Tuesday Poster Session
Category: Liver
P5964 - Rapidly Progressive Multisystem Organ Failure Due to EBV+ Primary Hepatic PTCL
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Max E. Edeson, MD
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Max E. Edeson, MD1, Aneesh Bhave, BS2, Ethan Burg, MS2, Gabrielle Sharbin, MS2, Davood Karimi Hosseini, MD2, Chinmay Trivedi, MD2, Shalom Frager, MD2, Shil Patel, DO2, Jonathan Weinberger, MD2, Rosario Ligresti, MD2
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Hackensack University Medical Center, Hackensack, NJ
Introduction: Peripheral T-Cell Lymphoma (PTCL) is a rare, aggressive form of Non-Hodgkin Lymphoma. Hepatosplenic/primary hepatic PTCL (HSPTCL) is a rarer subtype, < 1% of cases. It typically occurs in males aged 35 on immunosuppression, with no clear etiology, although associated with infections like EBV and other mutagens. Liver biopsy is vital for diagnosis. Rapid progression is common, especially if complicated by HLH. We present a case of EBV-driven HSPTCL causing multi-organ failure in a previously healthy man to increase awareness of a rare, acute, severe pathology.
Case Description/
Methods: A 35-year-old African American male with no medical history presented with 4 days of abdominal pain, nausea/vomiting, constipation, dark urine, and poor appetite - denied fever, travel, substance use, or family history. He was ill appearing, oriented, tachycardic, jaundiced, with epigastric tenderness and hepatomegaly. Labs showed leukocytosis, AKI, lactic acidosis (14.8 mmol/L), hyperbilirubinemia (12.2 mg/dL), transaminemia. RUQ ultrasound found hepatomegaly (21.3 cm) and gallbladder wall thickening with biliary sludge (Figure 1). Emergent ERCP for suspected cholangitis found sludge, no purulence or obstruction - stent was placed. Patient deteriorated rapidly - admitted to ICU with severe acidosis, renal and respiratory failure requiring intubation and continuous dialysis. During liver biopsy, he suffered a cardiac arrest and was resuscitated - required vasopressors and ECMO. Liver biopsy and blood revealed atypical lymphocytes with vacuolated cytoplasm, irregular nuclear contours, prominent nucleoli, and immature features (Figure 2); EBV DNA was elevated (89x10^6), flow cytometry and other serum studies were negative; he was diagnosed with EBV-driven HSPTCL. Renal function and oxygenation improved with high-dose steroids. Symptoms and LFTs further improved with cyclophosphamide and EPOCH chemotherapy - treatment was deescalated, and he was discharged with outpatient follow-up to Oncology.
Discussion: EBV-associated HSPTCL is a rare and aggressive malignancy that can present with multiorgan failure. Diagnosis is delayed due to nonspecific symptoms and overlap with other hepatic/infectious causes. Organ failure can occur even without HLH due to liver failure causing a systemic response. Early identification is critical given its rapid progression and poor prognosis even with early and aggressive treatment. This is true even for patients with no family or past medical history as seen here.
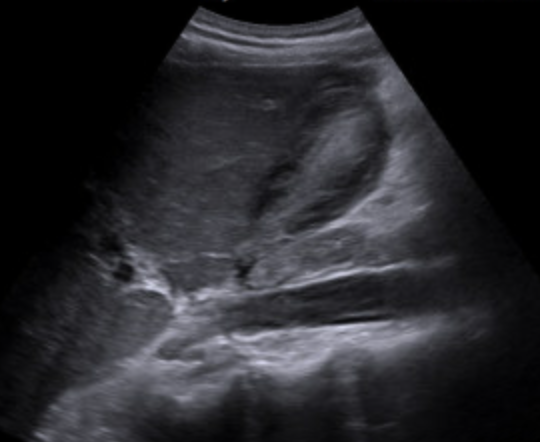
Figure: Figure 1: RUQ U/S showing hepatomegaly and biliary sludge

Figure: Figure 2: Liver Biopsy stained with H&E confirming diagnosis of PTCL primary hepatic
Disclosures:
Max Edeson indicated no relevant financial relationships.
Aneesh Bhave indicated no relevant financial relationships.
Ethan Burg indicated no relevant financial relationships.
Gabrielle Sharbin indicated no relevant financial relationships.
Davood Karimi Hosseini indicated no relevant financial relationships.
Chinmay Trivedi indicated no relevant financial relationships.
Shalom Frager indicated no relevant financial relationships.
Shil Patel indicated no relevant financial relationships.
Jonathan Weinberger indicated no relevant financial relationships.
Rosario Ligresti indicated no relevant financial relationships.
