Tuesday Poster Session
Category: Liver
P5777 - Long-Term Survivorship After Liver Transplantation - A Study of the US National Cohort
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ragesh Thandassery, MD
Central Arkansas Veterans Healthcare System, University of Arkansas for Medical Sciences
Little Rock, AR
Presenting Author(s)
Award: ACG Presidential Poster Award
Ragesh Thandassery, MD1, Allison Wells, MS, BS2, Suria Devarapalli, DO3, Thomas Schiano, MD4, Tamar Taddei, MD5
1Dept of Solid Organ Transplantation, University of Arkansas for Medical Sciences, Little Rock, AR; 2Biostatistician, Dept of Solid Organ Transplantation, University of Arkansas for Medical Sciences, Little Rock, AR; 3University of Arkansas for Medical Sciences, Little Rock, AR; 4Dept of Abdominal Transplantation Recanati/Miller Transplantation Institute/Division of Liver Diseases, Mt Sinai Hospital, NY, New York, NY; 5Dept of Gastroenterology and Hepatology, Yale School of Medicine & VA Connecticut Healthcare System, West Haven, CT
Introduction: We aimed to characterize the mortality trends in patients who survived liver transplantation (LT) for > 5 years in the US. Long-term outcomes are mostly unknown, as transplant centers are attuned to 1, 3, and 5-year post-LT outcomes.
Methods: We analyzed adult patients who underwent LT between Feb 2002 and Sept 2018 (UNOS cohort) and followed them until Sept 2024. Among 101,017 patients who underwent LT, after excluding retransplants and lost to follow-up, 87,693 were included. Causes of death (COD) and death rates (DR) were calculated in 5-year intervals after 5 years post-LT. Trends were compared across two different time intervals: Group T1 (2002-2010) and Group T2 (2011-2018).
Results: Median age at LT was 56 (IQR 30-62), 66.4% were male, 72.1% were Caucasian. Analyzing COD; malignancy (6.9%), cardiovascular (CV) events (5.3%), infection (3.9%), and graft failure [GF] (3.8%) were the leading causes. With every successive 5 y post-LT, there is a shift in the predominant COD (Fig-1). In 5–10 y post-LT, DR from malignancy was 27.9%, CV 16.4%, GF 8.8%, and infection 8.2%; but at 20–25-y, respective values were 17.8%, 21.6%, 3.8%, and 10.2%. At 20–25 years, CV was the most common COD, followed by malignancy, respiratory failure (RF), and infection. CV and infection showed a steady increase, whereas malignancy and GF showed a steady decrease over time. A similar trend was noted in gender specific DR analysis also (Fig-2), and as expected, COD from CV was lower in women.
Analyzing trends in Groups T1 and T2, at 5–10-y malignancy and CV were the most common COD in both groups, but infections, GF and renal failure were lower in Group T2 (T1- 9.4%, 11.7% and 5.3%, T2- 6.6%, 5.4% and 3.2%). At 10–15 y, a marked increase in RF as COD was noted in T2 (15.4% vs 10.0% in T1). COVID-19 pandemic likely accounts for the surge in RF as COD at these time intervals.
The following were independently associated with long-term death in a Cox-PH model (HR, CI)- age at LT (1.03, 1.03-1.03), pre-LT malignancy (1.08, 1.03-1.14), pre-LT diabetes (1.42, 1.36-1.47), poor performance status (1.22, 1.16-1.28), LT in Group T2 (0.86, 0.83-0.90), p< 0.001 (MELD at LT was not associated).
Discussion: COD post-LT has shown a shift with every successive 5 years; malignancy is the predominant cause in 5-10 years and CV in 20-25 years, in both genders. LT between 2010 and 2018 showed increased long-term survival compared to the previous decade, indicating refinement in LT care over time.
