Tuesday Poster Session
Category: Liver
P5869 - Phase 1: Improving FIB-4 Screening in the Underserved Primary Care Setting for At-Risk Populations of Metabolic Dysfunction-Associated Steatotic Liver Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Danzhu Zhao, DO
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Danzhu Zhao, DO1, Ruchir Paladiya, MBBS2, Amanda Frondella, MD3, Nicole Bambara, MD3, Neil Khoury, MD1, Cunegundo Vergara, MD4
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut School of Medicine, Farmington, CT; 3University of Connecticut Health, Farmington, CT; 4Hartford Hospital, Hartford, CT
Introduction: The prevalence of metabolic dysfunction-associated steatotic liver disease (MASLD) is rising globally (25–30%), influenced by risk factors such as type 2 diabetes mellitus (T2DM), obesity, hypertension, among others. T2DM is a major risk factor for MASLD, fibrosis progression, and hepatocellular carcinoma. The American Association for the Study of Liver Diseases (AASLD) recommends FIB-4 scoring for risk stratification, but this had not been implemented at the Hartford Hospital Adult Primary Care Clinic, which serves a high-risk, underserved population.
Methods: Baseline screening with FIB-4 scoring prior to our interventions was only 0.6%. We utilized the electronic health record (Epic) “smartphrase” known as “.fib4” to self-populate a calculated FIB-4 score based on available laboratory studies and patient age.
To improve utilization, we implemented a multi-level strategy that included provider education, workflow integration, and interdisciplinary support. A simplified one-page screening algorithm was emailed to clinic physicians and posted in provider workspaces. To incorporate FIB-4 use into daily workflow, nurses prompted physicians to calculate FIB-4 for patients with T2DM undergoing hemoglobin A1c (Hgb A1c) testing that day. Data was extracted from the clinic database and electronic medical records before (04/20/2023) and after (on 04/20/2025) intervention. We included patients at least 35 years old. Patients who were deceased, no longer active in the clinic, or under 35 years old were excluded.
Results: Screening rates improved from 0.6% to 1.9%, a more than threefold increase. Despite this advancement, overall screening rates continue to be suboptimal.
Discussion: Implementing a multidisciplinary screening protocol for MASLD in the primary care clinic significantly increased FIB-4 use. Key barriers included knowledge gaps on the clinical significance associated with FIB-4 screening. We plan to address this with formal educational sessions and pre- and post-education surveys designed to reinforce knowledge retention through active recall techniques. Many patients were ineligible for FIB-4 due to outdated complete blood count or liver function tests which should be checked annually in diabetics. We also identified patients who were not seen during the intervention window due to missed visits which decreases opportunity for screening. Future steps will aim to integrate additional risk factors, including obesity and hypertension, into the screening protocol.
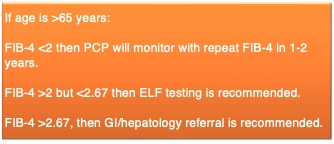
Figure: Figure 1. FIB-4 algorithm for evaluating patients ages at least 35 years but less than 65 years at high risk for MASLD.
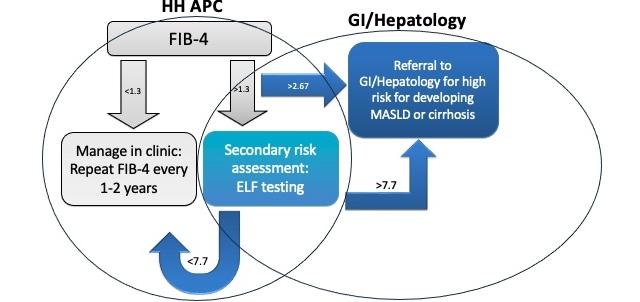
Figure: Figure 2. FIB-4 algorithm for evaluating patients over 65 years who are high risk for MASLD.
Disclosures:
Danzhu Zhao indicated no relevant financial relationships.
Ruchir Paladiya indicated no relevant financial relationships.
Amanda Frondella indicated no relevant financial relationships.
Nicole Bambara indicated no relevant financial relationships.
Neil Khoury indicated no relevant financial relationships.
Cunegundo Vergara indicated no relevant financial relationships.
