Tuesday Poster Session
Category: Liver
P5941 - Assessing Predictors of Early and Late Alcohol Relapse Following Liver Transplantation for Alcohol-Associated Liver Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- GM
Garren Montgomery, MD (he/him/his)
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Garren Montgomery, MD1, Ayato Obana, MD1, Antonio Alvarez Castaneda, MD1, Benjamin Davies, MD2, Khalid Mumtaz, MBBS, MSc1
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University College of Medicine, Columbus, OH
Introduction: Alcohol-associated liver disease (ALD) is a leading indication for liver transplantation (LT) in the United States. Alcohol relapse (AR) after LT remains a significant risk and has been associated with graft loss and mortality. However, data on the timing of AR after LT and its predictors remains scarce. Therefore, the aim of this study was to identify predictors of early and late AR after LT.
Methods: We performed a retrospective study of LT recipients (LTRs) for ALD at a single high-volume transplant center between 1/1/2016 and 11/30/2023. LTRs with AR were divided into those with early relapse (ER, relapse within the first 12 months after LT) and those with late relapse (LR, >12 months after LT). Demographics, social determinants of health, and alcohol use data including High Risk Alcohol Relapse (HRAR) and Stanford Integrated Psychosocial Assessment for Transplant (SIPAT) scores were gathered. Logistic regression analysis was used to determine predictors of AR among these two groups.
Results: A total of 383 LTRs were included, with 80 experiencing AR. ER occurred in 28 (35%) LTRs and LR occurred in 52 (65%) LTRs. When comparing patient characteristics between the ER, LR, and no relapse groups, univariate analysis showed that HRAR score ≥4 (p=0.005), recent marijuana use prior to LT (use within 3 months of LT, p=0.0084), and history of psychiatric illness (p=0.042) were significantly associated with relapse. On multivariate analysis, predictors of LR included duration of pre-transplant alcohol abstinence in months (OR: 0.95, p=0.014), SIPAT score as a continuous variable (OR: 1.03, p=0.025), HRAR score ≥4 (OR: 3.44, p=0.01), and low education level (high school or lower; OR: 0.365, p=0.017). No statistically significant predictors of ER were identified, potentially due to limited sample size.
Discussion: We found that higher HRAR (≥4) and SIPAT scores, and a shorter duration of alcohol abstinence prior to LT were associated with increased risk of LR, but not ER. Interestingly, lower education level has a protective effect against LR in our cohort. These observations suggest that a longer duration of close monitoring for alcohol relapse may be warranted in those with shorter duration of pre-LT abstinence and higher HRAR and SIPAT scores.
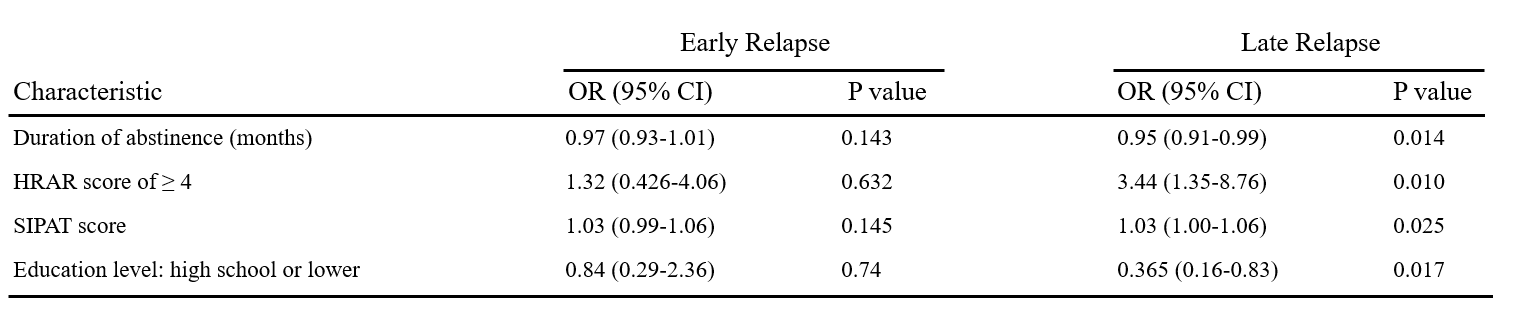
Figure: Title: Table 1: Patient Characteristics.
Caption:
Note: values are either n (%) or median (interquartile range).
