Tuesday Poster Session
Category: Liver
P5866 - AI-Based Risk Stratification and Time-to-Transplant Prediction in Cirrhosis Using Random Survival Forest Modeling
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sri Harsha Boppana, MBBS, MD
Nassau University Medical Center
Hicksville, NY
Presenting Author(s)
Sri Harsha Boppana, MBBS, MD1, Manaswitha Thota, MD2, Gautam Maddineni, MD3, Sachin Sravan Kumar Komati, 4, Sarath Chandra Ponnada, 5, Sai Lakshmi Prasanna Komati, MBBS6, C. David Mintz, MD, PhD7
1Nassau University Medical Center, East Meadow, NY; 2Virginia Commonwealth University, Richmond, VA; 3Florida State University, Cape Coral, FL; 4Florida International University, Florida, FL; 5Great Eastern Medical School and Hospital, Srikakulam, Srikakulam, Andhra Pradesh, India; 6Government Medical College, Ongole, Ongole, Andhra Pradesh, India; 7Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: Cirrhosis patients often follow an unpredictable clinical course, and timely identification of those at greatest risk for liver transplantation remains an unmet need. We developed a random survival forest combining routine laboratory values with three engineered predictors age-adjusted enzyme ratios, treatment-response flags, and a composite severity score to predict transplant-free survival and identify key prognostic markers.
Methods: We assembled a de-identified cohort of cirrhosis patients from a tertiary‐care database and extracted routinely collected variables, including age, bilirubin, serum glutamic-oxaloacetic transaminase, albumin, comorbidity indices, and treatment history. We engineered three novel features—age-adjusted liver enzyme ratios, binary treatment-response flags, and a composite severity score—and handled missing data via mean imputation for continuous variables and mode imputation for categorical variables. We randomly allocated 80%of the records to a training set and reserved 20% for independent testing. We then implemented a random survival forest with 100 trees using the sksurv library, tuning split-rule and node-size hyperparameters through five-fold cross-validation. We assessed discrimination by the concordance index and visualized risk stratification with Kaplan–Meier survival curves. We applied permutation-based importance analysis to rank predictors of time to transplantation.
Results: The model yielded a concordance index of 0.94 on the training cohort and 0.82 on the test cohort.Permutation importance pinpointed age, bilirubin, and SGOT as the top three predictors of transplant risk. Stratification into low-, medium-, and high-risk groups captured 29%, 37%, and 34%of the cohort, respectively. Median transplant-free survival was 2,450 days in the low-risk group, 1,520 days in the medium-risk group, and 890 days in the high-risk group. Kaplan–Meier curves demonstrated clear separation among all three risk strata (log-rank p < 0.001), confirming robust prognostic discrimination and supporting the model’s potential for guiding timely transplant assessments.
Discussion: Our model demonstrated high discriminative performance, stratifying patients into low-, medium-, and high-risk groups with significantly different median transplant-free survival times. Incorporating novel engineered features alongside traditional laboratory measures shows promise for personalized transplant referral strategies; external validation will be essential to confirm clinical utility.
