Tuesday Poster Session
Category: Liver
P5831 - Beyond Obstructive Sleep Apnea: Elevated Odds of Diverse Sleep Disorders in Metabolic Dysfunction-Associated Steatotic Liver Disease -- A Large-Scale US Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AS
Arshia Sethi
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Arshia Sethi, 1, Rishi Chowdhary, MD2, Megh Patel, MBBS3, Samiksha Jain, MBBS4, Prachi Dawer, MBBS5, Venkata Sunkesula, MD2
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3B.J. Medical College, Ahmedabad, Gujarat, India; 4Guntur Medical College, India, Guntur, Andhra Pradesh, India; 5University College of Medical Sciences, New Delhi, Delhi, India
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is a globally prevalent condition with systemic implications. While its association with obstructive sleep apnea is recognized, the broader burden of sleep disorders—especially across sexes—remains poorly characterized. We aimed to evaluate the odds of developing major sleep disorder categories among MASLD patients and examine sex-based variations using a nationally representative dataset.
Methods: We conducted a retrospective cohort study using the TriNetX U.S. Collaborative Network. Adults (≥18 years) diagnosed with imaging-confirmed MASLD (ICD-10: K75.81, K76.0) between 2010–2020 were identified. Patients with pre-existing sleep disorders or confounding neurologic/psychiatric conditions were excluded. MASLD patients (n=175,952) were 1:1 propensity score-matched to liver disease–free controls based on demographics, metabolic comorbidities, and healthcare access variables. Sex-stratified analysis was performed on matched male and female MASLD cohorts (n=67,694 each). Odds ratios (OR) with 95% confidence intervals (CI) were calculated for six predefined sleep disorder categories.
Results: MASLD was associated with significantly increased odds of multiple sleep disorders. Compared to controls, MASLD patients had higher odds of sleep-disordered breathing (OR 1.59; 95% CI, 1.54–1.64), insomnia spectrum disorders (OR 1.33; 95% CI, 1.26–1.39), circadian rhythm disorders (OR 1.79; 95% CI, 1.49–2.16), movement-related sleep disorders (OR 1.39; 95% CI, 1.28–1.51), and parasomnias (OR 1.52; 95% CI, 1.16–1.98). No significant association was found with hypersomnia (OR 1.13; 95% CI, 0.78–1.64). Among MASLD patients, males had higher odds of sleep-disordered breathing (OR 1.73; 95% CI, 1.65–1.81), circadian rhythm disorders (OR 1.36; 95% CI, 1.03–1.78), and parasomnias (OR 1.82; 95% CI, 1.19–2.78). Females had greater odds of insomnia (OR 0.88; 95% CI, 0.82–0.95) and movement-related sleep disorders (OR 0.82; 95% CI, 0.72–0.92). No sex-based difference was observed for hypersomnia (OR 0.91; 95% CI, 0.50–1.67).
Discussion: MASLD is independently associated with increased odds of a broad range of sleep disorders beyond obstructive sleep apnea. Sex-based differences suggest males are more prone to breathing and parasomnia-related issues, while females are more affected by insomnia and movement-related disorders. These findings highlight the need for integrated and sex-specific sleep assessments in MASLD management.
