Tuesday Poster Session
Category: Liver
P5868 - Potential Impact of Hepatic Encephalopathy on Clinical Outcomes in Patients Hospitalized With Alcohol-Related Hepatitis: Insights from a National Inpatient Database
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Adham Obeidat, MD (he/him/his)
presbyterian Hospital
Albuquerque, NM
Presenting Author(s)
Adham Obeidat, MD1, Gicel J. Aguilar, BS, DO2, Ahmad Abou Yassine, MD2, Christopher Chang, MD, PhD3
1presbyterian Hospital, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM; 3University of New Mexico School of Medicine, Albuquerque, NM
Introduction: Alcohol-related hepatitis (AH) is a severe and often life-threatening manifestation of alcohol-related liver disease (ALD). Hepatic encephalopathy (HE), a common complication of advanced liver dysfunction, may further worsen clinical outcomes. This study aimed to characterize patients hospitalized with AH and concomitant HE to evaluate the impact of HE on in-hospital outcomes.
Methods: Using the United States National Inpatient Sample (NIS) database, a retrospective study was conducted to identify hospitalized adults with the diagnosis of AH between 2019 and 2021. Using ICD codes, we identified adult patients who were admitted with a primary diagnosis of AH and stratified them based on the presence or absence of HE. We compared demographic and clinical characteristics, as well as, in-hospital mortality and other clinical outcomes including sepsis, spontaneous bacterial peritonitis (SBP), hyponatremia, respiratory failure (RF), malnutrition, cardiac arrest and acute kidney injury (AKI). Multivariate logistic regression was used to adjust for relevant variables.
Results: Among 91,787 patients hospitalized with AH, 11,652 (12.7%) had HE. Compared to those without HE, these patients were older (mean age 50.4 vs. 46.8 years), had longer hospital stays (10.5 vs. 5.6 days), and higher mean hospitalization costs ($127,977 vs. $59,109). Additionally, the HE group had significantly higher in-hospital mortality (12.7% vs. 3.1%).
Multivariate regression analysis identified malnutrition (OR 1.74), AKI (OR 2.24), sepsis (OR 2.69), cirrhosis (OR 1.11), and hyponatremia (OR 1.36) as independent predictors of HE in patients with AH. Further, HE itself was an independent predictor of in-hospital mortality (OR 3.90), RF (OR 4.65), sepsis (OR 3.30), SBP (OR 1.41), cardiac arrest (OR 3.31) and increased LOS (OR 1.55) in patients with AH.
Discussion: HE is a significant predictor to increase mortality and worse clinical outcomes in patients admitted with AH. Recognition of associated predictors such as malnutrition, renal dysfunction, and sepsis may help guide early interventions aimed at improving outcomes in this high-risk population.
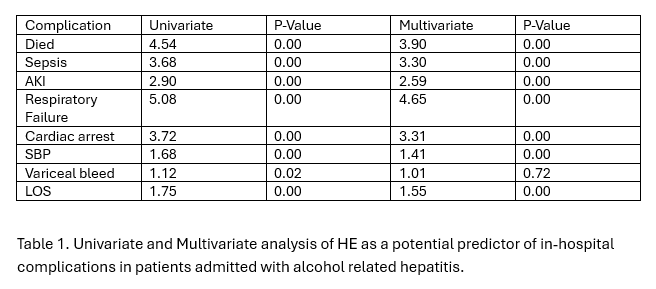
Figure: Table 1. Univariate and Multivariate analysis of HE as a potential predictor of in-hospital complications in patients admitted with alcohol related hepatitis.
Disclosures:
Adham Obeidat indicated no relevant financial relationships.
Gicel Aguilar indicated no relevant financial relationships.
Ahmad Abou Yassine indicated no relevant financial relationships.
Christopher Chang: Mirum Pharmaceuticals – Advisory Committee/Board Member. Nestle Health – Speakers Bureau. Salix Pharmaceuticals – Advisory Committee/Board Member.