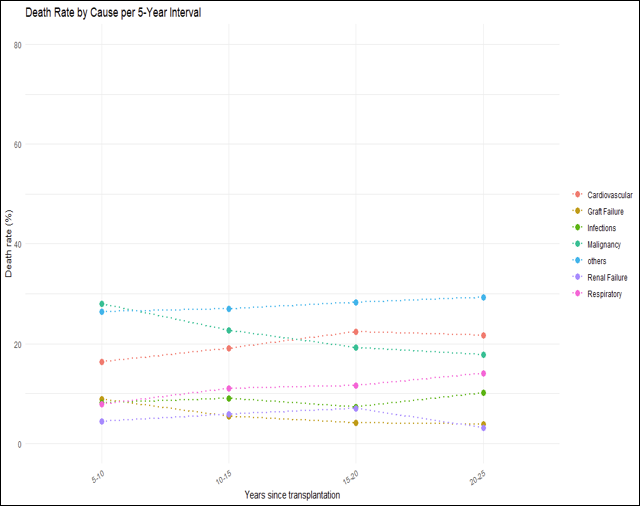
Figure: Title: Long-term (>5 years) mortality trend in LT recipients
Legend: The spike in respiratory failure as COD in 20-25 years in overall and 10–15-year interval in T2 group likely corresponds to the COVID-19 pandemic
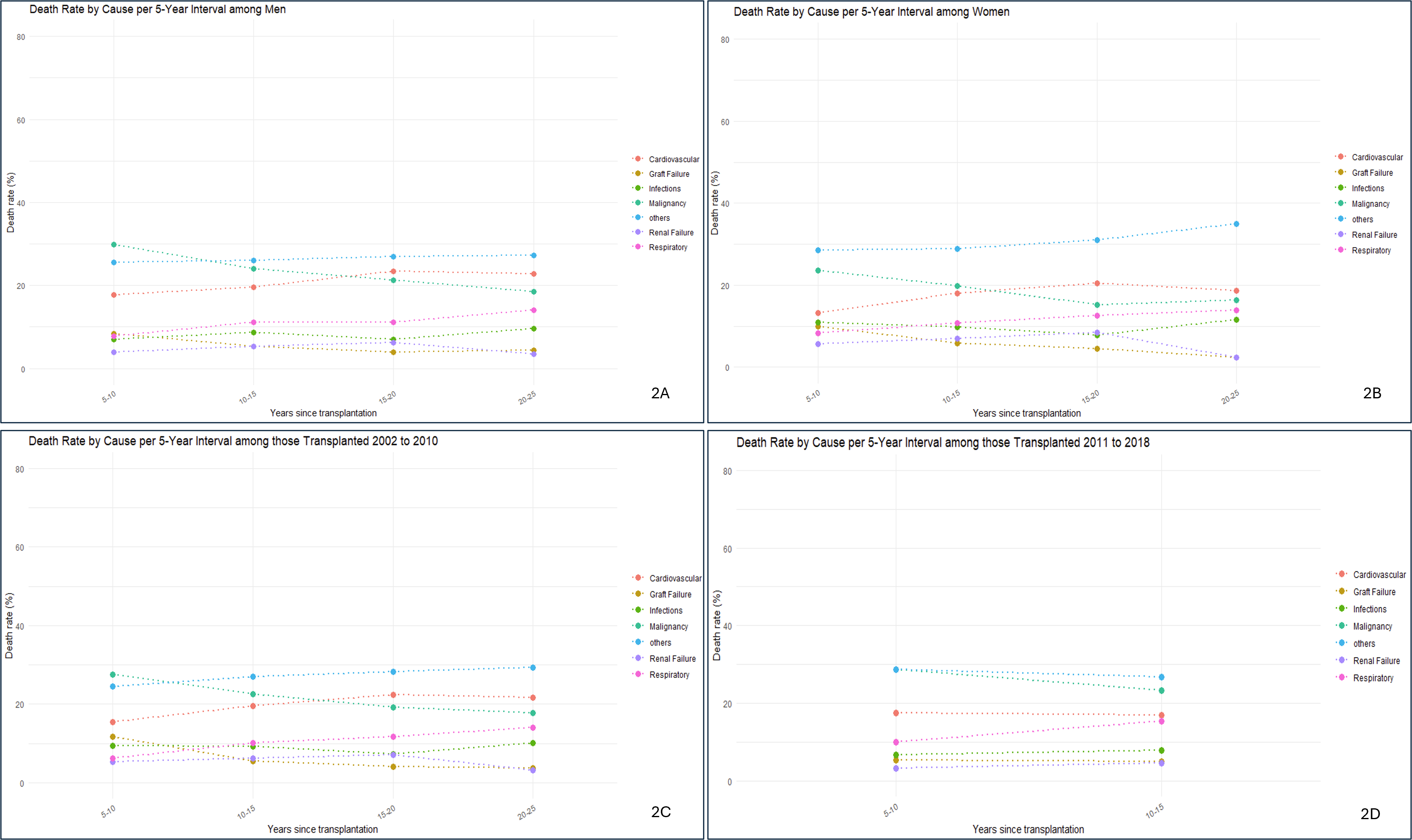
Figure: Title: Long-term (>5years) mortality trend in LT recipients, gender, and time interval characteristics
Disclosures:
Ragesh Thandassery indicated no relevant financial relationships.
Allison Wells indicated no relevant financial relationships.
Suria Devarapalli indicated no relevant financial relationships.
Thomas Schiano indicated no relevant financial relationships.
Tamar Taddei indicated no relevant financial relationships.