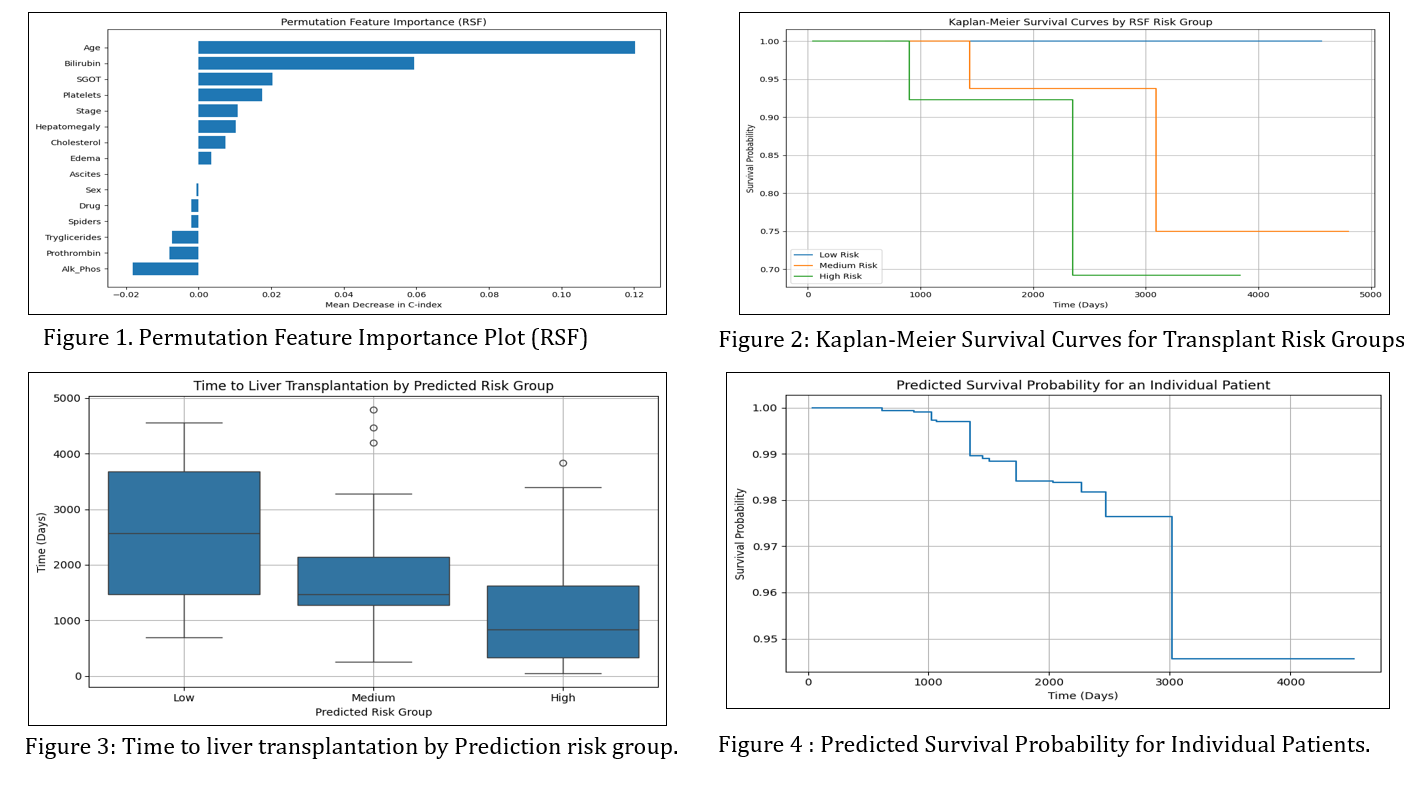
Figure: Figure 1, 2, 3, 4.
Disclosures:
Sri Harsha Boppana indicated no relevant financial relationships.
Manaswitha Thota indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Sachin Sravan Kumar Komati indicated no relevant financial relationships.
Sarath Chandra Ponnada indicated no relevant financial relationships.
Sai Lakshmi Prasanna Komati indicated no relevant financial relationships.
C. David Mintz indicated no relevant financial relationships.
Sri Harsha Boppana, MBBS, MD1, Manaswitha Thota, MD2, Gautam Maddineni, MD3, Sachin Sravan Kumar Komati, 4, Sarath Chandra Ponnada, 5, Sai Lakshmi Prasanna Komati, MBBS6, C. David Mintz, MD, PhD7. P5866 - AI-Based Risk Stratification and Time-to-Transplant Prediction in Cirrhosis Using Random Survival Forest Modeling, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Nassau University Medical Center, East Meadow, NY; 2Virginia Commonwealth University, Richmond, VA; 3Florida State University, Cape Coral, FL; 4Florida International University, Florida, FL; 5Great Eastern Medical School and Hospital, Srikakulam, Srikakulam, Andhra Pradesh, India; 6Government Medical College, Ongole, Ongole, Andhra Pradesh, India; 7Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: Cirrhosis patients often follow an unpredictable clinical course, and timely identification of those at greatest risk for liver transplantation remains an unmet need. We developed a random survival forest combining routine laboratory values with three engineered predictors age-adjusted enzyme ratios, treatment-response flags, and a composite severity score to predict transplant-free survival and identify key prognostic markers.
Methods: We assembled a de-identified cohort of cirrhosis patients from a tertiary‐care database and extracted routinely collected variables, including age, bilirubin, serum glutamic-oxaloacetic transaminase, albumin, comorbidity indices, and treatment history. We engineered three novel features—age-adjusted liver enzyme ratios, binary treatment-response flags, and a composite severity score—and handled missing data via mean imputation for continuous variables and mode imputation for categorical variables. We randomly allocated 80%of the records to a training set and reserved 20% for independent testing. We then implemented a random survival forest with 100 trees using the sksurv library, tuning split-rule and node-size hyperparameters through five-fold cross-validation. We assessed discrimination by the concordance index and visualized risk stratification with Kaplan–Meier survival curves. We applied permutation-based importance analysis to rank predictors of time to transplantation.
Results: The model yielded a concordance index of 0.94 on the training cohort and 0.82 on the test cohort.Permutation importance pinpointed age, bilirubin, and SGOT as the top three predictors of transplant risk. Stratification into low-, medium-, and high-risk groups captured 29%, 37%, and 34%of the cohort, respectively. Median transplant-free survival was 2,450 days in the low-risk group, 1,520 days in the medium-risk group, and 890 days in the high-risk group. Kaplan–Meier curves demonstrated clear separation among all three risk strata (log-rank p < 0.001), confirming robust prognostic discrimination and supporting the model’s potential for guiding timely transplant assessments.
