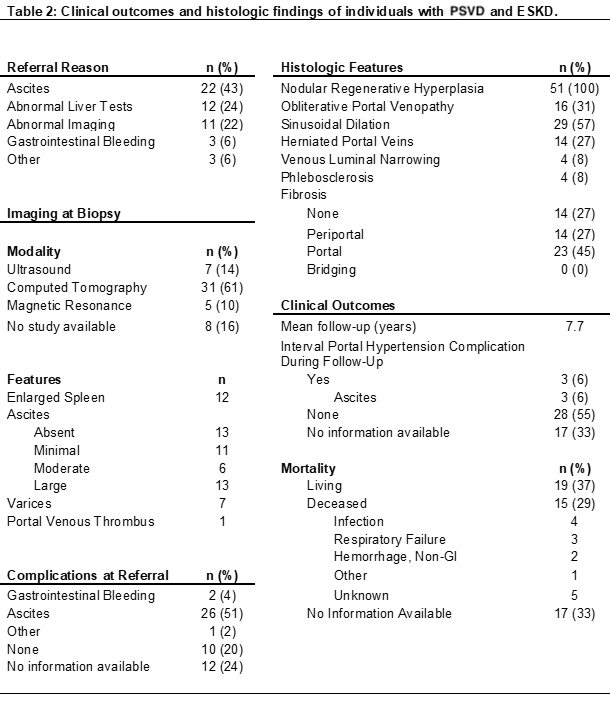
Figure: Clinical outcomes and histologic findings of individuals with PSVD and ESKD
Disclosures:
Alexander Imas indicated no relevant financial relationships.
James Crismale indicated no relevant financial relationships.
Thomas Schiano indicated no relevant financial relationships.
Alexander Imas, MD1, James Crismale, MD2, Thomas Schiano, MD3. P5944 - Porto-Sinusoidal Vascular Disease in End-Stage Kidney Disease: A Distinct Clinical Phenotype With Implications for Transplant Evaluation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Hospital, New York, NY; 3Dept of Abdominal Transplantation Recanati/Miller Transplantation Institute/Division of Liver Diseases, Mt Sinai Hospital, NY, New York, NY
Introduction: Porto-sinusoidal vascular disease (PSVD) is a cause of non-cirrhotic portal hypertension defined by characteristic histology. Differentiating PSVD from cirrhosis is critical due to differences in prognosis and management. While several PSVD risk factors are known, the relationship between end-stage kidney disease (ESKD) requiring kidney replacement therapy and PSVD remains unclear. We aimed to assess the prevalence of ESKD among patients with biopsy-proven PSVD and compare clinical, histologic, and outcome features between those with and without ESKD.
Methods: We conducted a retrospective study of liver biopsies from 2011–2020 at a single center to identify patients with histologic features of PSVD. Those with ESKD on hemodialysis or peritoneal dialysis were matched by age and sex to PSVD controls without ESKD. Patients with evidence of other chronic liver diseases on biopsy or prior transplant were excluded. Clinical data, imaging, histology, portal hypertensive complications, mortality, and transplant outcomes were compared.
Results: Of 755 patients with PSVD histology, 51 (6.8%) had ESKD and were matched with 37 controls. ESKD patients were less often female (20% vs 59%, p< 0.01) and had more comorbidities (hypertension, diabetes, heart failure, HIV; all p< 0.01). A greater proportion had no PSVD risk factors aside from ESKD (51% vs 19%, p< 0.01). ESKD patients more frequently presented with ascites (43% vs 19%, p=0.052) and had ascites on imaging (70% vs 35%, p=0.002), while controls were more often referred for abnormal imaging or labs. Rates of varices and portal hypertensive bleeding were similar. Median HVPG did not differ (3.5 vs 4.5 mmHg, p=0.20). Over ~4.5 years of follow-up, new ascites developed more often in ESKD patients (18% vs 3%, p=0.03). Mortality was higher in the ESKD group (29% vs 3%, p< 0.01), driven by infection and respiratory failure, not portal hypertension. Five ESKD patients underwent kidney transplant after PSVD diagnosis with favorable outcomes.
