Tuesday Poster Session
Category: Liver
P5787 - Exploring the Relationship Between Cirrhotic Cardiomyopathy Development and Portal Hypertension
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shivangini Duggal, MD
Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA
El Paso, TX
Presenting Author(s)
Shivangini Duggal, MD1, Lakshmi Kattamuri, MD2, Michael J. Brockman, DO2, Mutaz Kalas, MD3, Swati Mahapatra, DO4, Keith Garrison, MD2, Sherif E. Elhanafi, MD2, Alejandro Robles, MD5
1Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 4Texas A&M, El Paso, TX; 5Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX
Introduction: Cirrhotic cardiomyopathy (CCM) is a subclinical cardiac dysfunction increasingly recognized in cirrhotic patients. Characterized by impaired systolic reserve, diastolic dysfunction, and electrophysiological abnormalities, CCM may contribute to the development of portal hypertension and its complications. This study evaluates the relationship between transthoracic echocardiographic (TTE) findings and portal hypertensive manifestations observed on esophagogastroduodenoscopy (EGD).
Methods: We retrospectively analyzed 94 patients with CCM at University Medical Center in El Paso (2014–2024) who underwent both TTE and EGD. Key demographic, echocardiographic, endoscopic, and liver disease severity data (FIB-4, MELD) were extracted.
Results: Among 94 patients (mean age 53.9±16.4 years; 57.4% female; 98.9% Hispanic), the leading etiologies were alcoholic liver disease (34%), hepatitis C (23.4%), NASH (17%), and autoimmune hepatitis (20.2%) (Table 1). EGD revealed esophageal varices in 70% (primarily Grade