Tuesday Poster Session
Category: Interventional Endoscopy
P5728 - Endoscopic Management of Bouveret Syndrome in a High-Risk Surgical Candidate
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MV
Meghana Vankina, MD (she/her/hers)
Tulane School of Medicine
New Orleans, LA
Presenting Author(s)
Meghana Vankina, MD1, Jayaprakash Sreenarasimhaiah, MD, FACG2
1Tulane School of Medicine, New Orleans, LA; 2Baylor Scott & White Medical Center Irving, Dallas, TX
Introduction: Bouveret syndrome is a rare medical condition where gallstones pass through a bilioenteric fistula before they become lodged in either the stomach or duodenum thereby creating a gastric outlet obstruction. This condition primarily affects elderly patients with multiple comorbidities and has a high morbidity and mortality rate1. Currently, no official standards exist for endoscopic interventions in Bouveret syndrome. We present a case of Bouveret syndrome in a medically complex patient who underwent endoscopic treatment because surgical options were not viable.
Case Description/
Methods: A 76-year-old female with an extensive medical history, including congestive heart failure, coronary artery disease, chronic kidney disease, chronic obstructive pulmonary disease, and gallstones, presented to the emergency department with chest pain, nausea, vomiting, and abdominal distention. Her chronic cholecystitis was being managed with a cholecystostomy tube for over 18 months, but was removed two months prior to admission. Computed tomography (CT) scan revealed a large calcified gallstone trapped in the gastric antrum along with pneumobilia which confirmed Bouveret syndrome originating from a cholecystogastric fistula. The endoscopy procedure revealed a large stone blockage at the duodenal bulb. Endoscopic Holmium laser lithotripsy was performed which successfully fragmented the gallstone so it could be passed. The patient developed a perforation days following the procedure. Surgical intervention was considered, but she was too high risk for anesthesia. A multidisciplinary team discussion supported her decision to move to hospice care for comfort-based treatment instead of pursuing additional high-risk medical interventions.
Discussion: This case presents endoscopic Holmium laser lithotripsy as a minimally invasive option to treat Bouveret syndrome among high risk surgical patients. The patient experienced obstruction relief but later developed a perforation which demonstrates the need for thorough risk evaluation along with close monitoring after procedures. Multidisciplinary coordination across specialities becomes essential when treating medically complex patients. This case contributes to the growing clinical experience in managing Bouveret syndrome and may help guide future best practices.
References:
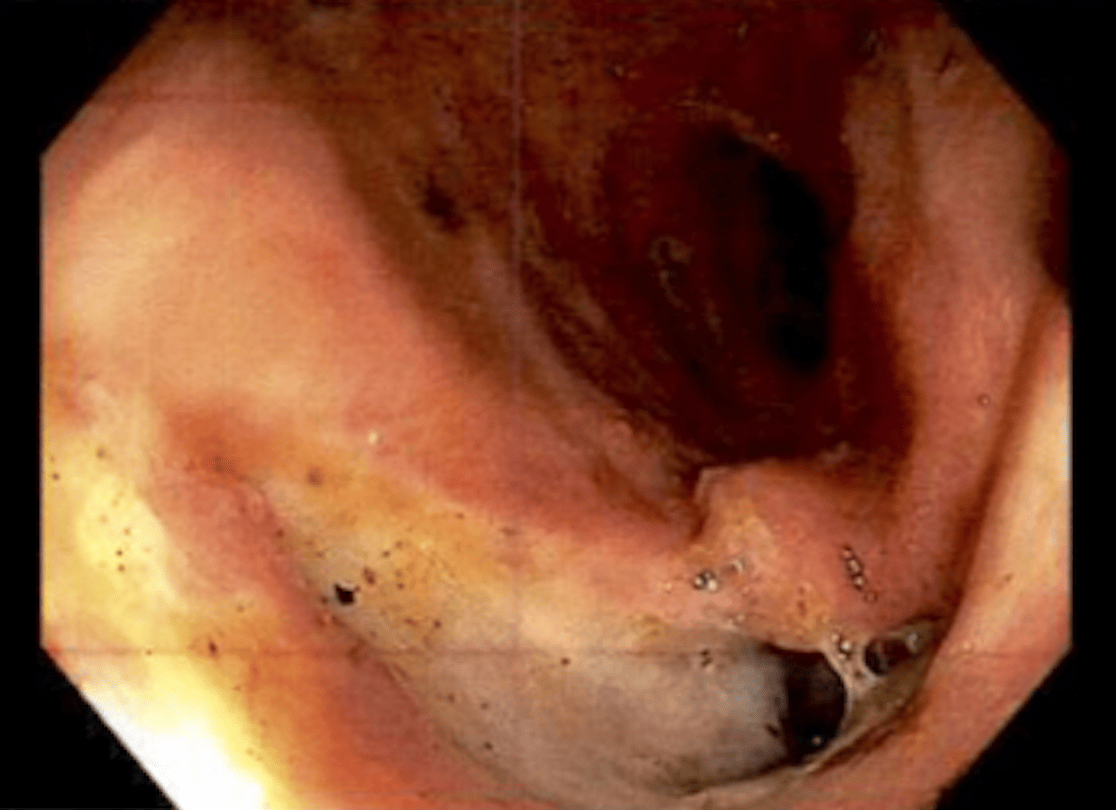
Figure: Endoscopic view of a 4 cm impacted gallstone causing gastric outlet obstruction in the duodenal bulb, consistent with Bouveret syndrome.