Discussion: ESKD may be an underrecognized risk factor for PSVD, possibly linked to inflammation, hemodynamic shifts, or prothrombotic states. ESKD-associated PSVD shows a distinct clinical profile with more ascites but fewer classic portal hypertensive complications. Identifying PSVD in ESKD is critical, as it may support candidacy for kidney transplant alone, avoiding simultaneous liver-kidney transplantation.
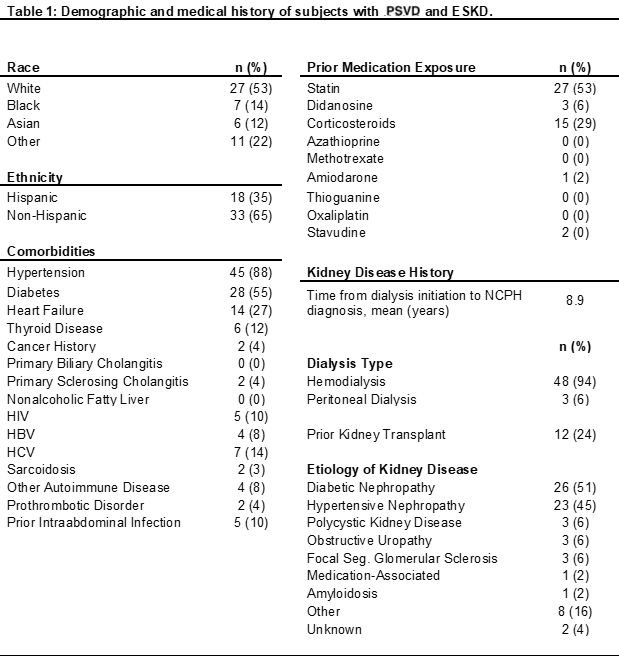
Figure: Demographic and medical history of subjects with PSVD and ESKD
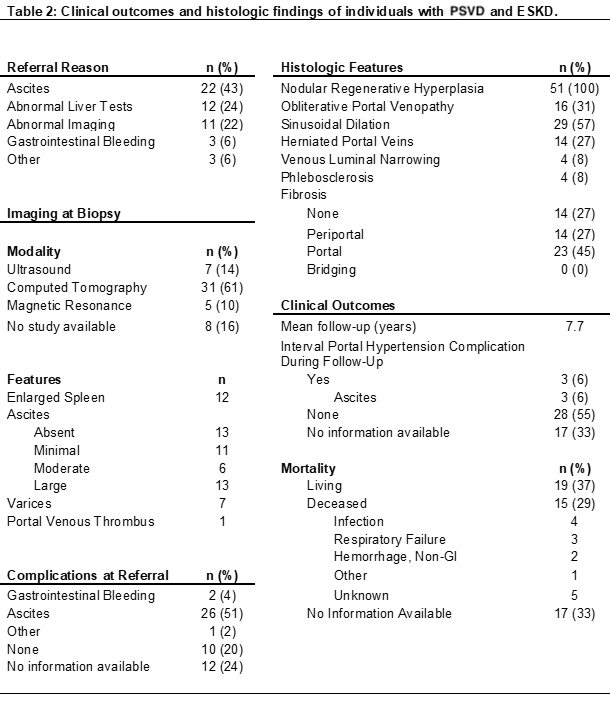
Figure: Clinical outcomes and histologic findings of individuals with PSVD and ESKD
Disclosures:
Alexander Imas indicated no relevant financial relationships.
James Crismale indicated no relevant financial relationships.
Thomas Schiano indicated no relevant financial relationships.
Alexander Imas, MD1, James Crismale, MD2, Thomas Schiano, MD3. P5944 - Porto-Sinusoidal Vascular Disease in End-Stage Kidney Disease: A Distinct Clinical Phenotype With Implications for Transplant Evaluation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