I–II) and portal gastropathy in 17%. Ascites (84%) and hepatic encephalopathy (61.7%) were common. TTE showed mean LVEF 49.7±20.8%, RVSP 33.6±12 mmHg, and TAPSE 1.77±0.75 cm. ALT correlated strongly with RVSP (r=0.675, p< 0.001), while AST correlated with PA max PG (r=0.230, p=0.041) (Table 2). MELD, Child-Pugh, and FIB-4 showed limited correlation with echocardiographic measures, suggesting subclinical cardiac dysfunction may precede hepatic decompensation.
Discussion: Echocardiographic features of CCM correlate with portal hypertension severity. Routine cardiac assessment may improve risk stratification and guide earlier interventions in cirrhosis. Incorporating echocardiographic evaluation into standard cirrhosis care may help identify high-risk patients before overt cardiac symptoms develop.
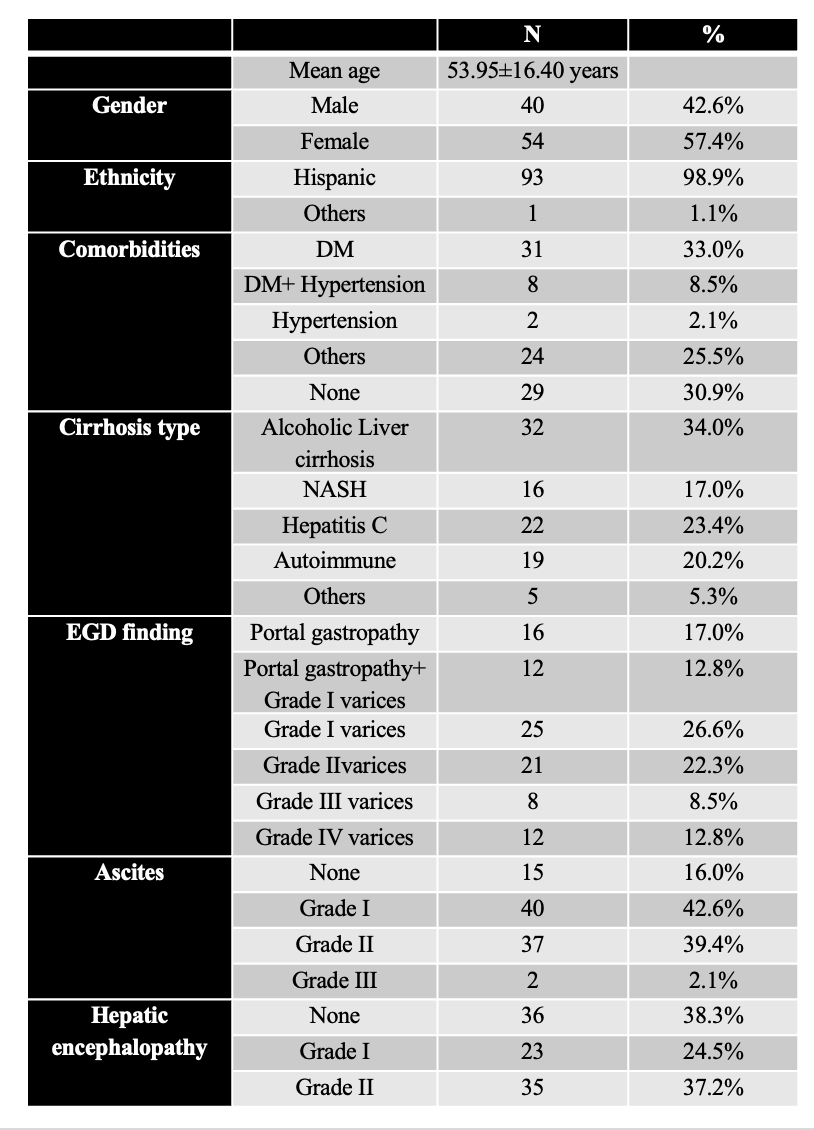
Figure: Table 1: Baseline characteristics in study subjects (n=94)
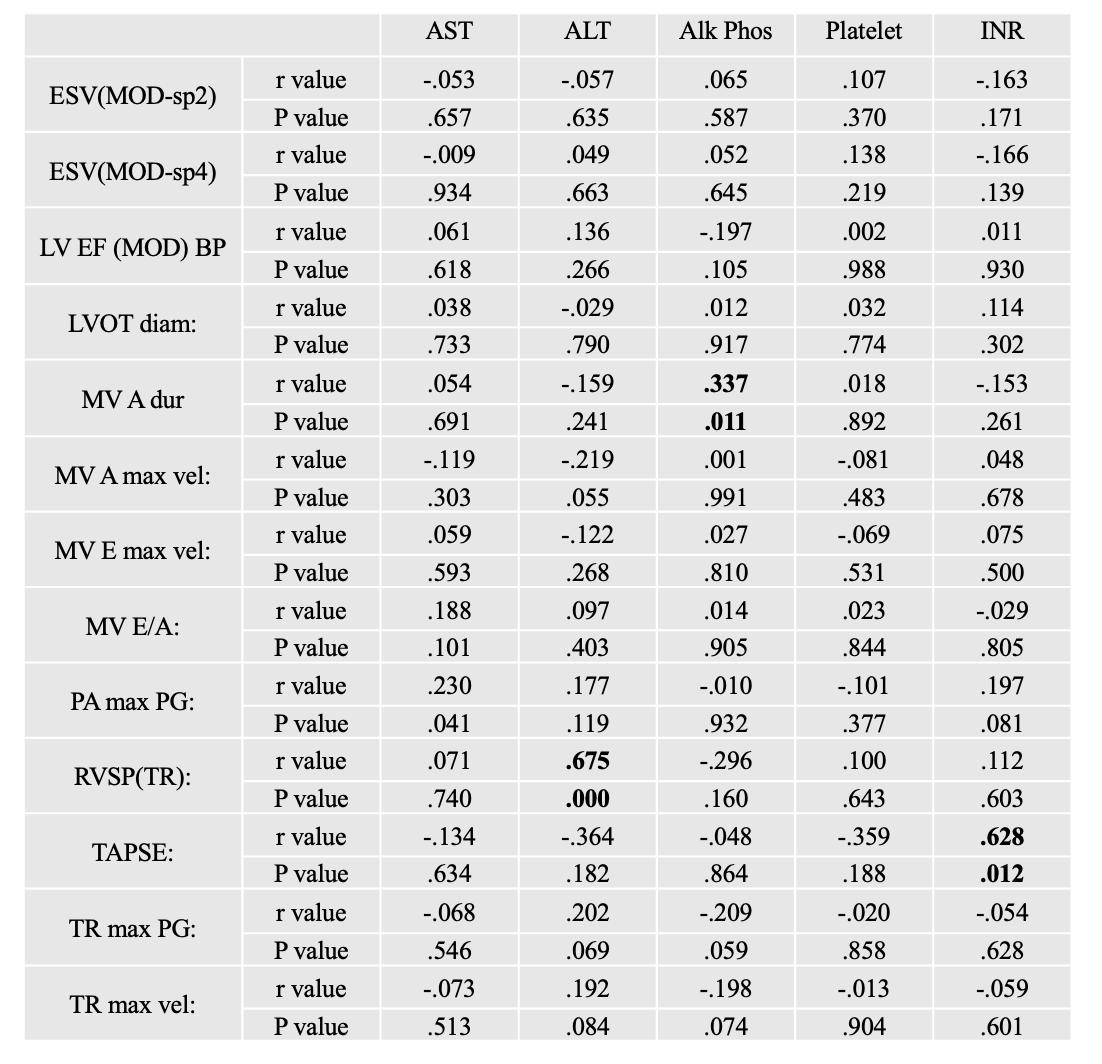
Figure: Table 2: Correlation of LFT parameters with ECHO parameters in study subjects
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Lakshmi Kattamuri indicated no relevant financial relationships.
Michael Brockman indicated no relevant financial relationships.
Mutaz Kalas indicated no relevant financial relationships.
Swati Mahapatra indicated no relevant financial relationships.
Keith Garrison indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Shivangini Duggal, MD1, Lakshmi Kattamuri, MD2, Michael J. Brockman, DO2, Mutaz Kalas, MD3, Swati Mahapatra, DO4, Keith Garrison, MD2, Sherif E. Elhanafi, MD2, Alejandro Robles, MD5. P5787 - Exploring the Relationship Between Cirrhotic Cardiomyopathy Development and Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 4Texas A&M, El Paso, TX; 5Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX
