Tuesday Poster Session
Category: Interventional Endoscopy
P5755 - No Light at the End of the Tunnel: Closing a Mucosal Defect from Inside the Tunnel During G-POEM Procedure
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FH
Falak Hamo, MD
University of Kansas Medical Center
Overland Park, KS
Presenting Author(s)
Falak Hamo, MD1, Shahryar Khan, MD2, Mashal Alam Khan, MBBS3, Mollie Jackson, DO2, Kevin Liu, MD4, Salih Samo, MD, MSci1
1University of Kansas Medical Center, Overland Park, KS; 2University of Kansas Medical Center, Kansas City, KS; 3Khyber Medical University, Kansas City, KS; 4Banner University Medical Center, Phoenix, AZ
Introduction: Mucosal injuries during peroral endoscopic myotomy (POEM) can lead to leaks and infection. Therefore, recognizing such injuries and closing them is important to avoid adverse outcomes requiring surgery. We report a case of gastric POEM (GPOEM) with a mucosal defect closure from inside the tunnel due to difficult luminal side closure.
Case Description/
Methods: A 48-year-old female with gastroparesis (gastric emptying study with 68% retention at 4 hours) with abdominal pain after eating, epigastric fullness, early satiety, bloating, nausea with rare vomiting, not feeling hungry, and 60 lbs weight loss over two years underwent GPOEM due to concern about long term neurological side effects with metoclopramide in the setting of lamotrigine use for bipolar disorder. Her gastroparesis cardinal symptom index (GCS I) was 3.75.
During the GPOEM procedure a significant bleeding occurred during submucosal tunneling requiring cautery use, which led to a thermal mucosal injury in the duodenal bulb just distal to the pylorus (Figure 1, panel A. Panel B represents a view of the mucosal defect from inside the tunnel). Due to the difficult location and unsuccessful closure from the luminal side, the defect was successfully closed from inside the tunnel using two clips (Figure 1, Panel C). The patient was kept nil per os (NPO) and on IV antibiotics. She developed abdominal pain and leukocytosis (WBC 13.6 k/ul) on postop day 1, but no fever. Computed tomography (CT) scan with oral contrast two days later revealed no leak. The patient improved clinically over the next few days and was eventually started on clear liquid diet with good tolerance. She was discharged home on postoperative day 6. A follow up abdominal X-ray 3 months later showed only one clip in the gastric outlet/duodenal bulb area (Figure 1, panel D).
Discussion: Foreign objects in the wall of the gastrointestinal tract gradually resurface and fall into the lumen. Following this principal, we closed the mucosal defect in our case with clips from inside the submucosal tunnel. A follow up abdominal X-ray 3 months later showed only one clip in the area, consistent with the above notion. This intervention prevented our patient from having a leak and eventually avoided surgery. Our case supports closing mucosal defects from inside the tunnel during POEM and GPOEM procedures when luminal side closure is unsuccessful and can prevent leaks and surgical intervention.