MELD-Na, Model for End-Stage Liver Disease serum sodium; LT, liver transplantation; SIPAT, Stanford Integrated Psychosocial Assessment for Transplant; HRAR, High Risk Alcohol Relapse; SALT, Sustained Alcohol Use Post-Liver Transplant; DUI, driving under the influence of alcohol; AUD, alcohol use disorder.
a: High = Associate degree or higher; Middle = some college; Low = High school graduate/GED or lower
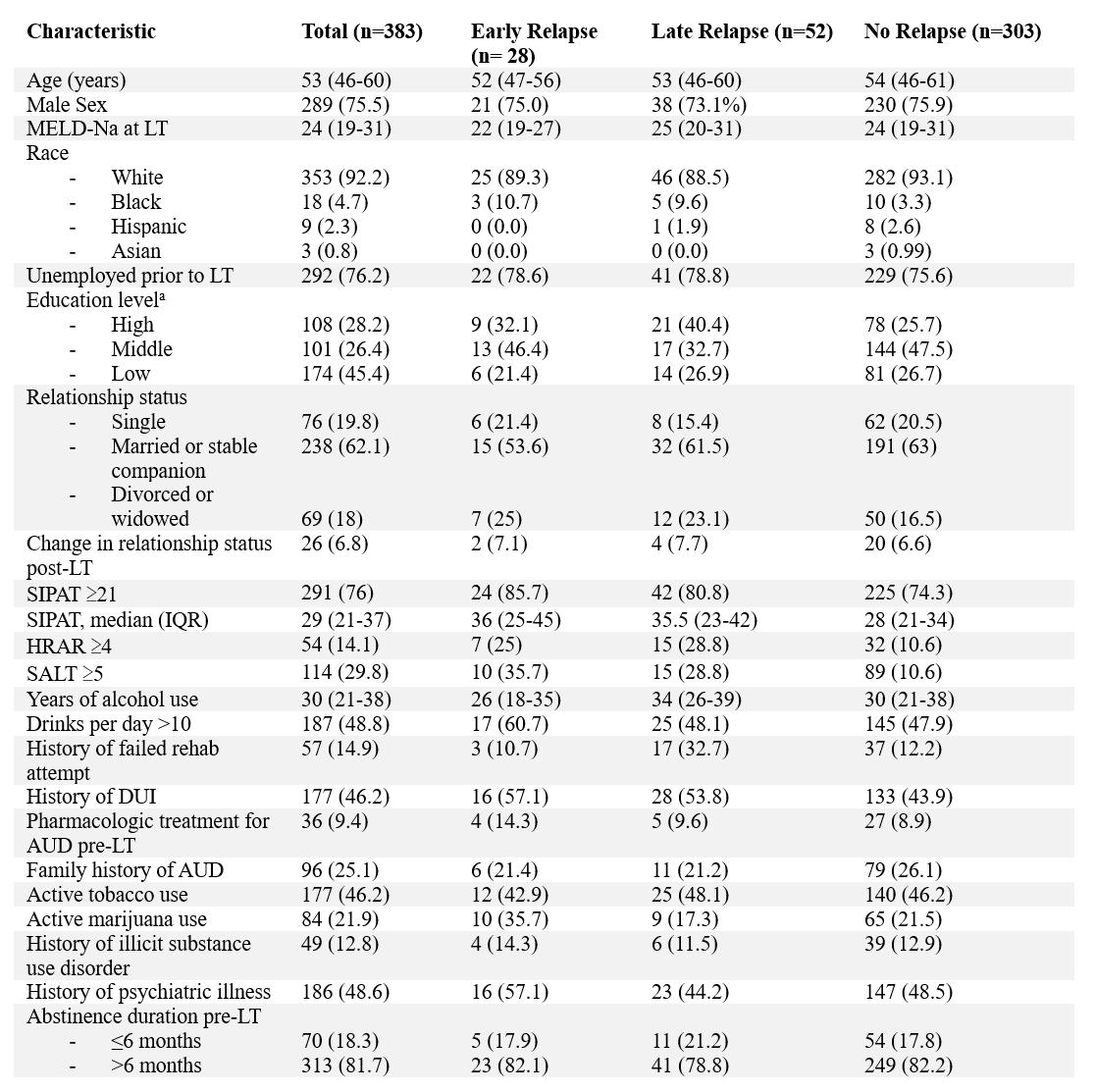
Figure: Title: Table 2: Multivariable Logistic Regression Analysis to Determine Patient Characteristics Associated with Early and Late Relapse.
Caption:
OR, odds ratio; CI, confidence interval; HRAR, High Risk Alcohol Relapse; SIPAT, Stanford Integrated Psychosocial Assessment for Transplant
Disclosures:
Garren Montgomery indicated no relevant financial relationships.
Ayato Obana indicated no relevant financial relationships.
Antonio Alvarez Castaneda indicated no relevant financial relationships.