Introduction: Cirrhotic cardiomyopathy (CCM) is a subclinical cardiac dysfunction increasingly recognized in cirrhotic patients. Characterized by impaired systolic reserve, diastolic dysfunction, and electrophysiological abnormalities, CCM may contribute to the development of portal hypertension and its complications. This study evaluates the relationship between transthoracic echocardiographic (TTE) findings and portal hypertensive manifestations observed on esophagogastroduodenoscopy (EGD).
Methods: We retrospectively analyzed 94 patients with CCM at University Medical Center in El Paso (2014–2024) who underwent both TTE and EGD. Key demographic, echocardiographic, endoscopic, and liver disease severity data (FIB-4, MELD) were extracted.
Results: Among 94 patients (mean age 53.9±16.4 years; 57.4% female; 98.9% Hispanic), the leading etiologies were alcoholic liver disease (34%), hepatitis C (23.4%), NASH (17%), and autoimmune hepatitis (20.2%) (Table 1). EGD revealed esophageal varices in 70% (primarily Grade I–II) and portal gastropathy in 17%. Ascites (84%) and hepatic encephalopathy (61.7%) were common. TTE showed mean LVEF 49.7±20.8%, RVSP 33.6±12 mmHg, and TAPSE 1.77±0.75 cm. ALT correlated strongly with RVSP (r=0.675, p< 0.001), while AST correlated with PA max PG (r=0.230, p=0.041) (Table 2). MELD, Child-Pugh, and FIB-4 showed limited correlation with echocardiographic measures, suggesting subclinical cardiac dysfunction may precede hepatic decompensation.
