Tuesday Poster Session
Category: Liver
P5857 - Unequal Outcomes: Racial Differences in Early Mortality Following Liver Transplantation in the United States (2014-2023)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Boniface Mensah, MBChB, MPh
MedStar Georgetown University Hospital
Baltimore, MD
Presenting Author(s)
Boniface Mensah, MBChB, MPh1, Seunghee Han, MBChB1, Albert E.. Orhin, MBChB, MHS2, Rachel A. Boateng, MBChB3, Simardeep Singh, MBBS1, Ramya Vasireddy, MBBS4, Kevin Eid, MD1, Joseph A. Atarere, MBChB, MPH1, Haider A. Naqvi, MD5
1MedStar Georgetown University Hospital, Baltimore, MD; 2Ascension Saint Agnes Hospital, Baltimore, MD; 3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 4MedStar Health, Baltimore, MD; 5MedStar Franklin Square Medical Center, Baltimore, MD
Introduction: Despite major advances in liver transplantation (LT), disparities in post-transplant outcomes persist, particularly among racially and ethnically minoritized populations. While prior studies have described inequities in access to LT, less is known about whether race independently predicts early post-transplant outcomes in the modern transplant era. This study aims to evaluate contemporary racial disparities in graft outcomes and mortality within one year after LT using a nationally representative database over the last decade.
Methods: We conducted a retrospective cohort study using the United Network for Organ Sharing (UNOS) Standard Transplant Analysis and Research (STAR) database from 2014–2023. Adult patients (≥18 years) who underwent LT were included. Recipient demographics, baseline characteristics, and outcomes including graft rejection, failure, re-transplantation, and 1-year mortality were analyzed by race/ethnicity. Multivariable logistic regression was performed to estimate adjusted odds of death within 1 year, controlling for baseline demographics.
Results: A total of 79,212 LT recipients were included: 71% White, 8% Black, 16% Hispanic, 4% Asian, and 1% American Indian/Alaska Native (AIAN). Black (22.5%), Hispanic (24.9%), and Asian (36.1%) recipients had higher HCC prevalence at transplant. AIAN patients had the highest MELD scores (27.2), while Asian and Hispanic patients experienced the longest wait times (250 and 283 days, respectively). Black recipients had the highest rate of previous LT (6.7%). Graft rejection and failure were most common in Black and AIAN populations, while Asian recipients had the highest rate of re-transplantation (17.8%). One-year mortality was highest among Black (35.1%) and AIAN (29.1%) recipients. After adjustment, Black recipients had 60% higher odds of death at 1 year compared to White recipients which was statistically significant (AOR 1.6; 95% CI: 1.4–1.8).
Discussion: Racial disparities persist in early outcomes after LT, with Black and AIAN recipients experiencing the greatest 1-year mortality. These disparities may reflect differences in disease severity, access to timely care, or post-transplant management. Our findings underscore the urgent need for equity-focused interventions to improve transplant outcomes and eliminate racial disparities in the post-LT setting.