Benjamin Davies indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Garren Montgomery, MD1, Ayato Obana, MD1, Antonio Alvarez Castaneda, MD1, Benjamin Davies, MD2, Khalid Mumtaz, MBBS, MSc1. P5941 - Assessing Predictors of Early and Late Alcohol Relapse Following Liver Transplantation for Alcohol-Associated Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University College of Medicine, Columbus, OH
Introduction: Alcohol-associated liver disease (ALD) is a leading indication for liver transplantation (LT) in the United States. Alcohol relapse (AR) after LT remains a significant risk and has been associated with graft loss and mortality. However, data on the timing of AR after LT and its predictors remains scarce. Therefore, the aim of this study was to identify predictors of early and late AR after LT.
Methods: We performed a retrospective study of LT recipients (LTRs) for ALD at a single high-volume transplant center between 1/1/2016 and 11/30/2023. LTRs with AR were divided into those with early relapse (ER, relapse within the first 12 months after LT) and those with late relapse (LR, >12 months after LT). Demographics, social determinants of health, and alcohol use data including High Risk Alcohol Relapse (HRAR) and Stanford Integrated Psychosocial Assessment for Transplant (SIPAT) scores were gathered. Logistic regression analysis was used to determine predictors of AR among these two groups.
Results: A total of 383 LTRs were included, with 80 experiencing AR. ER occurred in 28 (35%) LTRs and LR occurred in 52 (65%) LTRs. When comparing patient characteristics between the ER, LR, and no relapse groups, univariate analysis showed that HRAR score ≥4 (p=0.005), recent marijuana use prior to LT (use within 3 months of LT, p=0.0084), and history of psychiatric illness (p=0.042) were significantly associated with relapse. On multivariate analysis, predictors of LR included duration of pre-transplant alcohol abstinence in months (OR: 0.95, p=0.014), SIPAT score as a continuous variable (OR: 1.03, p=0.025), HRAR score ≥4 (OR: 3.44, p=0.01), and low education level (high school or lower; OR: 0.365, p=0.017). No statistically significant predictors of ER were identified, potentially due to limited sample size.
Discussion: We found that higher HRAR (≥4) and SIPAT scores, and a shorter duration of alcohol abstinence prior to LT were associated with increased risk of LR, but not ER. Interestingly, lower education level has a protective effect against LR in our cohort. These observations suggest that a longer duration of close monitoring for alcohol relapse may be warranted in those with shorter duration of pre-LT abstinence and higher HRAR and SIPAT scores.
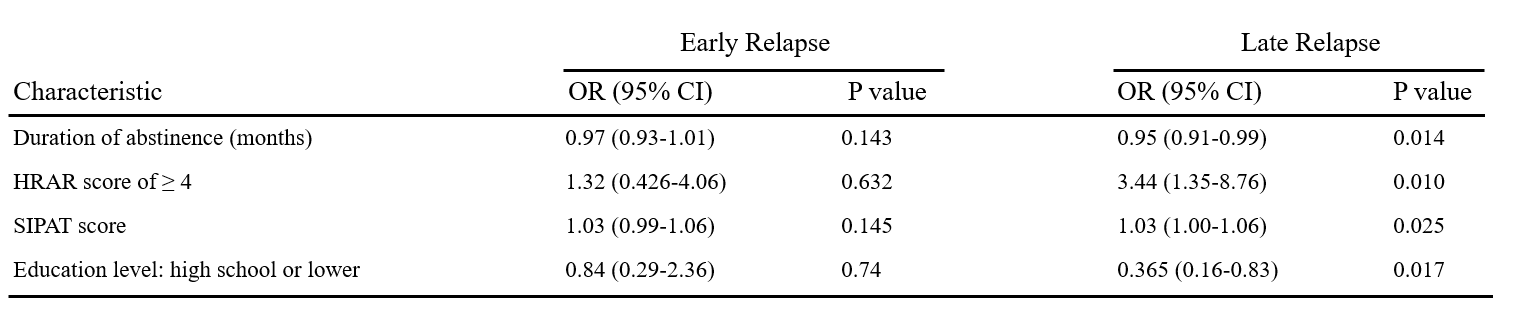
Figure: Title: Table 1: Patient Characteristics.
Caption:
Note: values are either n (%) or median (interquartile range).