Adham Obeidat, MD1, Gicel J. Aguilar, BS, DO2, Ahmad Abou Yassine, MD2, Christopher Chang, MD, PhD3. P5868 - Potential Impact of Hepatic Encephalopathy on Clinical Outcomes in Patients Hospitalized With Alcohol-Related Hepatitis: Insights from a National Inpatient Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1presbyterian Hospital, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM; 3University of New Mexico School of Medicine, Albuquerque, NM
Introduction: Alcohol-related hepatitis (AH) is a severe and often life-threatening manifestation of alcohol-related liver disease (ALD). Hepatic encephalopathy (HE), a common complication of advanced liver dysfunction, may further worsen clinical outcomes. This study aimed to characterize patients hospitalized with AH and concomitant HE to evaluate the impact of HE on in-hospital outcomes.
Methods: Using the United States National Inpatient Sample (NIS) database, a retrospective study was conducted to identify hospitalized adults with the diagnosis of AH between 2019 and 2021. Using ICD codes, we identified adult patients who were admitted with a primary diagnosis of AH and stratified them based on the presence or absence of HE. We compared demographic and clinical characteristics, as well as, in-hospital mortality and other clinical outcomes including sepsis, spontaneous bacterial peritonitis (SBP), hyponatremia, respiratory failure (RF), malnutrition, cardiac arrest and acute kidney injury (AKI). Multivariate logistic regression was used to adjust for relevant variables.
Results: Among 91,787 patients hospitalized with AH, 11,652 (12.7%) had HE. Compared to those without HE, these patients were older (mean age 50.4 vs. 46.8 years), had longer hospital stays (10.5 vs. 5.6 days), and higher mean hospitalization costs ($127,977 vs. $59,109). Additionally, the HE group had significantly higher in-hospital mortality (12.7% vs. 3.1%).
Multivariate regression analysis identified malnutrition (OR 1.74), AKI (OR 2.24), sepsis (OR 2.69), cirrhosis (OR 1.11), and hyponatremia (OR 1.36) as independent predictors of HE in patients with AH. Further, HE itself was an independent predictor of in-hospital mortality (OR 3.90), RF (OR 4.65), sepsis (OR 3.30), SBP (OR 1.41), cardiac arrest (OR 3.31) and increased LOS (OR 1.55) in patients with AH.
Discussion: HE is a significant predictor to increase mortality and worse clinical outcomes in patients admitted with AH. Recognition of associated predictors such as malnutrition, renal dysfunction, and sepsis may help guide early interventions aimed at improving outcomes in this high-risk population.
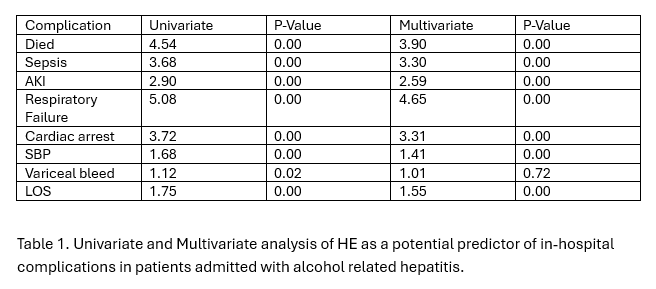
Figure: Table 1. Univariate and Multivariate analysis of HE as a potential predictor of in-hospital complications in patients admitted with alcohol related hepatitis.
Disclosures:
Adham Obeidat indicated no relevant financial relationships.
Gicel Aguilar indicated no relevant financial relationships.
Ahmad Abou Yassine indicated no relevant financial relationships.
Christopher Chang: Mirum Pharmaceuticals – Advisory Committee/Board Member. Nestle Health – Speakers Bureau. Salix Pharmaceuticals – Advisory Committee/Board Member.
Adham Obeidat, MD1, Gicel J. Aguilar, BS, DO2, Ahmad Abou Yassine, MD2, Christopher Chang, MD, PhD3. P5868 - Potential Impact of Hepatic Encephalopathy on Clinical Outcomes in Patients Hospitalized With Alcohol-Related Hepatitis: Insights from a National Inpatient Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
