Tuesday Poster Session
Category: Liver
P5788 - The Impact of Obstructive Sleep Apnea on Hospitalized Patients With Metabolic Dysfunction-Associated Steatotic Liver Disease: Insights From a Nationwide Cohort
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shivangini Duggal, MD
Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA
El Paso, TX
Presenting Author(s)
Shivangini Duggal, MD1, Sakar Khattar, MS2, Lakshmi Kattamuri, MD3, Adderly Toribio de Jesus, MD4, Alejandro Robles, MD5, Marc J. Zuckerman, MD4, Sherif E. Elhanafi, MD3
1Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 2Google Inc., Santa Clara, CA; 3Texas Tech University Health Sciences Center, El Paso, TX; 4Division of Gastroenterology, Department of Internal Medicine, Texas Tech University Health Sciences Center, El Paso, TX., El Paso, TX; 5Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX
Introduction: Obstructive sleep apnea syndrome (OSA) has been increasingly recognized as a key comorbidity in metabolic dysfunction-associated steatotic liver disease (MASLD). OSA contributes to systemic inflammation, insulin resistance, endothelial dysfunction, and sympathetic overactivation, all of which may impact hepatic and cardiovascular outcomes. However, literature evaluating the interplay of OSA and MASLD remains limited. The aim of this study was to evaluate the impact of OSA in MASLD patients using large-scale real-world data.
Methods: We analyzed the Nationwide Inpatient Sample database from 2012 to 2021, identifying adult hospitalizations with MASLD using ICD-9/10-CM codes. Patients were stratified by the presence of OSA. Demographics, comorbidities, and clinical outcomes were compared between groups using appropriate statistical tests using R software.
Results: Among 6,331,909 MASLD hospitalizations, 1,015,555 (16.0%) had concomitant OSA. Compared to non-OSA group, patients with MASLD in OSA group had slightly older age (median age 62 vs 61 years; p< 0.001) and a higher proportion of males (50.8% vs 47.0%; p< 0.001). The OSA group demonstrated significantly higher rates of diabetes (31.5% vs 23.9%), hypertension (66.7% vs 56.8%), acute coronary syndrome (23.3% vs 16.5%), chronic kidney disease (23.0% vs 18.9%), arrhythmias (25.1% vs 17.0%), venous thromboembolism (9.3% vs 7.2%), anxiety (20.4% vs 14.8%), and depression (21.4% vs 14.0%) (all p< 0.001). Additionally, OSA patients had lower rates of acute liver failure (8.1% vs 10.7%), alcohol use (4.2% vs 10.1%), mechanical ventilation (4.1% vs 4.6%), and liver transplantation (0.16% vs 0.21%). Despite their higher comorbidity burden, OSA patients experienced lower in-hospital mortality (2.6% vs 3.7%; p< 0.001), shorter length of stay (median 4 vs 4 days; p< 0.001), and slightly reduced hospitalization charges (median $41,755 vs $39,166; p< 0.001) (Table 1).
Discussion: While MASLD patients with OSA exhibited a heavier cardiometabolic burden, they paradoxically had lower inpatient mortality. This may reflect earlier detection, more aggressive management, or adaptive responses to intermittent hypoxia that blunt acute illness severity. Alternatively, OSA may serve as a marker for heightened healthcare engagement. These findings highlight the need for longitudinal studies to elucidate the interplay between OSA, MASLD progression, and outcomes.