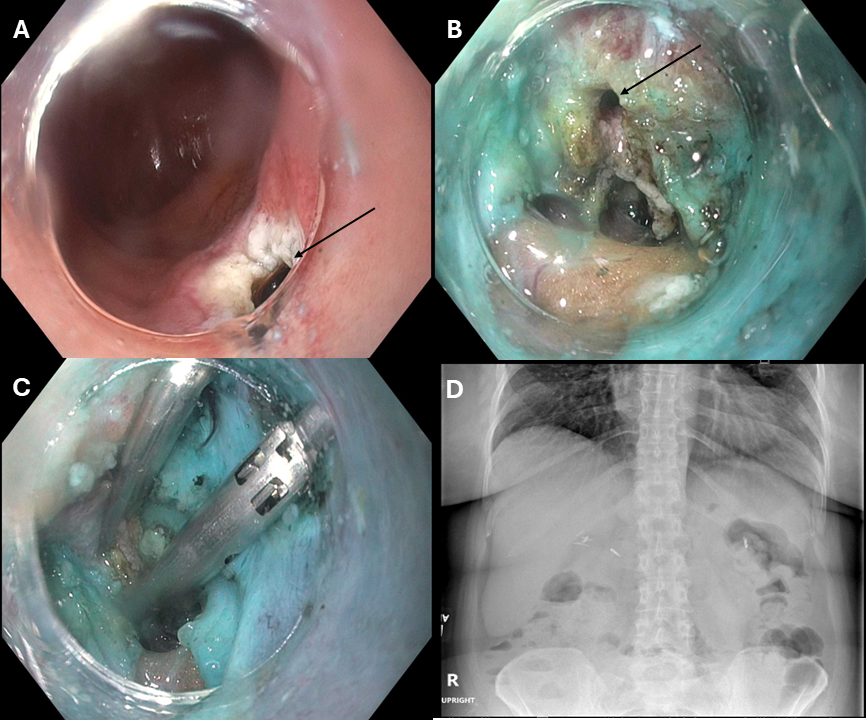
Figure: Figure 1. Panel A: luminal view of a thermal mucosal injury in the duodenal bulb just distal to the pylorus. Panel B: a view of the mucosal defect from inside the tunnel. Panel C: closure of the mucosal defect from inside the tunnel using two clips. Panel D: abdominal X-ray 3 months later showing only one clip in the gastric outlet/duodenal bulb area.
Disclosures:
Falak Hamo indicated no relevant financial relationships.
Shahryar Khan indicated no relevant financial relationships.
Mashal Alam Khan indicated no relevant financial relationships.
Mollie Jackson indicated no relevant financial relationships.
Kevin Liu indicated no relevant financial relationships.
Salih Samo: Castle Biosciences – Advisory Committee/Board Member, Consultant, Speakers Bureau. EndoGastric Solutions – Speakers Bureau. Evoke – Speakers Bureau. Medtronic – Speakers Bureau. Phathom – Speakers Bureau. Sanofi – Advisory Committee/Board Member, Speakers Bureau. Takeda – Speakers Bureau.
Falak Hamo, MD1, Shahryar Khan, MD2, Mashal Alam Khan, MBBS3, Mollie Jackson, DO2, Kevin Liu, MD4, Salih Samo, MD, MSci1. P5755 - No Light at the End of the Tunnel: Closing a Mucosal Defect from Inside the Tunnel During G-POEM Procedure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas Medical Center, Overland Park, KS; 2University of Kansas Medical Center, Kansas City, KS; 3Khyber Medical University, Kansas City, KS; 4Banner University Medical Center, Phoenix, AZ
Introduction: Mucosal injuries during peroral endoscopic myotomy (POEM) can lead to leaks and infection. Therefore, recognizing such injuries and closing them is important to avoid adverse outcomes requiring surgery. We report a case of gastric POEM (GPOEM) with a mucosal defect closure from inside the tunnel due to difficult luminal side closure.
Case Description/
Methods: A 48-year-old female with gastroparesis (gastric emptying study with 68% retention at 4 hours) with abdominal pain after eating, epigastric fullness, early satiety, bloating, nausea with rare vomiting, not feeling hungry, and 60 lbs weight loss over two years underwent GPOEM due to concern about long term neurological side effects with metoclopramide in the setting of lamotrigine use for bipolar disorder. Her gastroparesis cardinal symptom index (GCS I) was 3.75.
During the GPOEM procedure a significant bleeding occurred during submucosal tunneling requiring cautery use, which led to a thermal mucosal injury in the duodenal bulb just distal to the pylorus (Figure 1, panel A. Panel B represents a view of the mucosal defect from inside the tunnel). Due to the difficult location and unsuccessful closure from the luminal side, the defect was successfully closed from inside the tunnel using two clips (Figure 1, Panel C). The patient was kept nil per os (NPO) and on IV antibiotics. She developed abdominal pain and leukocytosis (WBC 13.6 k/ul) on postop day 1, but no fever. Computed tomography (CT) scan with oral contrast two days later revealed no leak. The patient improved clinically over the next few days and was eventually started on clear liquid diet with good tolerance. She was discharged home on postoperative day 6. A follow up abdominal X-ray 3 months later showed only one clip in the gastric outlet/duodenal bulb area (Figure 1, panel D).