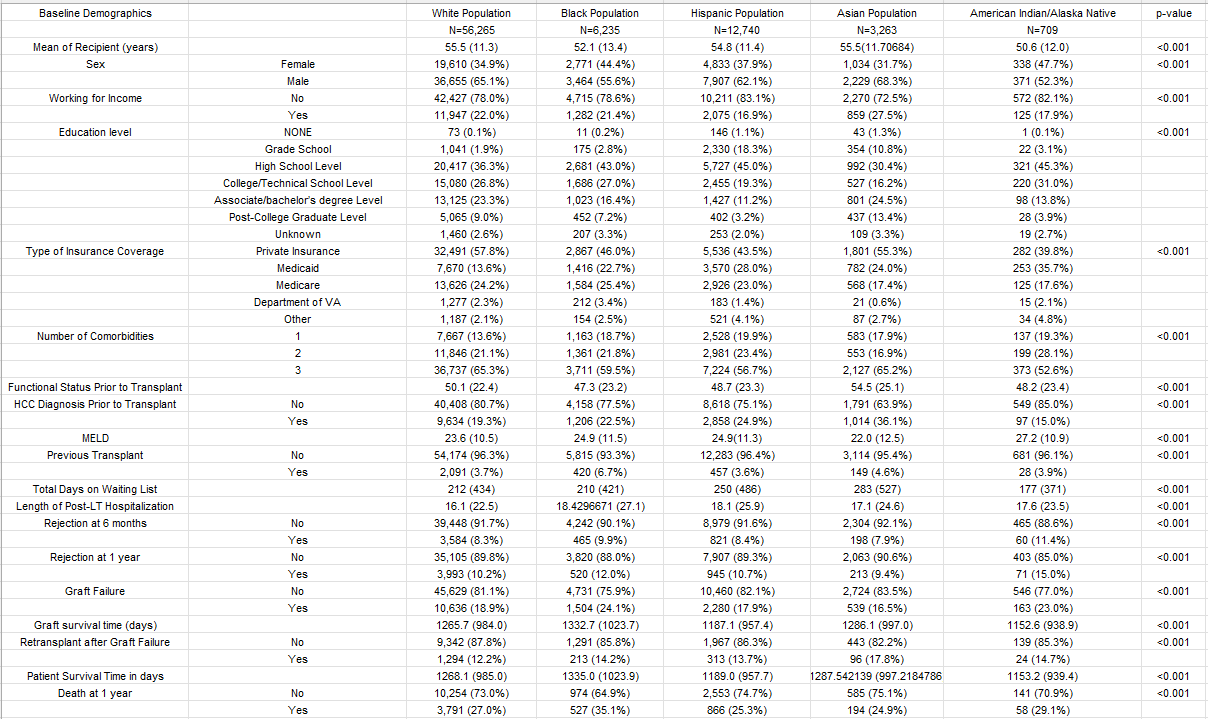
Figure: Baseline Demographics of LT Recipients
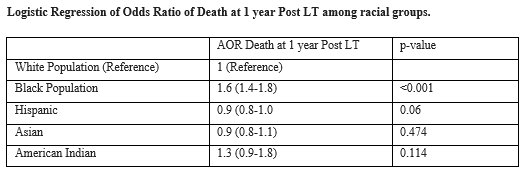
Figure: AOR of Mortality at 1 year after LT among Racial Groups.
Disclosures:
Boniface Mensah indicated no relevant financial relationships.
Seunghee Han indicated no relevant financial relationships.
Albert Orhin indicated no relevant financial relationships.
Rachel Boateng indicated no relevant financial relationships.
Simardeep Singh indicated no relevant financial relationships.
Ramya Vasireddy indicated no relevant financial relationships.
Kevin Eid indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Boniface Mensah, MBChB, MPh1, Seunghee Han, MBChB1, Albert E.. Orhin, MBChB, MHS2, Rachel A. Boateng, MBChB3, Simardeep Singh, MBBS1, Ramya Vasireddy, MBBS4, Kevin Eid, MD1, Joseph A. Atarere, MBChB, MPH1, Haider A. Naqvi, MD5. P5857 - Unequal Outcomes: Racial Differences in Early Mortality Following Liver Transplantation in the United States (2014-2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Baltimore, MD; 2Ascension Saint Agnes Hospital, Baltimore, MD; 3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 4MedStar Health, Baltimore, MD; 5MedStar Franklin Square Medical Center, Baltimore, MD
Introduction: Despite major advances in liver transplantation (LT), disparities in post-transplant outcomes persist, particularly among racially and ethnically minoritized populations. While prior studies have described inequities in access to LT, less is known about whether race independently predicts early post-transplant outcomes in the modern transplant era. This study aims to evaluate contemporary racial disparities in graft outcomes and mortality within one year after LT using a nationally representative database over the last decade.
Methods: We conducted a retrospective cohort study using the United Network for Organ Sharing (UNOS) Standard Transplant Analysis and Research (STAR) database from 2014–2023. Adult patients (≥18 years) who underwent LT were included. Recipient demographics, baseline characteristics, and outcomes including graft rejection, failure, re-transplantation, and 1-year mortality were analyzed by race/ethnicity. Multivariable logistic regression was performed to estimate adjusted odds of death within 1 year, controlling for baseline demographics.
Results: A total of 79,212 LT recipients were included: 71% White, 8% Black, 16% Hispanic, 4% Asian, and 1% American Indian/Alaska Native (AIAN). Black (22.5%), Hispanic (24.9%), and Asian (36.1%) recipients had higher HCC prevalence at transplant. AIAN patients had the highest MELD scores (27.2), while Asian and Hispanic patients experienced the longest wait times (250 and 283 days, respectively). Black recipients had the highest rate of previous LT (6.7%). Graft rejection and failure were most common in Black and AIAN populations, while Asian recipients had the highest rate of re-transplantation (17.8%). One-year mortality was highest among Black (35.1%) and AIAN (29.1%) recipients. After adjustment, Black recipients had 60% higher odds of death at 1 year compared to White recipients which was statistically significant (AOR 1.6; 95% CI: 1.4–1.8).