Discussion: Our model demonstrated high discriminative performance, stratifying patients into low-, medium-, and high-risk groups with significantly different median transplant-free survival times. Incorporating novel engineered features alongside traditional laboratory measures shows promise for personalized transplant referral strategies; external validation will be essential to confirm clinical utility.
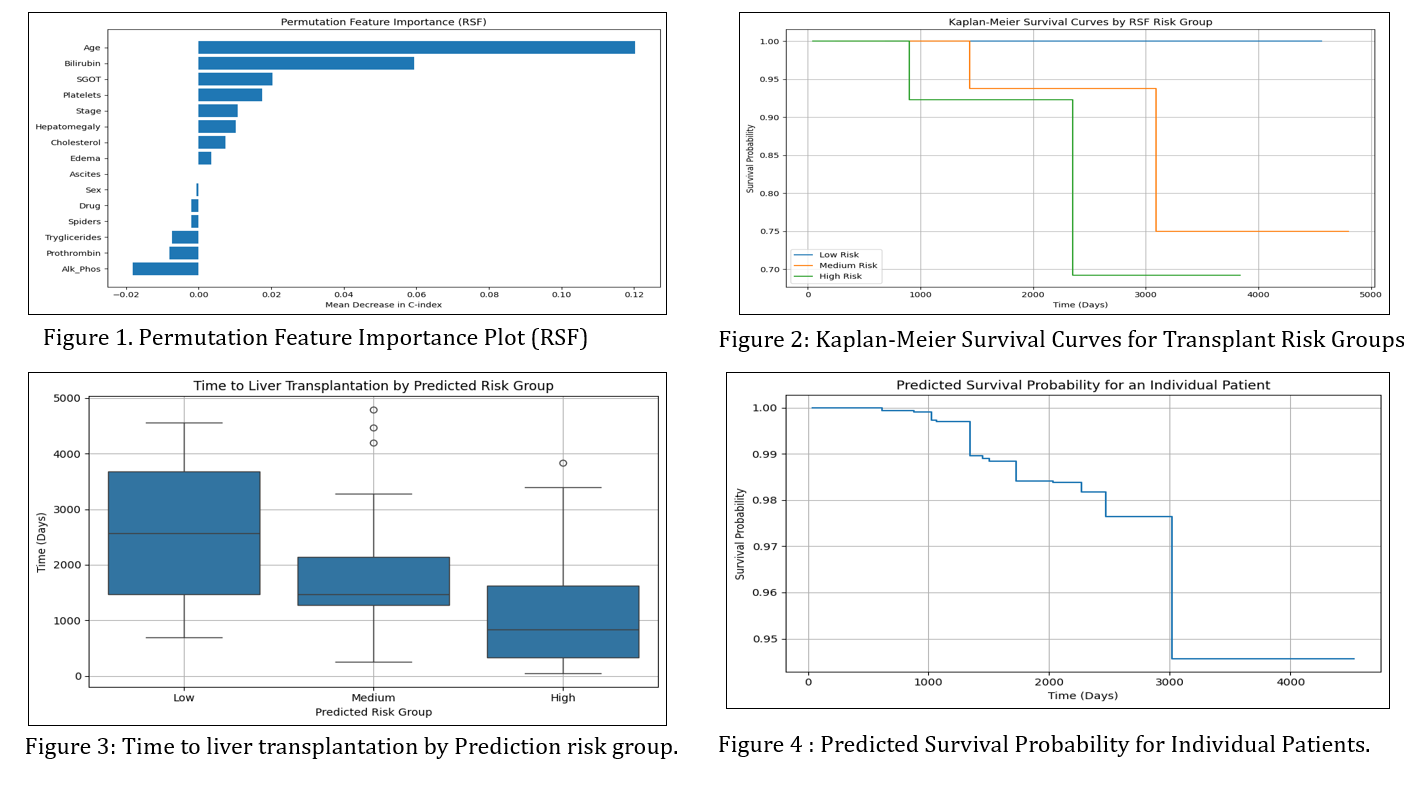
Figure: Figure 1, 2, 3, 4.
Disclosures:
Sri Harsha Boppana indicated no relevant financial relationships.
Manaswitha Thota indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Sachin Sravan Kumar Komati indicated no relevant financial relationships.
Sarath Chandra Ponnada indicated no relevant financial relationships.
Sai Lakshmi Prasanna Komati indicated no relevant financial relationships.
C. David Mintz indicated no relevant financial relationships.
Sri Harsha Boppana, MBBS, MD1, Manaswitha Thota, MD2, Gautam Maddineni, MD3, Sachin Sravan Kumar Komati, 4, Sarath Chandra Ponnada, 5, Sai Lakshmi Prasanna Komati, MBBS6, C. David Mintz, MD, PhD7. P5866 - AI-Based Risk Stratification and Time-to-Transplant Prediction in Cirrhosis Using Random Survival Forest Modeling, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