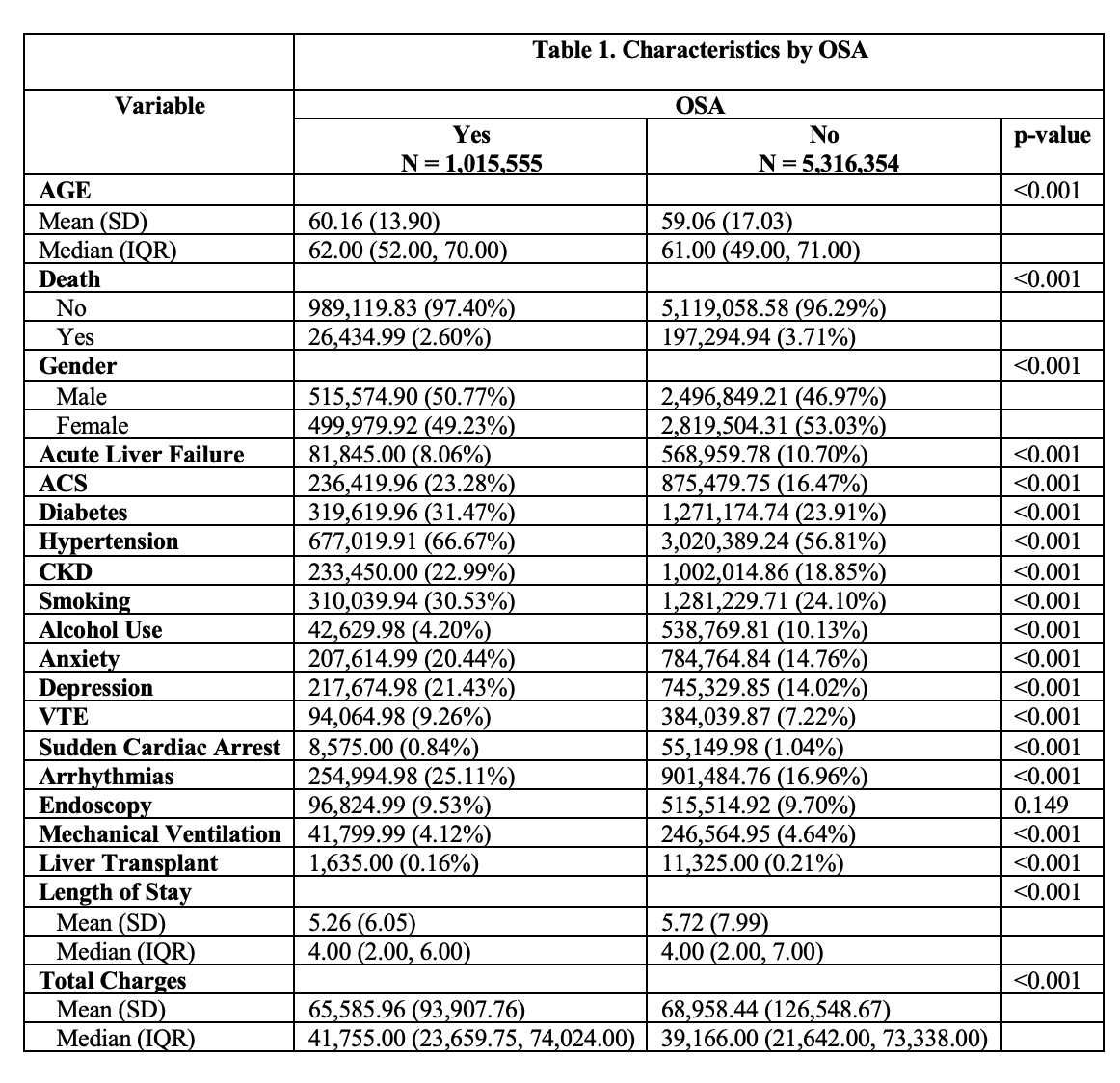
Figure: Table 1. Describes the characteristics of patients with and without OSA.
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Sakar Khattar indicated no relevant financial relationships.
Lakshmi Kattamuri indicated no relevant financial relationships.