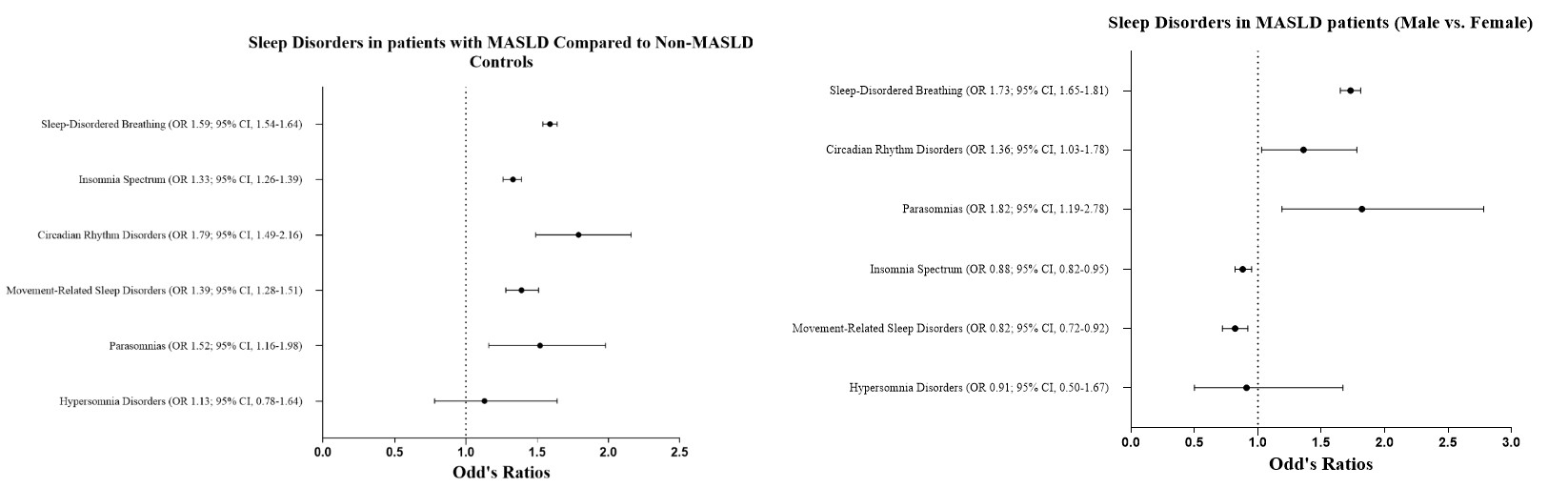
Figure: Sleep disorder in patients with MASLD versus controls and in males versus females
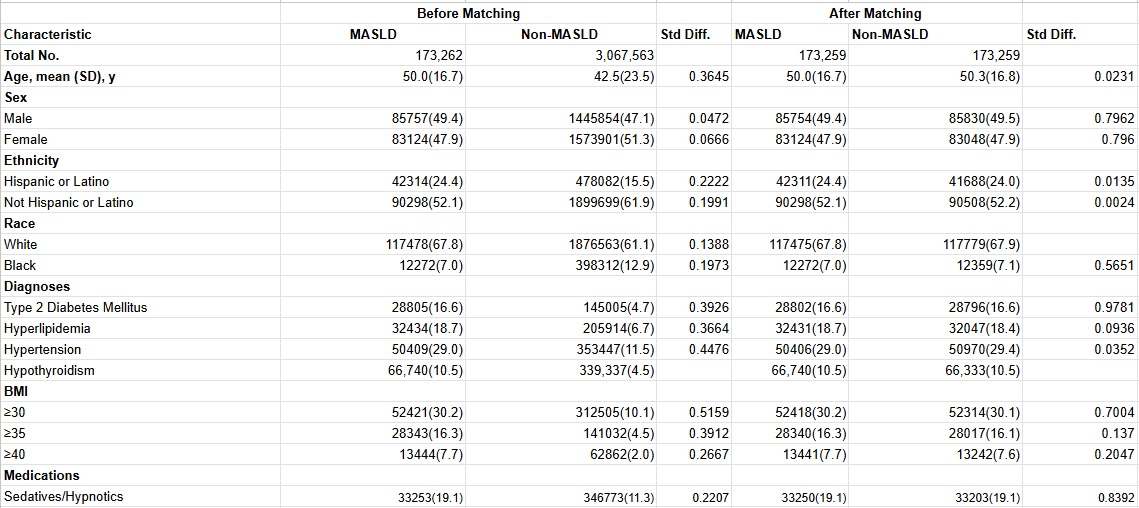
Figure: Baseline demographics, Co-morbidities , and BMI in patients with and without MASLD before and after propensity score matching.
Disclosures:
Arshia Sethi indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Megh Patel indicated no relevant financial relationships.
Samiksha Jain indicated no relevant financial relationships.
