Tuesday Poster Session
Category: Liver
P5841 - Identifying Screening Deficits for MASLD in the Diabetic Population at an Academic Endocrinology Clinic
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AM
Ahila Manivannan, MD (she/her/hers)
Wayne State University School of Medicine / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Ahila Manivannan, MD1, Malek Shatila, MD2, Mazhar Shapoo, MD2, Victor Osio, MD1, Varun Nandamudi, DO1, Ranim Chamseddin, MD1, Bashar Mohamad, MD1
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Detroit Medical Center/Wayne State University, Detroit, MI
Introduction: The incidence of metabolic dysfunction-associated steatotic liver disease (MASLD) is rising and diabetes is a major risk factor. The American Diabetes Association has implemented screening guidelines for MASLD in diabetics with screening tools such as the Fibrosis-4 (FIB-4) score. Screening these patients for MASLD is crucial to improving outcomes. This quality improvement (QI) project aims to identify deficits in screening at our academic endocrinology clinic and examine the clinical variables that may impact the FIB-4 score.
Methods: In this initial phase, we included a random sample of 200 diabetic patients from the Wayne Health Endocrinology clinic who had liver enzymes and complete blood counts (CBC) recorded in the past 12 months. A FIB-4 score was calculated to identify those at risk for F2 or greater fibrosis (advanced fibrosis), defined as a FIB-4 >1.3. We collected demographic data, diabetes-related variables including hemoglobin A1c (HbA1c), insulin and glucose-like peptide 1 (GLP-1) agonist use, and available liver imaging. An educational session was provided to the endocrinology department focusing on MASLD screening, FIB-4 calculation, and appropriate referrals for Fibroscans.
Results: Demographic information is summarized in Table 1, and our analysis is summarized in Table 2. Among the 200 patients in our initial cohort, the mean FIB-4 score was 1.15. 68 (34%) patients were at risk for advanced fibrosis (mean FIB-4 of 1.9). BMI >30 was associated with higher FIB4 (mean 1.28 v. 1.06; p=0.017), as was type 2 diabetes (mean 0.75 in type 1 v. 1.2 in type 2; p=0.004). GLP-1 agonist use was associated with lower FIB-4 (p=0.012), with 11.1% of patients on GLP-1 agonists at risk for advanced fibrosis compared to 31.4% of patients not on them (p=0.03). Only 2 (2.9%) patients at risk for advanced fibrosis had Fibroscans.
Discussion: Our findings highlight a significant gap in MASLD screening within our diabetic population, with only 3% at risk for advanced fibrosis on FIB-4 testing undergoing Fibroscan testing. Contributing factors include a lack of provider awareness regarding this testing and a lack of institutional screening algorithms. GLP-1 agonist use was associated with a lower FIB-4, likely due to its weight loss effects. Type 2 diabetics likely had higher FIB-4 scores than type 1 diabetics due to their link to metabolic dysfunction. Future QI steps include tracking FIB-4 calculation rates, appropriate Fibroscan orders, and gastroenterology referrals for advanced fibrosis.