Adderly Toribio de Jesus indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Marc Zuckerman indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Shivangini Duggal, MD1, Sakar Khattar, MS2, Lakshmi Kattamuri, MD3, Adderly Toribio de Jesus, MD4, Alejandro Robles, MD5, Marc J. Zuckerman, MD4, Sherif E. Elhanafi, MD3. P5788 - The Impact of Obstructive Sleep Apnea on Hospitalized Patients With Metabolic Dysfunction-Associated Steatotic Liver Disease: Insights From a Nationwide Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 2Google Inc., Santa Clara, CA; 3Texas Tech University Health Sciences Center, El Paso, TX; 4Division of Gastroenterology, Department of Internal Medicine, Texas Tech University Health Sciences Center, El Paso, TX., El Paso, TX; 5Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX
Introduction: Obstructive sleep apnea syndrome (OSA) has been increasingly recognized as a key comorbidity in metabolic dysfunction-associated steatotic liver disease (MASLD). OSA contributes to systemic inflammation, insulin resistance, endothelial dysfunction, and sympathetic overactivation, all of which may impact hepatic and cardiovascular outcomes. However, literature evaluating the interplay of OSA and MASLD remains limited. The aim of this study was to evaluate the impact of OSA in MASLD patients using large-scale real-world data.
Methods: We analyzed the Nationwide Inpatient Sample database from 2012 to 2021, identifying adult hospitalizations with MASLD using ICD-9/10-CM codes. Patients were stratified by the presence of OSA. Demographics, comorbidities, and clinical outcomes were compared between groups using appropriate statistical tests using R software.
Results: Among 6,331,909 MASLD hospitalizations, 1,015,555 (16.0%) had concomitant OSA. Compared to non-OSA group, patients with MASLD in OSA group had slightly older age (median age 62 vs 61 years; p< 0.001) and a higher proportion of males (50.8% vs 47.0%; p< 0.001). The OSA group demonstrated significantly higher rates of diabetes (31.5% vs 23.9%), hypertension (66.7% vs 56.8%), acute coronary syndrome (23.3% vs 16.5%), chronic kidney disease (23.0% vs 18.9%), arrhythmias (25.1% vs 17.0%), venous thromboembolism (9.3% vs 7.2%), anxiety (20.4% vs 14.8%), and depression (21.4% vs 14.0%) (all p< 0.001). Additionally, OSA patients had lower rates of acute liver failure (8.1% vs 10.7%), alcohol use (4.2% vs 10.1%), mechanical ventilation (4.1% vs 4.6%), and liver transplantation (0.16% vs 0.21%). Despite their higher comorbidity burden, OSA patients experienced lower in-hospital mortality (2.6% vs 3.7%; p< 0.001), shorter length of stay (median 4 vs 4 days; p< 0.001), and slightly reduced hospitalization charges (median $41,755 vs $39,166; p< 0.001) (Table 1).
Discussion: While MASLD patients with OSA exhibited a heavier cardiometabolic burden, they paradoxically had lower inpatient mortality. This may reflect earlier detection, more aggressive management, or adaptive responses to intermittent hypoxia that blunt acute illness severity. Alternatively, OSA may serve as a marker for heightened healthcare engagement. These findings highlight the need for longitudinal studies to elucidate the interplay between OSA, MASLD progression, and outcomes.