Max E. Edeson, MD1, Aneesh Bhave, BS2, Ethan Burg, MS2, Gabrielle Sharbin, MS2, Davood Karimi Hosseini, MD2, Chinmay Trivedi, MD2, Shalom Frager, MD2, Shil Patel, DO2, Jonathan Weinberger, MD2, Rosario Ligresti, MD2. P5964 - Rapidly Progressive Multisystem Organ Failure Due to EBV+ Primary Hepatic PTCL, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Hackensack University Medical Center, Hackensack, NJ
Introduction: Peripheral T-Cell Lymphoma (PTCL) is a rare, aggressive form of Non-Hodgkin Lymphoma. Hepatosplenic/primary hepatic PTCL (HSPTCL) is a rarer subtype, < 1% of cases. It typically occurs in males aged 35 on immunosuppression, with no clear etiology, although associated with infections like EBV and other mutagens. Liver biopsy is vital for diagnosis. Rapid progression is common, especially if complicated by HLH. We present a case of EBV-driven HSPTCL causing multi-organ failure in a previously healthy man to increase awareness of a rare, acute, severe pathology.
Case Description/
Methods: A 35-year-old African American male with no medical history presented with 4 days of abdominal pain, nausea/vomiting, constipation, dark urine, and poor appetite - denied fever, travel, substance use, or family history. He was ill appearing, oriented, tachycardic, jaundiced, with epigastric tenderness and hepatomegaly. Labs showed leukocytosis, AKI, lactic acidosis (14.8 mmol/L), hyperbilirubinemia (12.2 mg/dL), transaminemia. RUQ ultrasound found hepatomegaly (21.3 cm) and gallbladder wall thickening with biliary sludge (Figure 1). Emergent ERCP for suspected cholangitis found sludge, no purulence or obstruction - stent was placed. Patient deteriorated rapidly - admitted to ICU with severe acidosis, renal and respiratory failure requiring intubation and continuous dialysis. During liver biopsy, he suffered a cardiac arrest and was resuscitated - required vasopressors and ECMO. Liver biopsy and blood revealed atypical lymphocytes with vacuolated cytoplasm, irregular nuclear contours, prominent nucleoli, and immature features (Figure 2); EBV DNA was elevated (89x10^6), flow cytometry and other serum studies were negative; he was diagnosed with EBV-driven HSPTCL. Renal function and oxygenation improved with high-dose steroids. Symptoms and LFTs further improved with cyclophosphamide and EPOCH chemotherapy - treatment was deescalated, and he was discharged with outpatient follow-up to Oncology.
Discussion: EBV-associated HSPTCL is a rare and aggressive malignancy that can present with multiorgan failure. Diagnosis is delayed due to nonspecific symptoms and overlap with other hepatic/infectious causes. Organ failure can occur even without HLH due to liver failure causing a systemic response. Early identification is critical given its rapid progression and poor prognosis even with early and aggressive treatment. This is true even for patients with no family or past medical history as seen here.
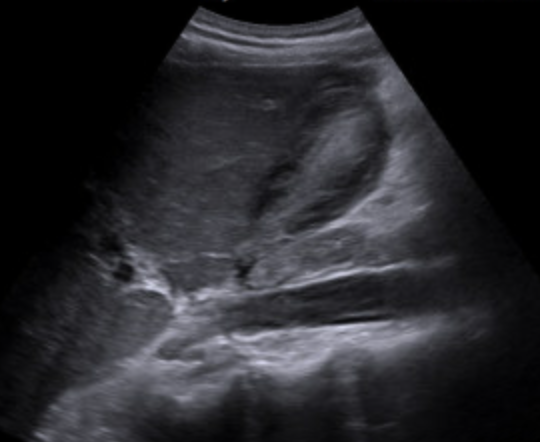
Figure: Figure 1: RUQ U/S showing hepatomegaly and biliary sludge

Figure: Figure 2: Liver Biopsy stained with H&E confirming diagnosis of PTCL primary hepatic
Disclosures:
Max Edeson indicated no relevant financial relationships.
Aneesh Bhave indicated no relevant financial relationships.
Ethan Burg indicated no relevant financial relationships.
Gabrielle Sharbin indicated no relevant financial relationships.
Davood Karimi Hosseini indicated no relevant financial relationships.
Chinmay Trivedi indicated no relevant financial relationships.
Shalom Frager indicated no relevant financial relationships.
Shil Patel indicated no relevant financial relationships.
Jonathan Weinberger indicated no relevant financial relationships.
Rosario Ligresti indicated no relevant financial relationships.
Max E. Edeson, MD1, Aneesh Bhave, BS2, Ethan Burg, MS2, Gabrielle Sharbin, MS2, Davood Karimi Hosseini, MD2, Chinmay Trivedi, MD2, Shalom Frager, MD2, Shil Patel, DO2, Jonathan Weinberger, MD2, Rosario Ligresti, MD2. P5964 - Rapidly Progressive Multisystem Organ Failure Due to EBV+ Primary Hepatic PTCL, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