Prachi Dawer indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Arshia Sethi, 1, Rishi Chowdhary, MD2, Megh Patel, MBBS3, Samiksha Jain, MBBS4, Prachi Dawer, MBBS5, Venkata Sunkesula, MD2. P5831 - Beyond Obstructive Sleep Apnea: Elevated Odds of Diverse Sleep Disorders in Metabolic Dysfunction-Associated Steatotic Liver Disease -- A Large-Scale US Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3B.J. Medical College, Ahmedabad, Gujarat, India; 4Guntur Medical College, India, Guntur, Andhra Pradesh, India; 5University College of Medical Sciences, New Delhi, Delhi, India
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is a globally prevalent condition with systemic implications. While its association with obstructive sleep apnea is recognized, the broader burden of sleep disorders—especially across sexes—remains poorly characterized. We aimed to evaluate the odds of developing major sleep disorder categories among MASLD patients and examine sex-based variations using a nationally representative dataset.
Methods: We conducted a retrospective cohort study using the TriNetX U.S. Collaborative Network. Adults (≥18 years) diagnosed with imaging-confirmed MASLD (ICD-10: K75.81, K76.0) between 2010–2020 were identified. Patients with pre-existing sleep disorders or confounding neurologic/psychiatric conditions were excluded. MASLD patients (n=175,952) were 1:1 propensity score-matched to liver disease–free controls based on demographics, metabolic comorbidities, and healthcare access variables. Sex-stratified analysis was performed on matched male and female MASLD cohorts (n=67,694 each). Odds ratios (OR) with 95% confidence intervals (CI) were calculated for six predefined sleep disorder categories.
Results: MASLD was associated with significantly increased odds of multiple sleep disorders. Compared to controls, MASLD patients had higher odds of sleep-disordered breathing (OR 1.59; 95% CI, 1.54–1.64), insomnia spectrum disorders (OR 1.33; 95% CI, 1.26–1.39), circadian rhythm disorders (OR 1.79; 95% CI, 1.49–2.16), movement-related sleep disorders (OR 1.39; 95% CI, 1.28–1.51), and parasomnias (OR 1.52; 95% CI, 1.16–1.98). No significant association was found with hypersomnia (OR 1.13; 95% CI, 0.78–1.64). Among MASLD patients, males had higher odds of sleep-disordered breathing (OR 1.73; 95% CI, 1.65–1.81), circadian rhythm disorders (OR 1.36; 95% CI, 1.03–1.78), and parasomnias (OR 1.82; 95% CI, 1.19–2.78). Females had greater odds of insomnia (OR 0.88; 95% CI, 0.82–0.95) and movement-related sleep disorders (OR 0.82; 95% CI, 0.72–0.92). No sex-based difference was observed for hypersomnia (OR 0.91; 95% CI, 0.50–1.67).
Discussion: MASLD is independently associated with increased odds of a broad range of sleep disorders beyond obstructive sleep apnea. Sex-based differences suggest males are more prone to breathing and parasomnia-related issues, while females are more affected by insomnia and movement-related disorders. These findings highlight the need for integrated and sex-specific sleep assessments in MASLD management.
