Tuesday Poster Session
Category: Liver
P5776 - Correlation of Epicardial Fat Thickness With Vibration-Controlled Transient Elastography - Continued Attenuation Parameter in Veterans With MASLD
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aakash Rana, MD (he/him/his)
Central Arkansas Veterans Healthcare System
Little Rock, AR
Presenting Author(s)
Aakash Rana, MD1, Sai Nikhila Ghanta, MD2, Suria Devarapalli, DO2, Adalberto Guzman, MD3, Srikanth Vallurupalli, MD1, Ragesh Thandassery, MD1
1Central Arkansas Veterans Healthcare System, Little Rock, AR; 2University of Arkansas for Medical Sciences, Little Rock, AR; 3University of Arkansas, Little Rock, AR
Introduction: Epicardial fat thickness (EFT) is an important predictor of cardiometabolic risk in adults. Metabolic dysfunction associated steatotic liver disease (MASLD) is the most important cause of liver disease in the US, and cardiovascular disease is the most important cause of death in MASLD. Estimation of cardiometabolic risk in these patients is therefore crucial. We attempted to correlate the continued attenuation parameter (CAP) measured using vibration-controlled transient elastography (FibroScan®) with the EFT measured using transthoracic echocardiography (TTE) in patients with MASLD as the predominant etiology of liver disease.
Methods: We retrospectively analyzed veterans with MASLD who were evaluated in the liver clinic between January 2019 and December 2024 (single center in Mid-West US). Hepatic steatosis (HS) markers, hepatic steatotic index (HSI), and CAP on FirboScan were compared with the EFT measured on TTE. HSI is calculated as 8×(ALT / AST) + BMI + 2 (if type 2 diabetes) + 2 (if female).
Only TTE performed within 6 months of FibroScan measurement were included. FibroScan reads with IQR ≥15 were excluded. Liver stiffness measurement (LSM) of ≥ 20kPa was defined as compensated advanced chronic liver disease (cACLD), and CAP≥ 275db/m as hepatic steatosis.
Results: Among 1298 patients, 244 patients met the inclusion criteria. The mean (SD) age was 64.1 (±9.8) years (92.2% males; 72.5% Caucasians). The median BMI (IQR) was 30.3 (25.9-35), and 51.2% were obese. Median values for serum albumin, fibrosis-4 (FIB-4 score), and NAFLD fibrosis score (NFS) were 3.7 (3.4-4.0) g/dl, 1.8 (1.3-2.8), and 0.129 (-1.1-1.2) respectively. Median value for HSI was 38.1 (32.7-44.2). FibroScan values revealed a median LSM of 8.7 (5.8-16.9) and a median CAP of 287 (233-331). cACLD was present in 21.7%.
Median EFT was 4.5 (2.4-7.5 mm), and 57.4% had EFT more than 5mm. On bivariate Spearman correlation, the HSI did not show a correlation with EFT (p=0.08). However, the CAP measurement revealed a significant correlation with EFT (r = 0.52, p = 0.039), Figure 1.
Discussion: In this cohort of veterans with MASLD, we observed a good correlation between CAP measured on FibroScan and EFT measured on TTE, indicating that elevated FirboScan CAP can also suggest an increased cardiometabolic risk. The potential for FibroScan CAP as a surrogate marker for cardiometabolic risk in patients with MASLD is promising, but these findings need to be validated by larger multicentric studies.
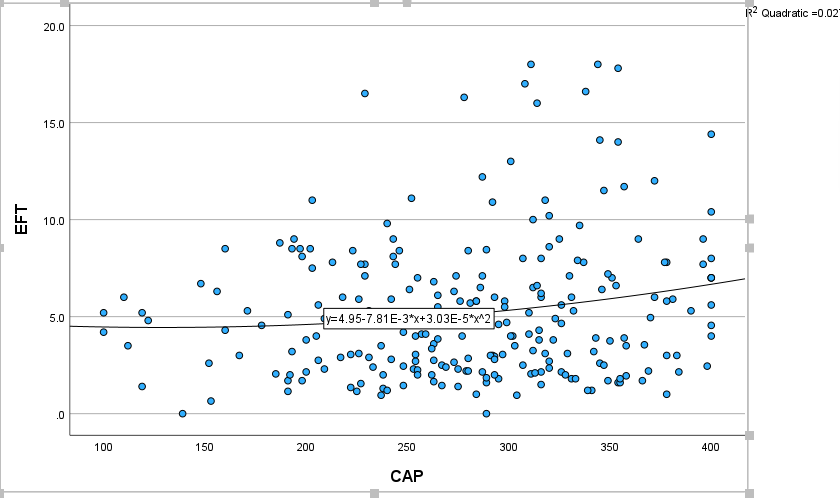
Figure: Correlation between Continued Attenuation Parameter (CAP) on FirboScan and Epicardial fat thickness (EFT) on transthoracic echocardiography (TTE)
Disclosures:
Aakash Rana indicated no relevant financial relationships.
Sai Nikhila Ghanta indicated no relevant financial relationships.
Suria Devarapalli indicated no relevant financial relationships.
Adalberto Guzman indicated no relevant financial relationships.
Srikanth Vallurupalli indicated no relevant financial relationships.
Ragesh Thandassery indicated no relevant financial relationships.