Danzhu Zhao, DO1, Ruchir Paladiya, MBBS2, Amanda Frondella, MD3, Nicole Bambara, MD3, Neil Khoury, MD1, Cunegundo Vergara, MD4. P5869 - Phase 1: Improving FIB-4 Screening in the Underserved Primary Care Setting for At-Risk Populations of Metabolic Dysfunction-Associated Steatotic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut School of Medicine, Farmington, CT; 3University of Connecticut Health, Farmington, CT; 4Hartford Hospital, Hartford, CT
Introduction: The prevalence of metabolic dysfunction-associated steatotic liver disease (MASLD) is rising globally (25–30%), influenced by risk factors such as type 2 diabetes mellitus (T2DM), obesity, hypertension, among others. T2DM is a major risk factor for MASLD, fibrosis progression, and hepatocellular carcinoma. The American Association for the Study of Liver Diseases (AASLD) recommends FIB-4 scoring for risk stratification, but this had not been implemented at the Hartford Hospital Adult Primary Care Clinic, which serves a high-risk, underserved population.
Methods: Baseline screening with FIB-4 scoring prior to our interventions was only 0.6%. We utilized the electronic health record (Epic) “smartphrase” known as “.fib4” to self-populate a calculated FIB-4 score based on available laboratory studies and patient age.
To improve utilization, we implemented a multi-level strategy that included provider education, workflow integration, and interdisciplinary support. A simplified one-page screening algorithm was emailed to clinic physicians and posted in provider workspaces. To incorporate FIB-4 use into daily workflow, nurses prompted physicians to calculate FIB-4 for patients with T2DM undergoing hemoglobin A1c (Hgb A1c) testing that day. Data was extracted from the clinic database and electronic medical records before (04/20/2023) and after (on 04/20/2025) intervention. We included patients at least 35 years old. Patients who were deceased, no longer active in the clinic, or under 35 years old were excluded.
Results: Screening rates improved from 0.6% to 1.9%, a more than threefold increase. Despite this advancement, overall screening rates continue to be suboptimal.
Discussion: Implementing a multidisciplinary screening protocol for MASLD in the primary care clinic significantly increased FIB-4 use. Key barriers included knowledge gaps on the clinical significance associated with FIB-4 screening. We plan to address this with formal educational sessions and pre- and post-education surveys designed to reinforce knowledge retention through active recall techniques. Many patients were ineligible for FIB-4 due to outdated complete blood count or liver function tests which should be checked annually in diabetics. We also identified patients who were not seen during the intervention window due to missed visits which decreases opportunity for screening. Future steps will aim to integrate additional risk factors, including obesity and hypertension, into the screening protocol.
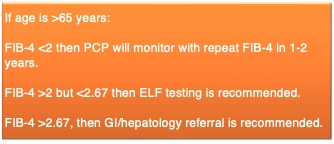
Figure: Figure 1. FIB-4 algorithm for evaluating patients ages at least 35 years but less than 65 years at high risk for MASLD.
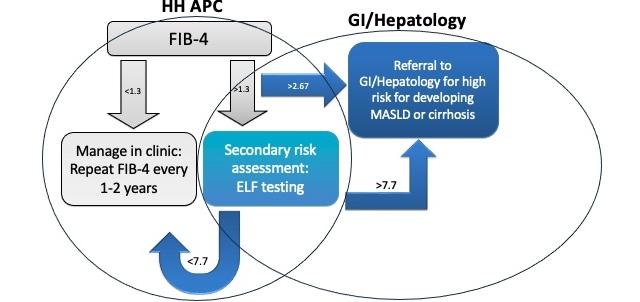
Figure: Figure 2. FIB-4 algorithm for evaluating patients over 65 years who are high risk for MASLD.
Disclosures:
Danzhu Zhao indicated no relevant financial relationships.
Ruchir Paladiya indicated no relevant financial relationships.
Amanda Frondella indicated no relevant financial relationships.
Nicole Bambara indicated no relevant financial relationships.
Neil Khoury indicated no relevant financial relationships.
Cunegundo Vergara indicated no relevant financial relationships.
Danzhu Zhao, DO1, Ruchir Paladiya, MBBS2, Amanda Frondella, MD3, Nicole Bambara, MD3, Neil Khoury, MD1, Cunegundo Vergara, MD4. P5869 - Phase 1: Improving FIB-4 Screening in the Underserved Primary Care Setting for At-Risk Populations of Metabolic Dysfunction-Associated Steatotic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

