Tuesday Poster Session
Category: Liver
P5763 - Insurance Status and Outcomes Following Liver Injury From Motor Vehicle Accidents: An Analysis of the National Trauma Data Bank (2017-2022)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AJ
Annie Jia, BS
University of Arizona College of Medicine - Phoenix
Phoenix, AZ
Presenting Author(s)
Annie Jia, BS1, Sophie Nguyen, BS2, Kinsley Wang, BS1, Angeli Sirilan, BS, BA1
1University of Arizona College of Medicine - Phoenix, Phoenix, AZ; 2University of Arizona College of Medicine, Phoenix, Phoenix, AZ
Introduction: Motor vehicle accidents (MVA) are a leading cause of injury and death among adults, frequently causing liver injury and an average of 37,000 deaths per year in the United States. Insurance status has been studied to improve long-term outcomes post-trauma, but there are few studies investigating its impact for patients with liver trauma post-MVA. This study presents mortality outcomes of liver trauma after MVA using the National Trauma Data Bank (NTDB).
Methods: Adult patients with liver trauma from a motor vehicle accident (MVA) were identified in the 2017–2022 NTDB using ICD-10 codes. Patients were grouped by insurance status including self-pay, public insurance (Medicaid, Medicare, other government), private insurance, and others. Associations between insurance status and mortality adjusting for sex, race, ethnicity, comorbidities, and injury severity scores (ISS) were evaluated with multivariable logistic regression analysis.
Results: Among the 73,900 identified patients, 12,253 (16.5%) were self-pay, 21,549 (29.2%) had public insurance, 34,924 (47.3%) had private insurance, and 5,174 (7%) had other forms of insurance. Self-paying patients were more likely to be younger, male, black, and be intoxicated by alcohol compared to other forms of insurance (all P < 0.001). Despite having