Ragesh Thandassery, MD1, Allison Wells, MS, BS2, Suria Devarapalli, DO3, Thomas Schiano, MD4, Tamar Taddei, MD5. P5777 - Long-Term Survivorship After Liver Transplantation - A Study of the US National Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Ragesh Thandassery, MD1, Allison Wells, MS, BS2, Suria Devarapalli, DO3, Thomas Schiano, MD4, Tamar Taddei, MD5
1Dept of Solid Organ Transplantation, University of Arkansas for Medical Sciences, Little Rock, AR; 2Biostatistician, Dept of Solid Organ Transplantation, University of Arkansas for Medical Sciences, Little Rock, AR; 3University of Arkansas for Medical Sciences, Little Rock, AR; 4Dept of Abdominal Transplantation Recanati/Miller Transplantation Institute/Division of Liver Diseases, Mt Sinai Hospital, NY, New York, NY; 5Dept of Gastroenterology and Hepatology, Yale School of Medicine & VA Connecticut Healthcare System, West Haven, CT
Introduction: We aimed to characterize the mortality trends in patients who survived liver transplantation (LT) for > 5 years in the US. Long-term outcomes are mostly unknown, as transplant centers are attuned to 1, 3, and 5-year post-LT outcomes.
Methods: We analyzed adult patients who underwent LT between Feb 2002 and Sept 2018 (UNOS cohort) and followed them until Sept 2024. Among 101,017 patients who underwent LT, after excluding retransplants and lost to follow-up, 87,693 were included. Causes of death (COD) and death rates (DR) were calculated in 5-year intervals after 5 years post-LT. Trends were compared across two different time intervals: Group T1 (2002-2010) and Group T2 (2011-2018).
Results: Median age at LT was 56 (IQR 30-62), 66.4% were male, 72.1% were Caucasian. Analyzing COD; malignancy (6.9%), cardiovascular (CV) events (5.3%), infection (3.9%), and graft failure [GF] (3.8%) were the leading causes. With every successive 5 y post-LT, there is a shift in the predominant COD (Fig-1). In 5–10 y post-LT, DR from malignancy was 27.9%, CV 16.4%, GF 8.8%, and infection 8.2%; but at 20–25-y, respective values were 17.8%, 21.6%, 3.8%, and 10.2%. At 20–25 years, CV was the most common COD, followed by malignancy, respiratory failure (RF), and infection. CV and infection showed a steady increase, whereas malignancy and GF showed a steady decrease over time. A similar trend was noted in gender specific DR analysis also (Fig-2), and as expected, COD from CV was lower in women.
Analyzing trends in Groups T1 and T2, at 5–10-y malignancy and CV were the most common COD in both groups, but infections, GF and renal failure were lower in Group T2 (T1- 9.4%, 11.7% and 5.3%, T2- 6.6%, 5.4% and 3.2%). At 10–15 y, a marked increase in RF as COD was noted in T2 (15.4% vs 10.0% in T1). COVID-19 pandemic likely accounts for the surge in RF as COD at these time intervals.
The following were independently associated with long-term death in a Cox-PH model (HR, CI)- age at LT (1.03, 1.03-1.03), pre-LT malignancy (1.08, 1.03-1.14), pre-LT diabetes (1.42, 1.36-1.47), poor performance status (1.22, 1.16-1.28), LT in Group T2 (0.86, 0.83-0.90), p< 0.001 (MELD at LT was not associated).
Discussion: COD post-LT has shown a shift with every successive 5 years; malignancy is the predominant cause in 5-10 years and CV in 20-25 years, in both genders. LT between 2010 and 2018 showed increased long-term survival compared to the previous decade, indicating refinement in LT care over time.