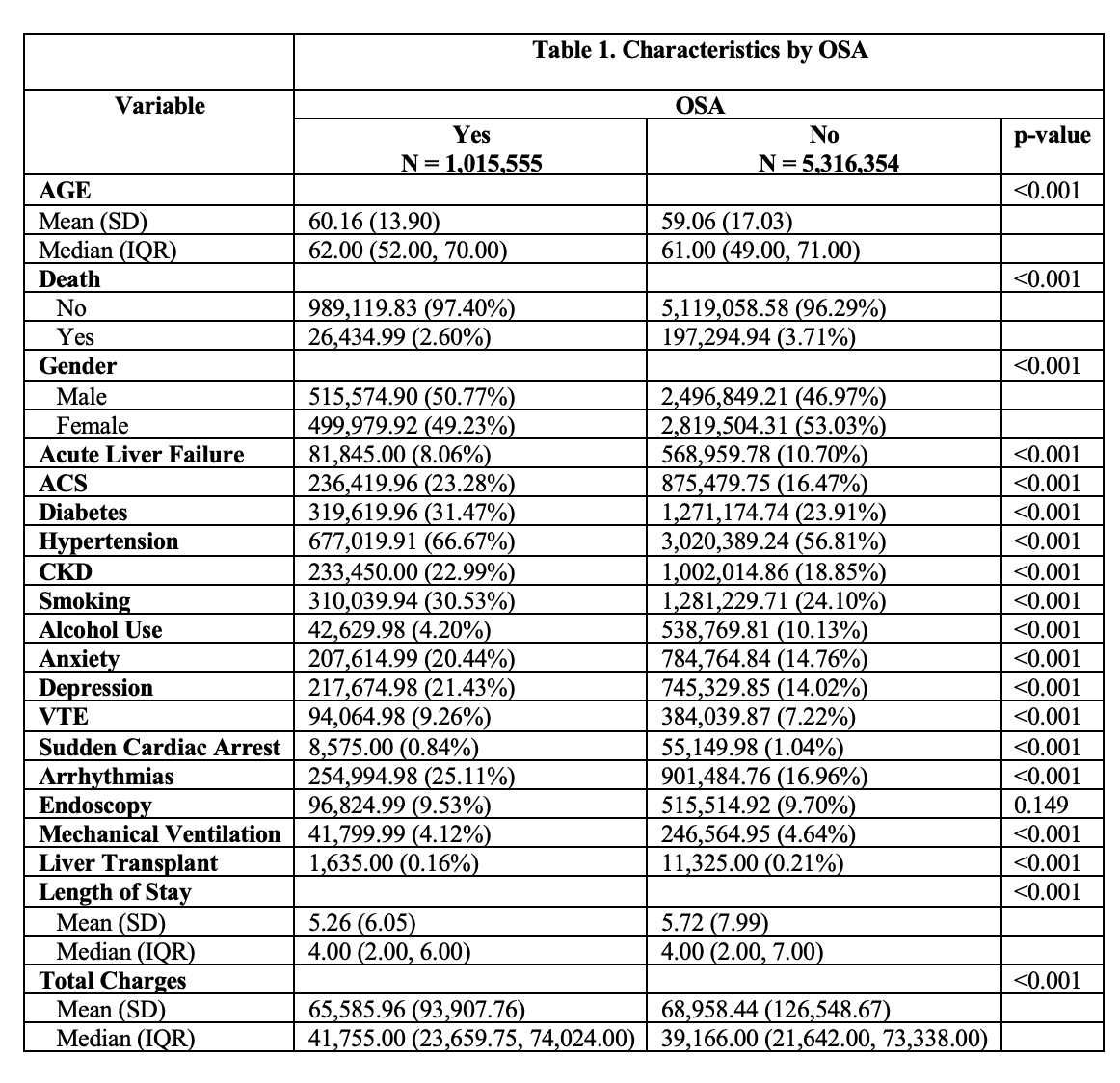
Figure: Table 1. Describes the characteristics of patients with and without OSA.
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Sakar Khattar indicated no relevant financial relationships.
Lakshmi Kattamuri indicated no relevant financial relationships.
Adderly Toribio de Jesus indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Marc Zuckerman indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Shivangini Duggal, MD1, Sakar Khattar, MS2, Lakshmi Kattamuri, MD3, Adderly Toribio de Jesus, MD4, Alejandro Robles, MD5, Marc J. Zuckerman, MD4, Sherif E. Elhanafi, MD3. P5788 - The Impact of Obstructive Sleep Apnea on Hospitalized Patients With Metabolic Dysfunction-Associated Steatotic Liver Disease: Insights From a Nationwide Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