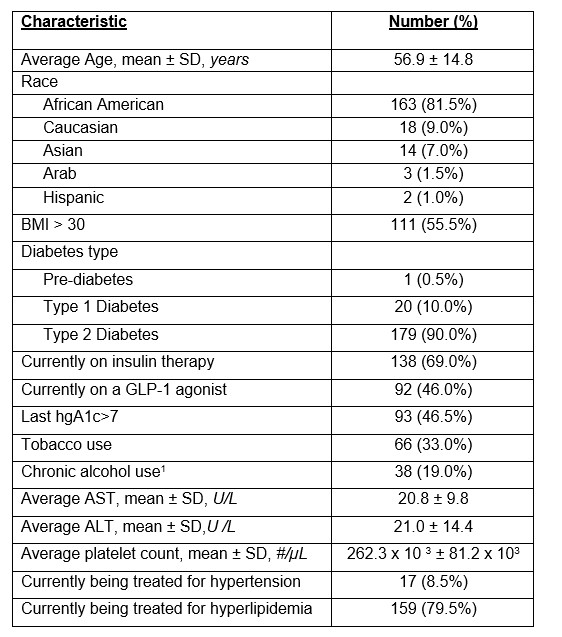
Figure: Table 1: Patient characteristics of initial cohort. Abbreviations: ALT - Alanine aminotransferase; AST - Aspartate aminotransferase; BMI – body mass index; GLP-1 agonists – glucose-like peptide 1 agonists; SD – standard deviation. 1 - Chronic alcohol use refers to >7 standard drinks/week for women; > 14 standard drinks/week for men
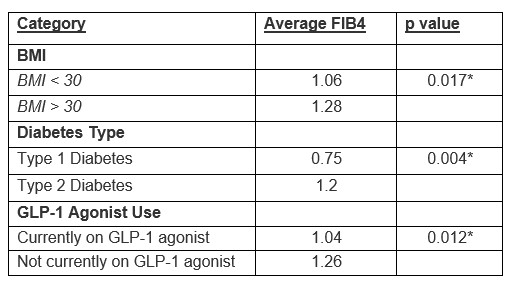
Figure: Table 2: Comparing the Average FIB4 Score Based on BMI, Diabetes Type, and GLP-1 Agonist Use. Abbreviations: BMI – Body Mass Index; FIB4 – Fibrosis4 score; GLP-1 agonists – Glucose-like peptide 1 agonists. *Significant at p<0.05.
Disclosures:
Ahila Manivannan indicated no relevant financial relationships.
Malek Shatila indicated no relevant financial relationships.
Mazhar Shapoo indicated no relevant financial relationships.
Victor Osio indicated no relevant financial relationships.
Varun Nandamudi indicated no relevant financial relationships.
Ranim Chamseddin indicated no relevant financial relationships.
Bashar Mohamad indicated no relevant financial relationships.
Ahila Manivannan, MD1, Malek Shatila, MD2, Mazhar Shapoo, MD2, Victor Osio, MD1, Varun Nandamudi, DO1, Ranim Chamseddin, MD1, Bashar Mohamad, MD1. P5841 - Identifying Screening Deficits for MASLD in the Diabetic Population at an Academic Endocrinology Clinic, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Detroit Medical Center/Wayne State University, Detroit, MI
Introduction: The incidence of metabolic dysfunction-associated steatotic liver disease (MASLD) is rising and diabetes is a major risk factor. The American Diabetes Association has implemented screening guidelines for MASLD in diabetics with screening tools such as the Fibrosis-4 (FIB-4) score. Screening these patients for MASLD is crucial to improving outcomes. This quality improvement (QI) project aims to identify deficits in screening at our academic endocrinology clinic and examine the clinical variables that may impact the FIB-4 score.
Methods: In this initial phase, we included a random sample of 200 diabetic patients from the Wayne Health Endocrinology clinic who had liver enzymes and complete blood counts (CBC) recorded in the past 12 months. A FIB-4 score was calculated to identify those at risk for F2 or greater fibrosis (advanced fibrosis), defined as a FIB-4 >1.3. We collected demographic data, diabetes-related variables including hemoglobin A1c (HbA1c), insulin and glucose-like peptide 1 (GLP-1) agonist use, and available liver imaging. An educational session was provided to the endocrinology department focusing on MASLD screening, FIB-4 calculation, and appropriate referrals for Fibroscans.
Results: Demographic information is summarized in Table 1, and our analysis is summarized in Table 2. Among the 200 patients in our initial cohort, the mean FIB-4 score was 1.15. 68 (34%) patients were at risk for advanced fibrosis (mean FIB-4 of 1.9). BMI >30 was associated with higher FIB4 (mean 1.28 v. 1.06; p=0.017), as was type 2 diabetes (mean 0.75 in type 1 v. 1.2 in type 2; p=0.004). GLP-1 agonist use was associated with lower FIB-4 (p=0.012), with 11.1% of patients on GLP-1 agonists at risk for advanced fibrosis compared to 31.4% of patients not on them (p=0.03). Only 2 (2.9%) patients at risk for advanced fibrosis had Fibroscans.