Discussion: Foreign objects in the wall of the gastrointestinal tract gradually resurface and fall into the lumen. Following this principal, we closed the mucosal defect in our case with clips from inside the submucosal tunnel. A follow up abdominal X-ray 3 months later showed only one clip in the area, consistent with the above notion. This intervention prevented our patient from having a leak and eventually avoided surgery. Our case supports closing mucosal defects from inside the tunnel during POEM and GPOEM procedures when luminal side closure is unsuccessful and can prevent leaks and surgical intervention.
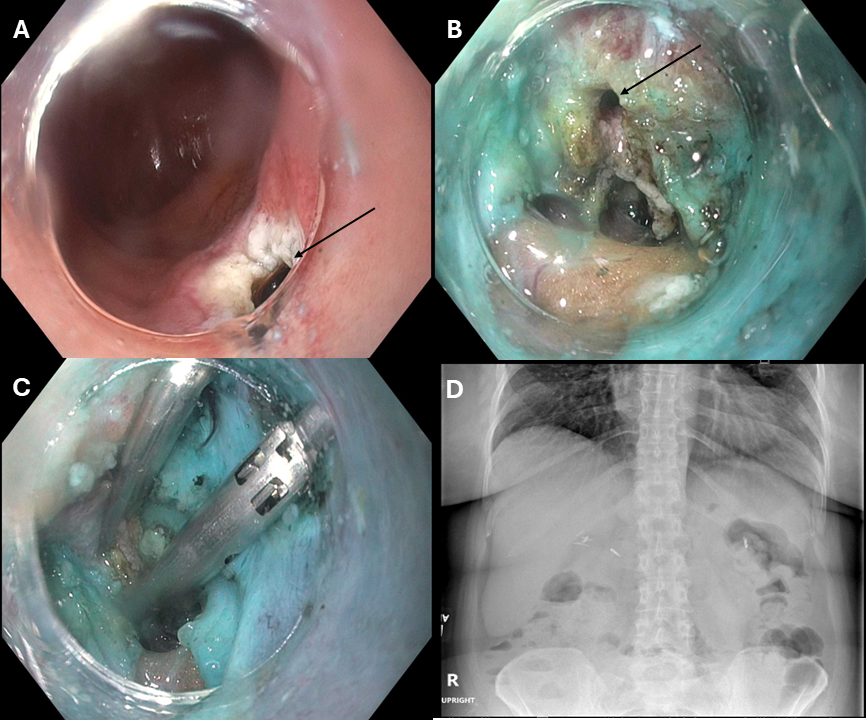
Figure: Figure 1. Panel A: luminal view of a thermal mucosal injury in the duodenal bulb just distal to the pylorus. Panel B: a view of the mucosal defect from inside the tunnel. Panel C: closure of the mucosal defect from inside the tunnel using two clips. Panel D: abdominal X-ray 3 months later showing only one clip in the gastric outlet/duodenal bulb area.
Disclosures:
Falak Hamo indicated no relevant financial relationships.
Shahryar Khan indicated no relevant financial relationships.
Mashal Alam Khan indicated no relevant financial relationships.
Mollie Jackson indicated no relevant financial relationships.
Kevin Liu indicated no relevant financial relationships.
Salih Samo: Castle Biosciences – Advisory Committee/Board Member, Consultant, Speakers Bureau. EndoGastric Solutions – Speakers Bureau. Evoke – Speakers Bureau. Medtronic – Speakers Bureau. Phathom – Speakers Bureau. Sanofi – Advisory Committee/Board Member, Speakers Bureau. Takeda – Speakers Bureau.
Falak Hamo, MD1, Shahryar Khan, MD2, Mashal Alam Khan, MBBS3, Mollie Jackson, DO2, Kevin Liu, MD4, Salih Samo, MD, MSci1. P5755 - No Light at the End of the Tunnel: Closing a Mucosal Defect from Inside the Tunnel During G-POEM Procedure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