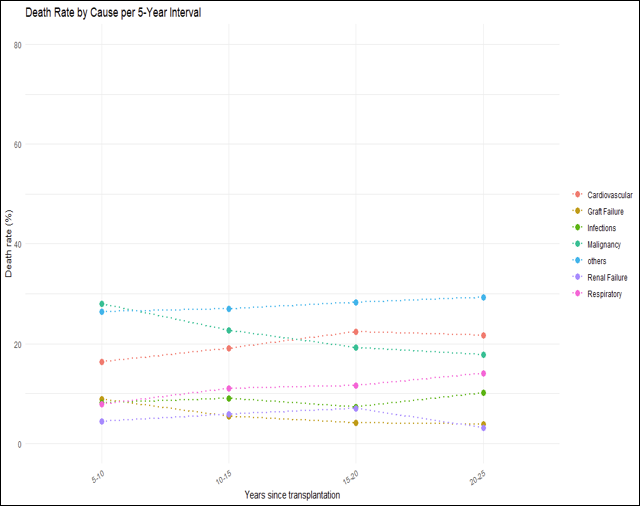
Figure: Title: Long-term (>5 years) mortality trend in LT recipients
Legend: The spike in respiratory failure as COD in 20-25 years in overall and 10–15-year interval in T2 group likely corresponds to the COVID-19 pandemic
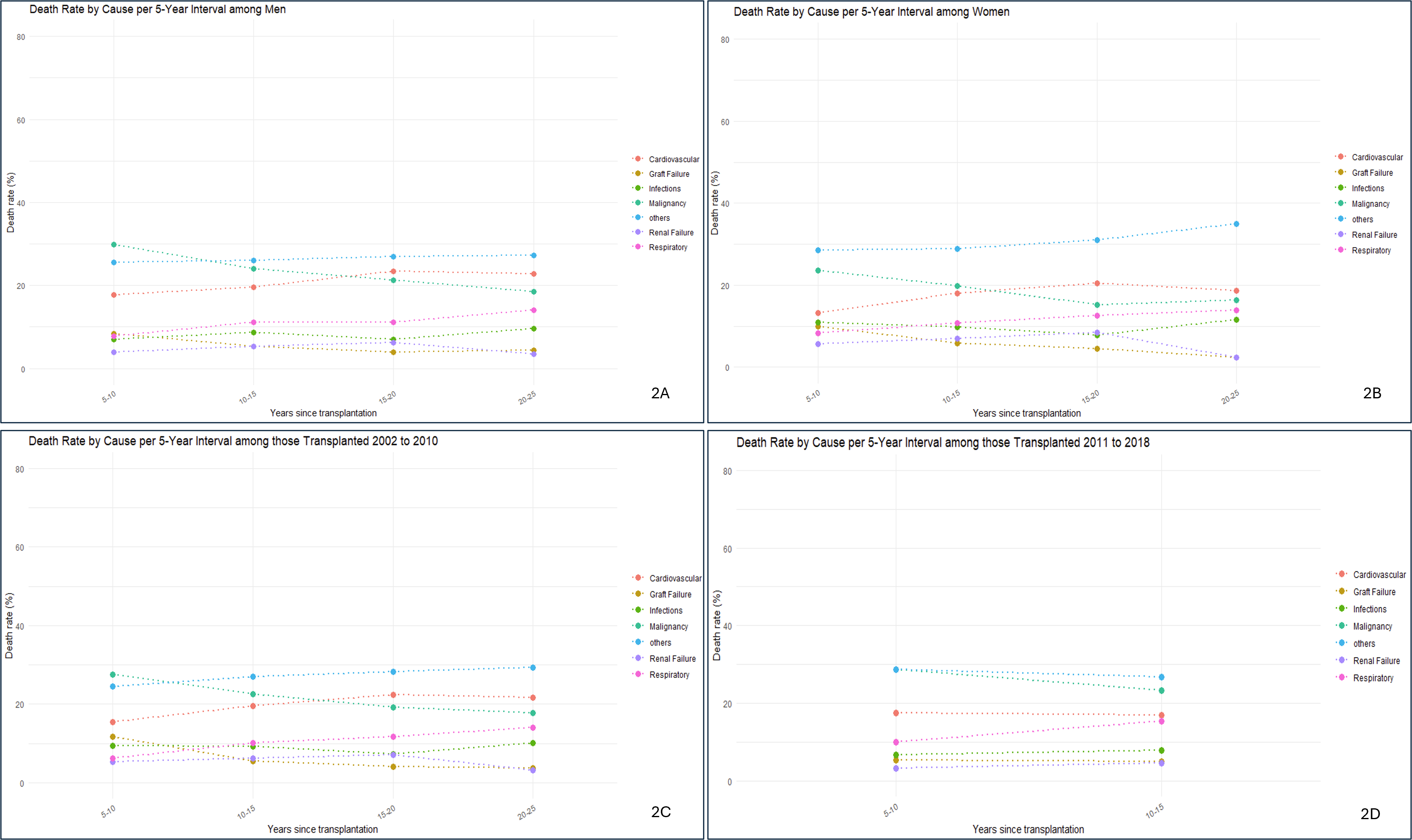
Figure: Title: Long-term (>5years) mortality trend in LT recipients, gender, and time interval characteristics
Disclosures:
Ragesh Thandassery indicated no relevant financial relationships.
Allison Wells indicated no relevant financial relationships.
Suria Devarapalli indicated no relevant financial relationships.
Thomas Schiano indicated no relevant financial relationships.
Tamar Taddei indicated no relevant financial relationships.
Ragesh Thandassery, MD1, Allison Wells, MS, BS2, Suria Devarapalli, DO3, Thomas Schiano, MD4, Tamar Taddei, MD5. P5777 - Long-Term Survivorship After Liver Transplantation - A Study of the US National Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