greater ISS scores, self-paying patients had shorter hospital and ICU lengths of stay (all P < 0.001). After adjusting for confounding variables, patients with public insurance (OR = 0.50, 95% CI = 0.46-0.56, P < 0.001), private insurance (OR = 0.44, 95% CI = 0.40-0.49, P < 0.001), or other forms of insurance (OR = 0.55, 95% CI = 0.47-0.65, P < 0.001) had about 2 times lower odds of mortality compared to self-paying patients.
Discussion: Despite having greater ISS scores for liver trauma after a MVA, self-paying patients spent less time in the hospital and ICU. Insurance status was significantly associated with in-hospital mortality, with being insured decreasing their odds by 2-fold. These findings underscore the critical role insurance status has on healthcare resources and survivability after MVA. Strategies should be developed to promote equitable resource allocation and interventions to ensure that insurance status does not impact health outcomes.
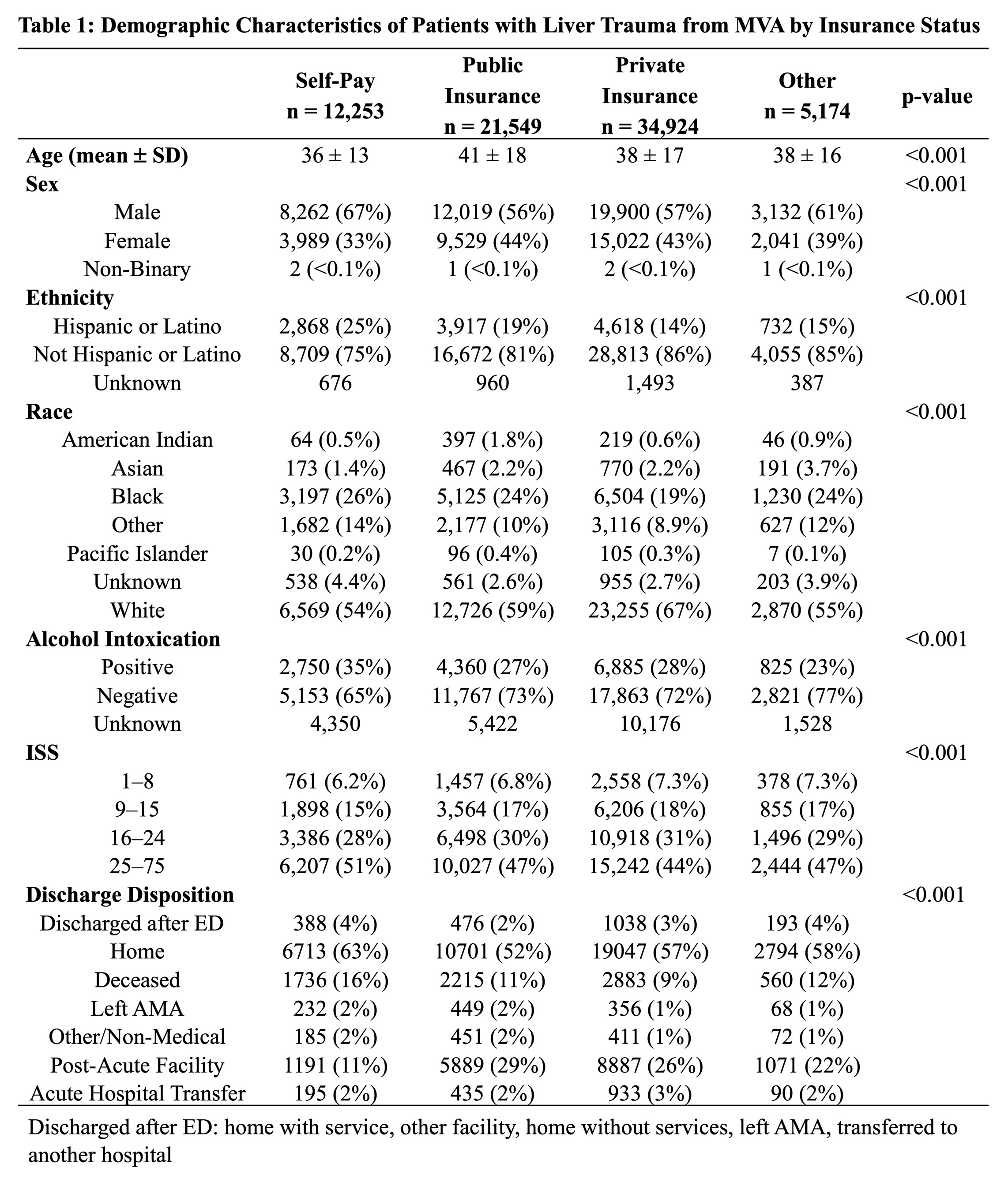
Figure: Table 1: Demographic Characteristics of Patients with Liver Trauma from MVA by Insurance Status
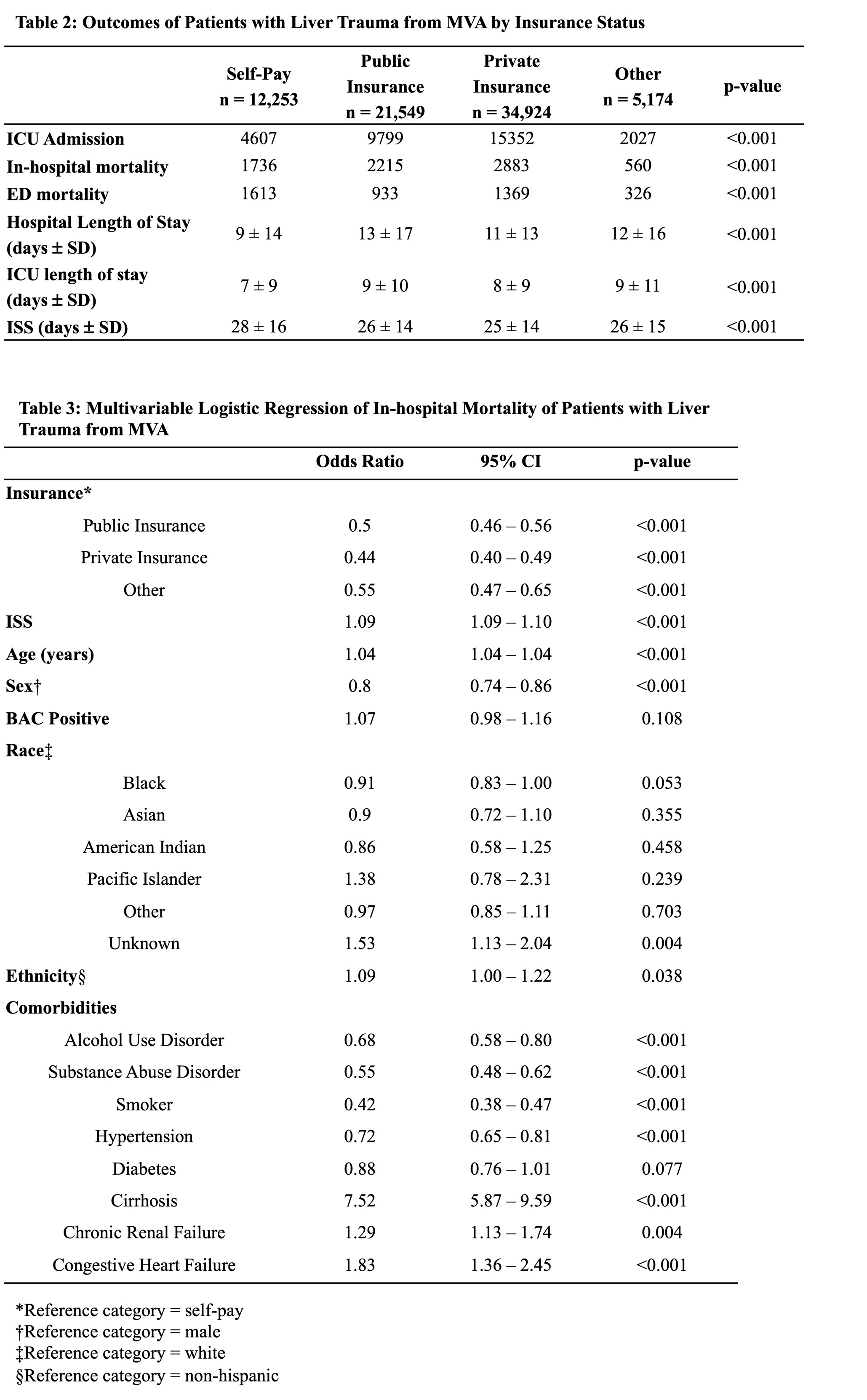
Figure: Table 2: Outcomes of Patients with Liver Trauma from MVA by Insurance Status, Table 3: Multivariable Logistic Regression of In-hospital Mortality of Patients with Liver Trauma from MVA
Disclosures:
Annie Jia indicated no relevant financial relationships.
Sophie Nguyen indicated no relevant financial relationships.
Kinsley Wang indicated no relevant financial relationships.
Angeli Sirilan indicated no relevant financial relationships.
Annie Jia, BS1, Sophie Nguyen, BS2, Kinsley Wang, BS1, Angeli Sirilan, BS, BA1. P5763 - Insurance Status and Outcomes Following Liver Injury From Motor Vehicle Accidents: An Analysis of the National Trauma Data Bank (2017-2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Arizona College of Medicine - Phoenix, Phoenix, AZ; 2University of Arizona College of Medicine, Phoenix, Phoenix, AZ