Aakash Rana, MD1, Sai Nikhila Ghanta, MD2, Suria Devarapalli, DO2, Adalberto Guzman, MD3, Srikanth Vallurupalli, MD1, Ragesh Thandassery, MD1. P5776 - Correlation of Epicardial Fat Thickness With Vibration-Controlled Transient Elastography - Continued Attenuation Parameter in Veterans With MASLD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Central Arkansas Veterans Healthcare System, Little Rock, AR; 2University of Arkansas for Medical Sciences, Little Rock, AR; 3University of Arkansas, Little Rock, AR
Introduction: Epicardial fat thickness (EFT) is an important predictor of cardiometabolic risk in adults. Metabolic dysfunction associated steatotic liver disease (MASLD) is the most important cause of liver disease in the US, and cardiovascular disease is the most important cause of death in MASLD. Estimation of cardiometabolic risk in these patients is therefore crucial. We attempted to correlate the continued attenuation parameter (CAP) measured using vibration-controlled transient elastography (FibroScan®) with the EFT measured using transthoracic echocardiography (TTE) in patients with MASLD as the predominant etiology of liver disease.
Methods: We retrospectively analyzed veterans with MASLD who were evaluated in the liver clinic between January 2019 and December 2024 (single center in Mid-West US). Hepatic steatosis (HS) markers, hepatic steatotic index (HSI), and CAP on FirboScan were compared with the EFT measured on TTE. HSI is calculated as 8×(ALT / AST) + BMI + 2 (if type 2 diabetes) + 2 (if female).
Only TTE performed within 6 months of FibroScan measurement were included. FibroScan reads with IQR ≥15 were excluded. Liver stiffness measurement (LSM) of ≥ 20kPa was defined as compensated advanced chronic liver disease (cACLD), and CAP≥ 275db/m as hepatic steatosis.
Results: Among 1298 patients, 244 patients met the inclusion criteria. The mean (SD) age was 64.1 (±9.8) years (92.2% males; 72.5% Caucasians). The median BMI (IQR) was 30.3 (25.9-35), and 51.2% were obese. Median values for serum albumin, fibrosis-4 (FIB-4 score), and NAFLD fibrosis score (NFS) were 3.7 (3.4-4.0) g/dl, 1.8 (1.3-2.8), and 0.129 (-1.1-1.2) respectively. Median value for HSI was 38.1 (32.7-44.2). FibroScan values revealed a median LSM of 8.7 (5.8-16.9) and a median CAP of 287 (233-331). cACLD was present in 21.7%.
Median EFT was 4.5 (2.4-7.5 mm), and 57.4% had EFT more than 5mm. On bivariate Spearman correlation, the HSI did not show a correlation with EFT (p=0.08). However, the CAP measurement revealed a significant correlation with EFT (r = 0.52, p = 0.039), Figure 1.
Discussion: In this cohort of veterans with MASLD, we observed a good correlation between CAP measured on FibroScan and EFT measured on TTE, indicating that elevated FirboScan CAP can also suggest an increased cardiometabolic risk. The potential for FibroScan CAP as a surrogate marker for cardiometabolic risk in patients with MASLD is promising, but these findings need to be validated by larger multicentric studies.
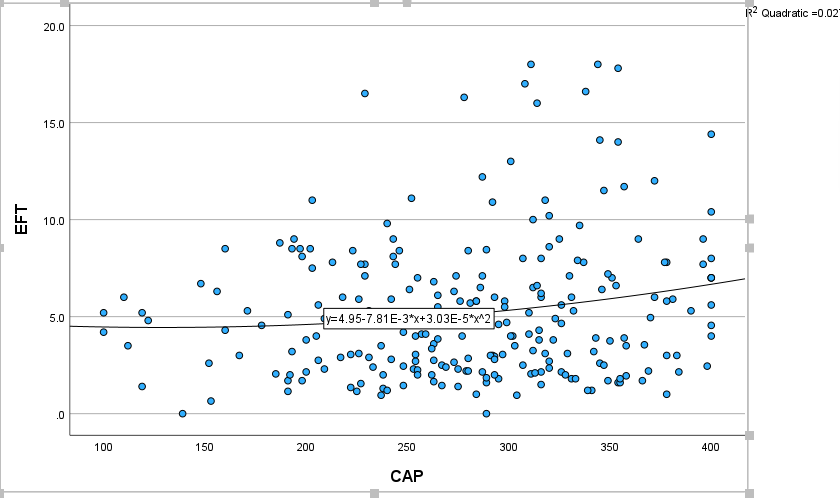
Figure: Correlation between Continued Attenuation Parameter (CAP) on FirboScan and Epicardial fat thickness (EFT) on transthoracic echocardiography (TTE)
Disclosures:
Aakash Rana indicated no relevant financial relationships.
Sai Nikhila Ghanta indicated no relevant financial relationships.
Suria Devarapalli indicated no relevant financial relationships.
Adalberto Guzman indicated no relevant financial relationships.
Srikanth Vallurupalli indicated no relevant financial relationships.
Ragesh Thandassery indicated no relevant financial relationships.
Aakash Rana, MD1, Sai Nikhila Ghanta, MD2, Suria Devarapalli, DO2, Adalberto Guzman, MD3, Srikanth Vallurupalli, MD1, Ragesh Thandassery, MD1. P5776 - Correlation of Epicardial Fat Thickness With Vibration-Controlled Transient Elastography - Continued Attenuation Parameter in Veterans With MASLD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