MELD-Na, Model for End-Stage Liver Disease serum sodium; LT, liver transplantation; SIPAT, Stanford Integrated Psychosocial Assessment for Transplant; HRAR, High Risk Alcohol Relapse; SALT, Sustained Alcohol Use Post-Liver Transplant; DUI, driving under the influence of alcohol; AUD, alcohol use disorder.
a: High = Associate degree or higher; Middle = some college; Low = High school graduate/GED or lower
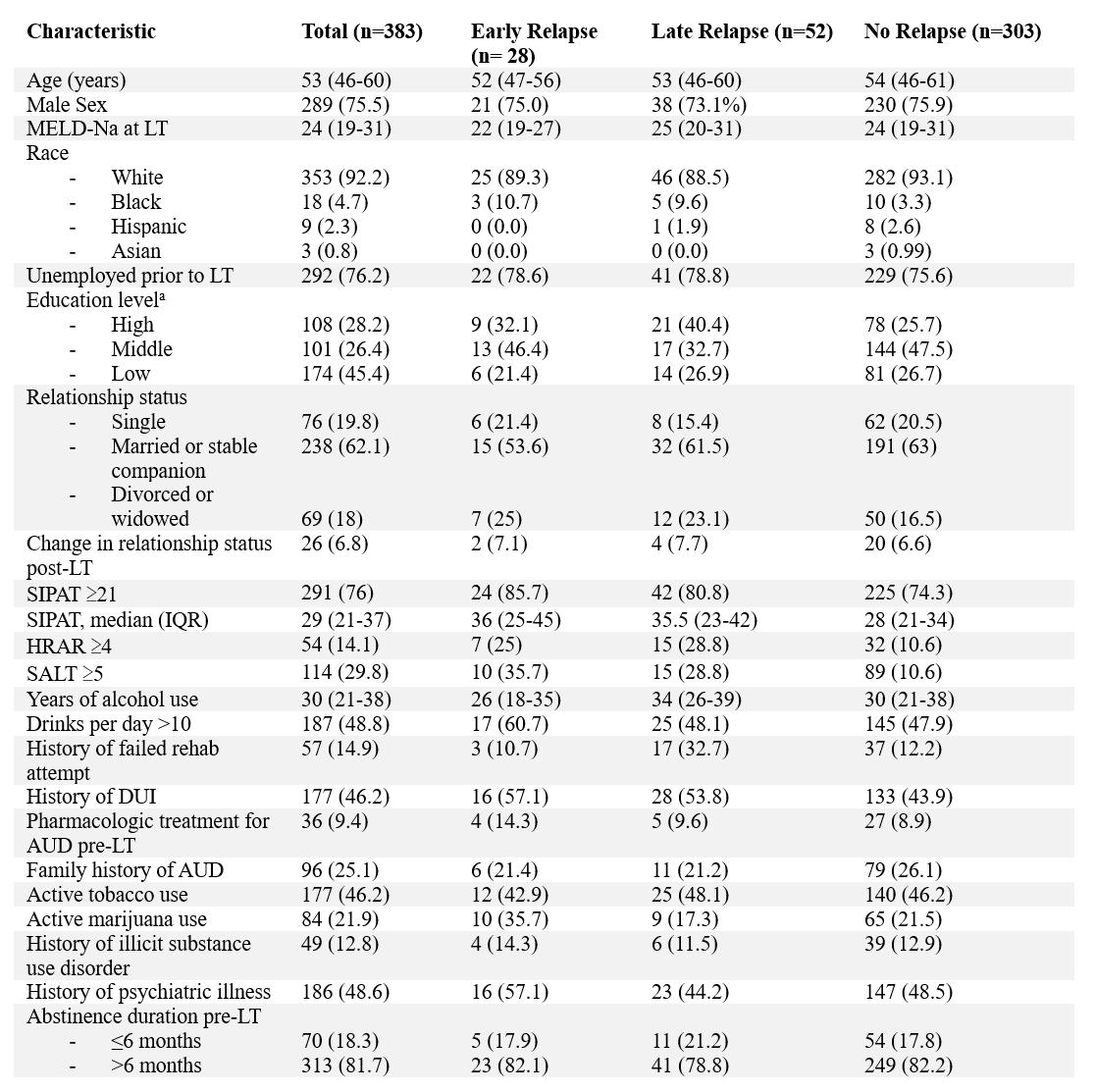
Figure: Title: Table 2: Multivariable Logistic Regression Analysis to Determine Patient Characteristics Associated with Early and Late Relapse.
Caption:
OR, odds ratio; CI, confidence interval; HRAR, High Risk Alcohol Relapse; SIPAT, Stanford Integrated Psychosocial Assessment for Transplant
Disclosures:
Garren Montgomery indicated no relevant financial relationships.
Ayato Obana indicated no relevant financial relationships.
Antonio Alvarez Castaneda indicated no relevant financial relationships.
Benjamin Davies indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Garren Montgomery, MD1, Ayato Obana, MD1, Antonio Alvarez Castaneda, MD1, Benjamin Davies, MD2, Khalid Mumtaz, MBBS, MSc1. P5941 - Assessing Predictors of Early and Late Alcohol Relapse Following Liver Transplantation for Alcohol-Associated Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