Discussion: Racial disparities persist in early outcomes after LT, with Black and AIAN recipients experiencing the greatest 1-year mortality. These disparities may reflect differences in disease severity, access to timely care, or post-transplant management. Our findings underscore the urgent need for equity-focused interventions to improve transplant outcomes and eliminate racial disparities in the post-LT setting.
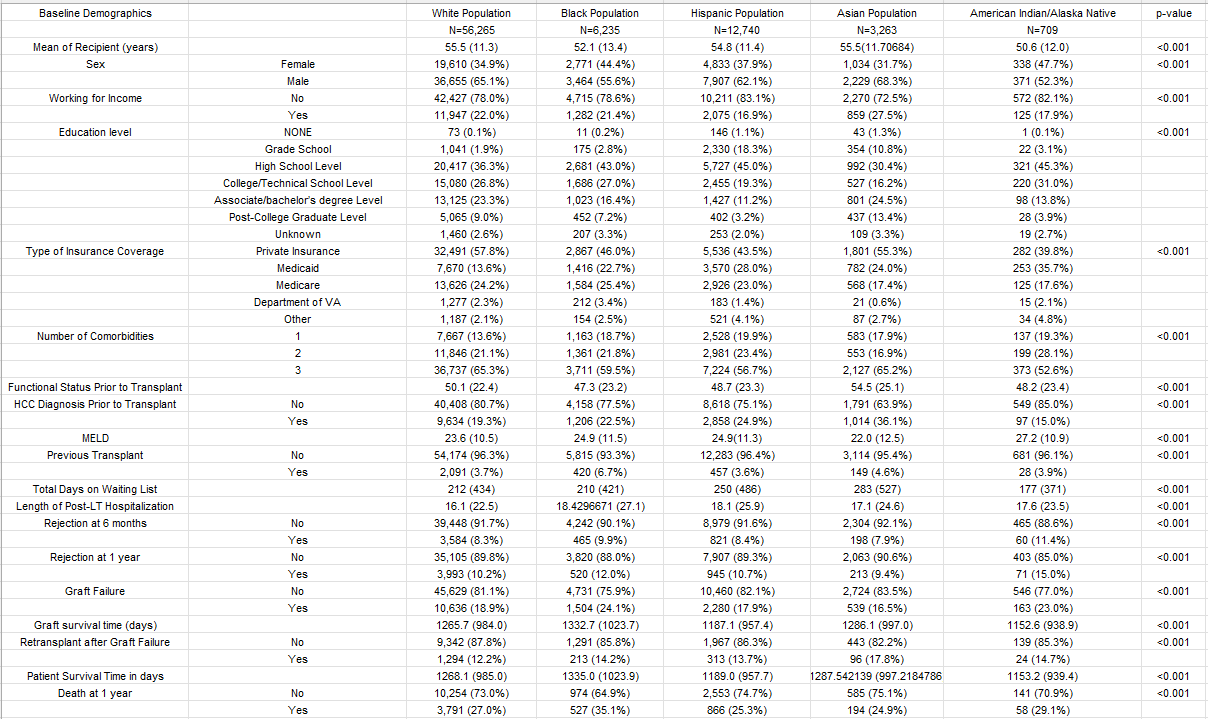
Figure: Baseline Demographics of LT Recipients
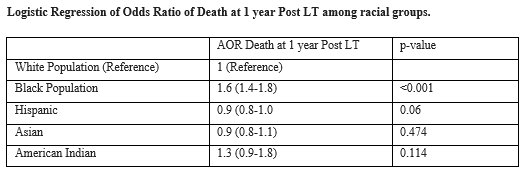
Figure: AOR of Mortality at 1 year after LT among Racial Groups.
Disclosures:
Boniface Mensah indicated no relevant financial relationships.
Seunghee Han indicated no relevant financial relationships.
Albert Orhin indicated no relevant financial relationships.
Rachel Boateng indicated no relevant financial relationships.
Simardeep Singh indicated no relevant financial relationships.
Ramya Vasireddy indicated no relevant financial relationships.
Kevin Eid indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Boniface Mensah, MBChB, MPh1, Seunghee Han, MBChB1, Albert E.. Orhin, MBChB, MHS2, Rachel A. Boateng, MBChB3, Simardeep Singh, MBBS1, Ramya Vasireddy, MBBS4, Kevin Eid, MD1, Joseph A. Atarere, MBChB, MPH1, Haider A. Naqvi, MD5. P5857 - Unequal Outcomes: Racial Differences in Early Mortality Following Liver Transplantation in the United States (2014-2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