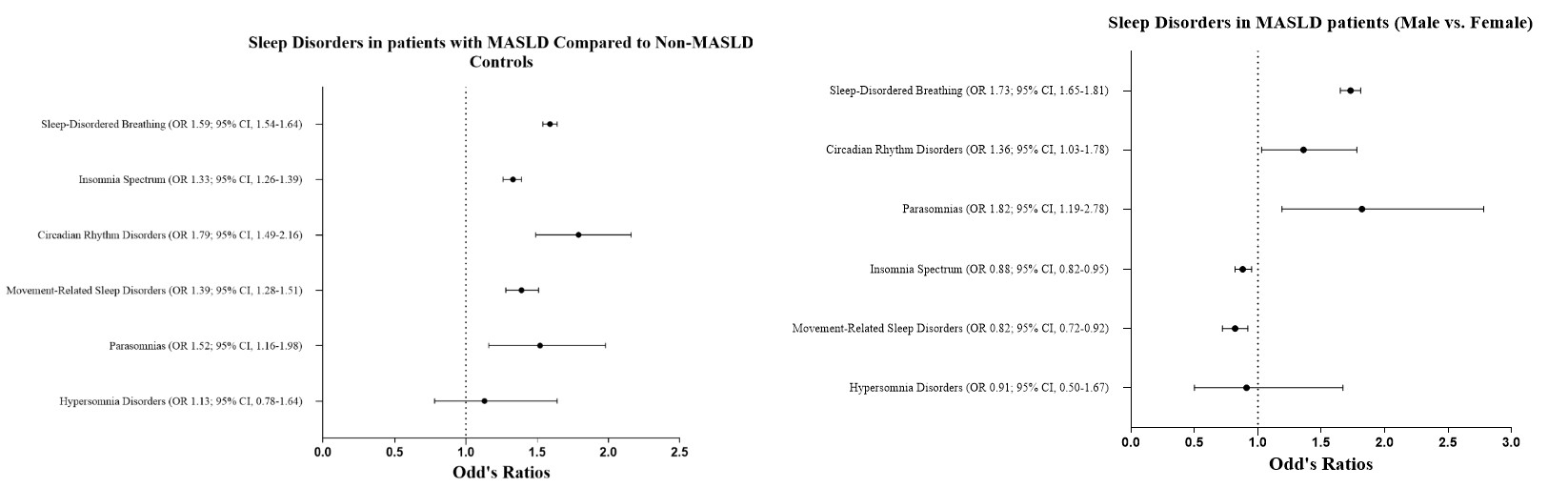
Figure: Sleep disorder in patients with MASLD versus controls and in males versus females
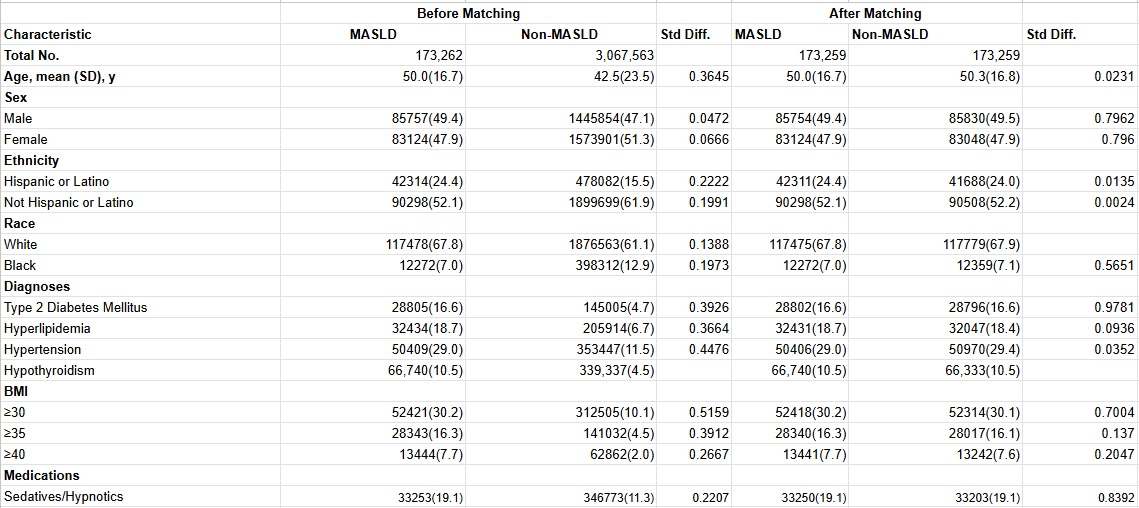
Figure: Baseline demographics, Co-morbidities , and BMI in patients with and without MASLD before and after propensity score matching.
Disclosures:
Arshia Sethi indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Megh Patel indicated no relevant financial relationships.
Samiksha Jain indicated no relevant financial relationships.
Prachi Dawer indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Arshia Sethi, 1, Rishi Chowdhary, MD2, Megh Patel, MBBS3, Samiksha Jain, MBBS4, Prachi Dawer, MBBS5, Venkata Sunkesula, MD2. P5831 - Beyond Obstructive Sleep Apnea: Elevated Odds of Diverse Sleep Disorders in Metabolic Dysfunction-Associated Steatotic Liver Disease -- A Large-Scale US Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