Introduction: Motor vehicle accidents (MVA) are a leading cause of injury and death among adults, frequently causing liver injury and an average of 37,000 deaths per year in the United States. Insurance status has been studied to improve long-term outcomes post-trauma, but there are few studies investigating its impact for patients with liver trauma post-MVA. This study presents mortality outcomes of liver trauma after MVA using the National Trauma Data Bank (NTDB).
Methods: Adult patients with liver trauma from a motor vehicle accident (MVA) were identified in the 2017–2022 NTDB using ICD-10 codes. Patients were grouped by insurance status including self-pay, public insurance (Medicaid, Medicare, other government), private insurance, and others. Associations between insurance status and mortality adjusting for sex, race, ethnicity, comorbidities, and injury severity scores (ISS) were evaluated with multivariable logistic regression analysis.
Results: Among the 73,900 identified patients, 12,253 (16.5%) were self-pay, 21,549 (29.2%) had public insurance, 34,924 (47.3%) had private insurance, and 5,174 (7%) had other forms of insurance. Self-paying patients were more likely to be younger, male, black, and be intoxicated by alcohol compared to other forms of insurance (all P < 0.001). Despite having greater ISS scores, self-paying patients had shorter hospital and ICU lengths of stay (all P < 0.001). After adjusting for confounding variables, patients with public insurance (OR = 0.50, 95% CI = 0.46-0.56, P < 0.001), private insurance (OR = 0.44, 95% CI = 0.40-0.49, P < 0.001), or other forms of insurance (OR = 0.55, 95% CI = 0.47-0.65, P < 0.001) had about 2 times lower odds of mortality compared to self-paying patients.