Discussion: Our findings highlight a significant gap in MASLD screening within our diabetic population, with only 3% at risk for advanced fibrosis on FIB-4 testing undergoing Fibroscan testing. Contributing factors include a lack of provider awareness regarding this testing and a lack of institutional screening algorithms. GLP-1 agonist use was associated with a lower FIB-4, likely due to its weight loss effects. Type 2 diabetics likely had higher FIB-4 scores than type 1 diabetics due to their link to metabolic dysfunction. Future QI steps include tracking FIB-4 calculation rates, appropriate Fibroscan orders, and gastroenterology referrals for advanced fibrosis.
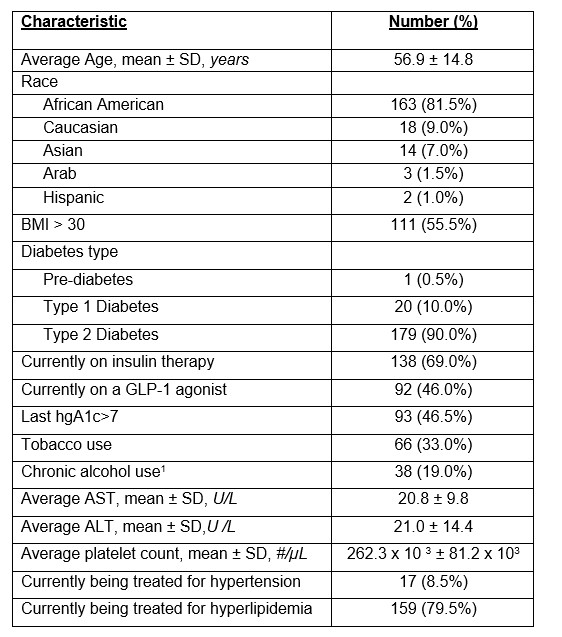
Figure: Table 1: Patient characteristics of initial cohort. Abbreviations: ALT - Alanine aminotransferase; AST - Aspartate aminotransferase; BMI – body mass index; GLP-1 agonists – glucose-like peptide 1 agonists; SD – standard deviation. 1 - Chronic alcohol use refers to >7 standard drinks/week for women; > 14 standard drinks/week for men
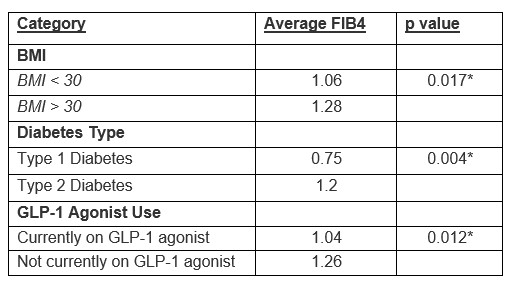
Figure: Table 2: Comparing the Average FIB4 Score Based on BMI, Diabetes Type, and GLP-1 Agonist Use. Abbreviations: BMI – Body Mass Index; FIB4 – Fibrosis4 score; GLP-1 agonists – Glucose-like peptide 1 agonists. *Significant at p<0.05.
Disclosures:
Ahila Manivannan indicated no relevant financial relationships.
Malek Shatila indicated no relevant financial relationships.
Mazhar Shapoo indicated no relevant financial relationships.
Victor Osio indicated no relevant financial relationships.
Varun Nandamudi indicated no relevant financial relationships.
Ranim Chamseddin indicated no relevant financial relationships.
Bashar Mohamad indicated no relevant financial relationships.
Ahila Manivannan, MD1, Malek Shatila, MD2, Mazhar Shapoo, MD2, Victor Osio, MD1, Varun Nandamudi, DO1, Ranim Chamseddin, MD1, Bashar Mohamad, MD1. P5841 - Identifying Screening Deficits for MASLD in the Diabetic Population at an Academic Endocrinology Clinic, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