Discussion: Echocardiographic features of CCM correlate with portal hypertension severity. Routine cardiac assessment may improve risk stratification and guide earlier interventions in cirrhosis. Incorporating echocardiographic evaluation into standard cirrhosis care may help identify high-risk patients before overt cardiac symptoms develop.
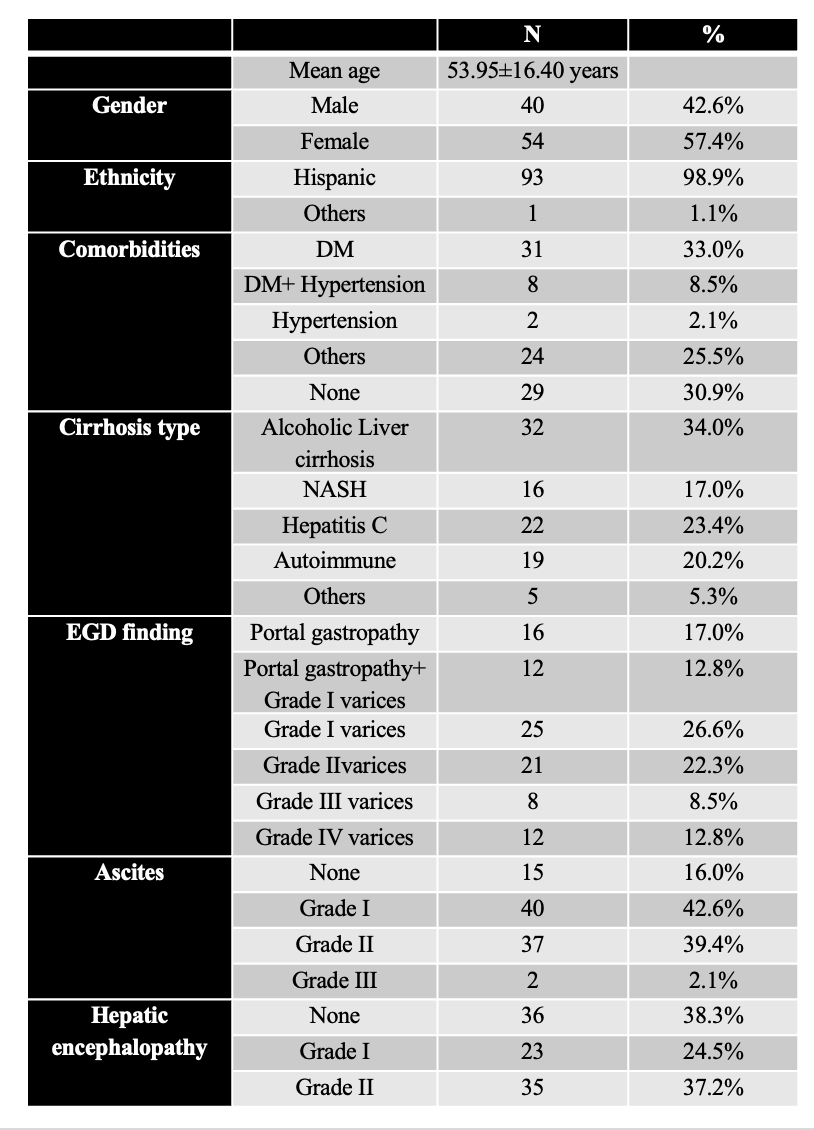
Figure: Table 1: Baseline characteristics in study subjects (n=94)
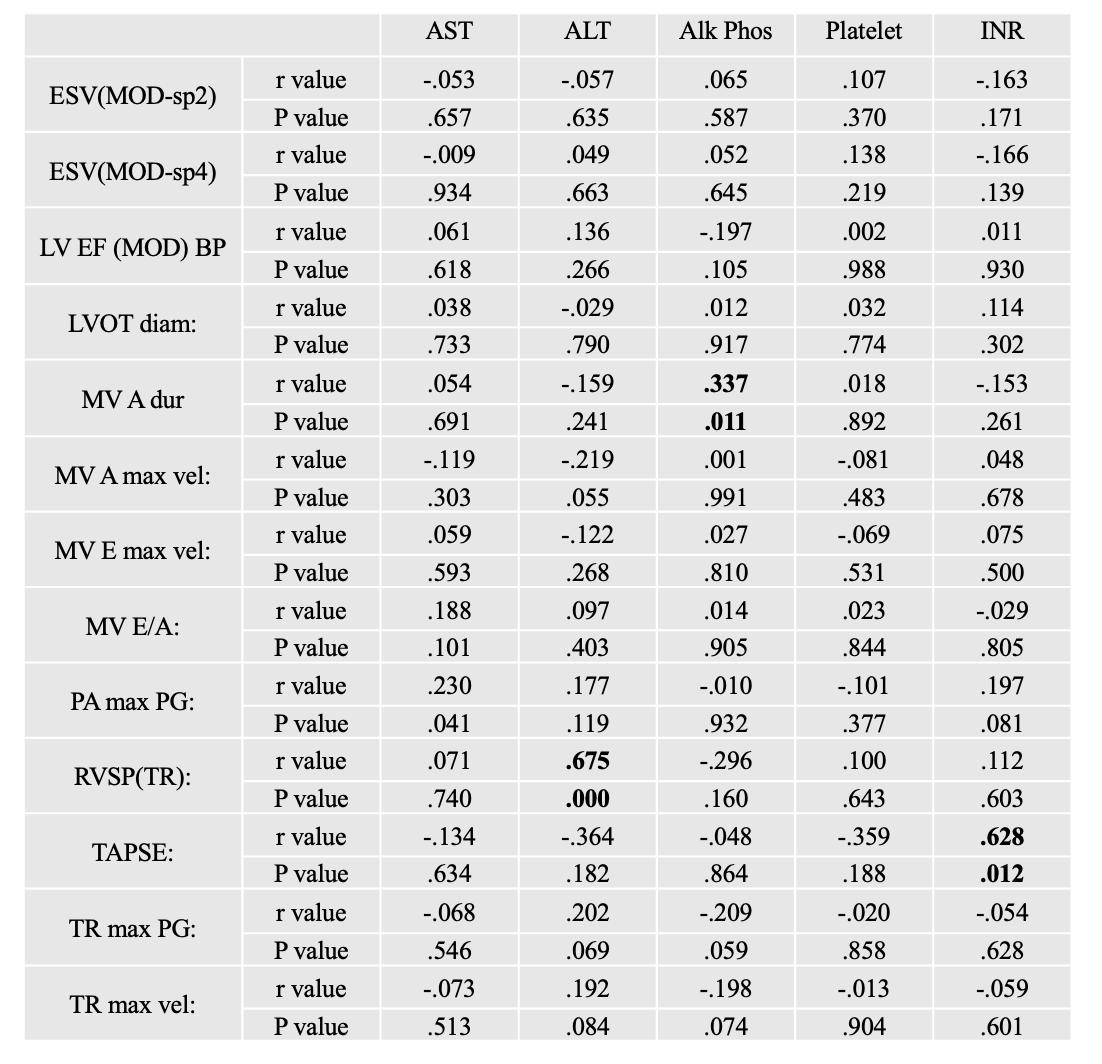
Figure: Table 2: Correlation of LFT parameters with ECHO parameters in study subjects
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Lakshmi Kattamuri indicated no relevant financial relationships.
Michael Brockman indicated no relevant financial relationships.
Mutaz Kalas indicated no relevant financial relationships.
Swati Mahapatra indicated no relevant financial relationships.
Keith Garrison indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Shivangini Duggal, MD1, Lakshmi Kattamuri, MD2, Michael J. Brockman, DO2, Mutaz Kalas, MD3, Swati Mahapatra, DO4, Keith Garrison, MD2, Sherif E. Elhanafi, MD2, Alejandro Robles, MD5. P5787 - Exploring the Relationship Between Cirrhotic Cardiomyopathy Development and Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