Discussion: Despite having greater ISS scores for liver trauma after a MVA, self-paying patients spent less time in the hospital and ICU. Insurance status was significantly associated with in-hospital mortality, with being insured decreasing their odds by 2-fold. These findings underscore the critical role insurance status has on healthcare resources and survivability after MVA. Strategies should be developed to promote equitable resource allocation and interventions to ensure that insurance status does not impact health outcomes.
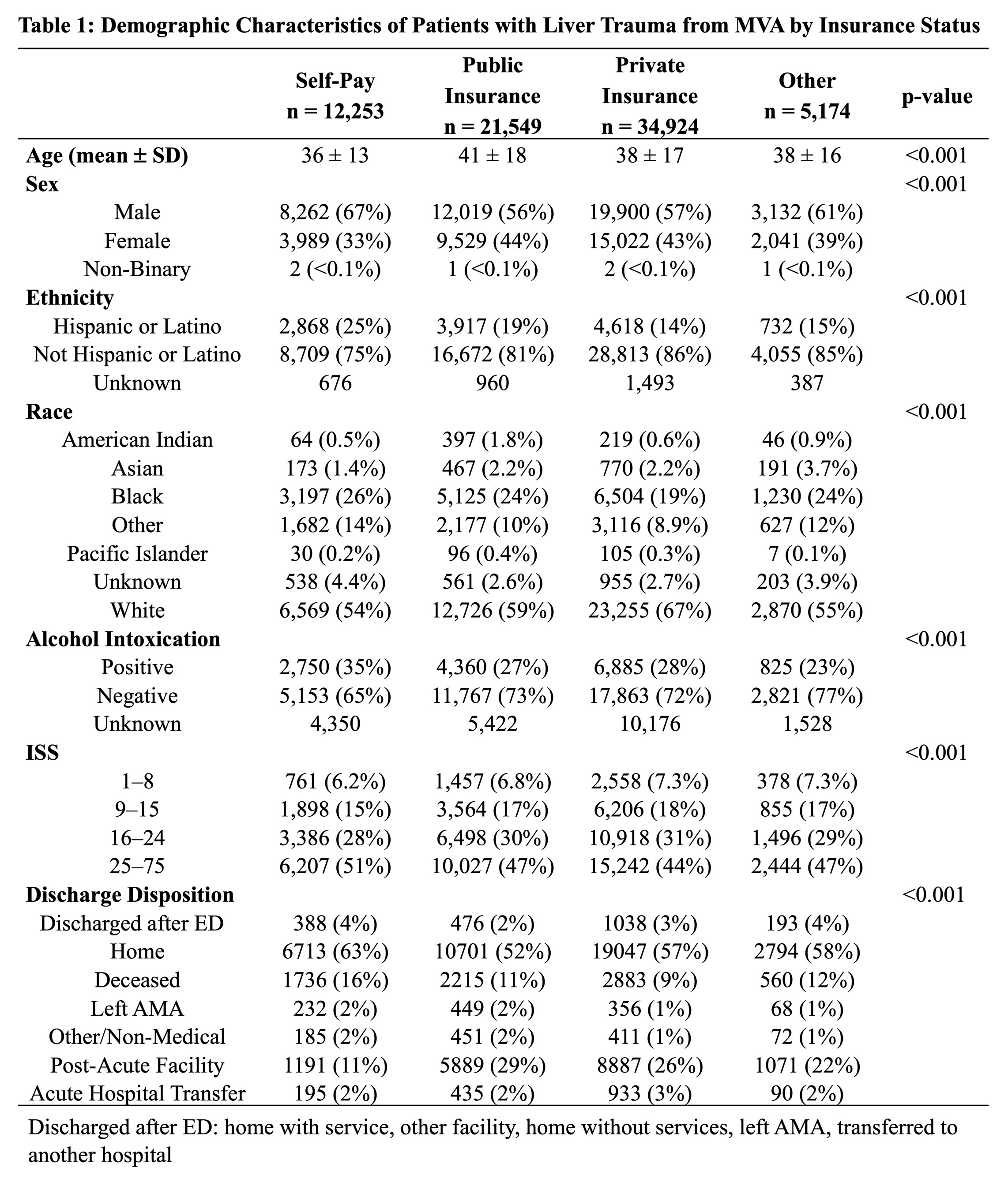
Figure: Table 1: Demographic Characteristics of Patients with Liver Trauma from MVA by Insurance Status
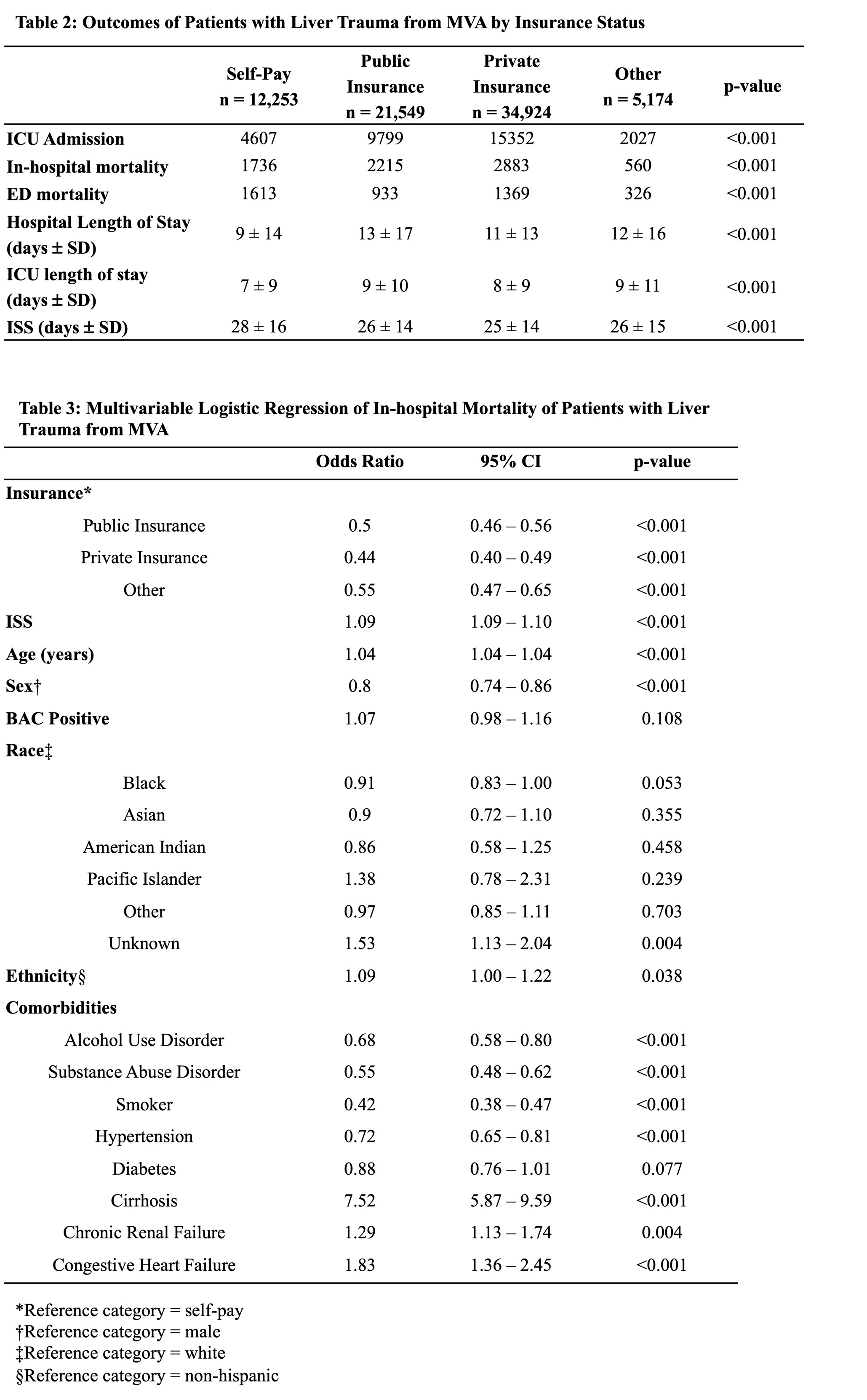
Figure: Table 2: Outcomes of Patients with Liver Trauma from MVA by Insurance Status, Table 3: Multivariable Logistic Regression of In-hospital Mortality of Patients with Liver Trauma from MVA
Disclosures:
Annie Jia indicated no relevant financial relationships.
Sophie Nguyen indicated no relevant financial relationships.
Kinsley Wang indicated no relevant financial relationships.
Angeli Sirilan indicated no relevant financial relationships.
Annie Jia, BS1, Sophie Nguyen, BS2, Kinsley Wang, BS1, Angeli Sirilan, BS, BA1. P5763 - Insurance Status and Outcomes Following Liver Injury From Motor Vehicle Accidents: An Analysis of the National Trauma Data Bank (2017-2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