Figure: Endoscopic view of the cholecystogastric fistula. An opening between the gallbladder and duodenal bulb is seen, confirming the route of gallstone migration in Bouveret syndrome.
Disclosures:
Meghana Vankina indicated no relevant financial relationships.
Jayaprakash Sreenarasimhaiah indicated no relevant financial relationships.
Meghana Vankina, MD1, Jayaprakash Sreenarasimhaiah, MD, FACG2. P5728 - Endoscopic Management of Bouveret Syndrome in a High-Risk Surgical Candidate, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tulane School of Medicine, New Orleans, LA; 2Baylor Scott & White Medical Center Irving, Dallas, TX
Introduction: Bouveret syndrome is a rare medical condition where gallstones pass through a bilioenteric fistula before they become lodged in either the stomach or duodenum thereby creating a gastric outlet obstruction. This condition primarily affects elderly patients with multiple comorbidities and has a high morbidity and mortality rate1. Currently, no official standards exist for endoscopic interventions in Bouveret syndrome. We present a case of Bouveret syndrome in a medically complex patient who underwent endoscopic treatment because surgical options were not viable.
Case Description/
Methods: A 76-year-old female with an extensive medical history, including congestive heart failure, coronary artery disease, chronic kidney disease, chronic obstructive pulmonary disease, and gallstones, presented to the emergency department with chest pain, nausea, vomiting, and abdominal distention. Her chronic cholecystitis was being managed with a cholecystostomy tube for over 18 months, but was removed two months prior to admission. Computed tomography (CT) scan revealed a large calcified gallstone trapped in the gastric antrum along with pneumobilia which confirmed Bouveret syndrome originating from a cholecystogastric fistula. The endoscopy procedure revealed a large stone blockage at the duodenal bulb. Endoscopic Holmium laser lithotripsy was performed which successfully fragmented the gallstone so it could be passed. The patient developed a perforation days following the procedure. Surgical intervention was considered, but she was too high risk for anesthesia. A multidisciplinary team discussion supported her decision to move to hospice care for comfort-based treatment instead of pursuing additional high-risk medical interventions.
Discussion: This case presents endoscopic Holmium laser lithotripsy as a minimally invasive option to treat Bouveret syndrome among high risk surgical patients. The patient experienced obstruction relief but later developed a perforation which demonstrates the need for thorough risk evaluation along with close monitoring after procedures. Multidisciplinary coordination across specialities becomes essential when treating medically complex patients. This case contributes to the growing clinical experience in managing Bouveret syndrome and may help guide future best practices.
References:
- Turner AR, Kudaravalli P, Al-Musawi JH, Ahmad H. Bouveret Syndrome (Bilioduodenal Fistula). In: StatPearls. Treasure Island (FL): StatPearls Publishing; March 13, 2023.
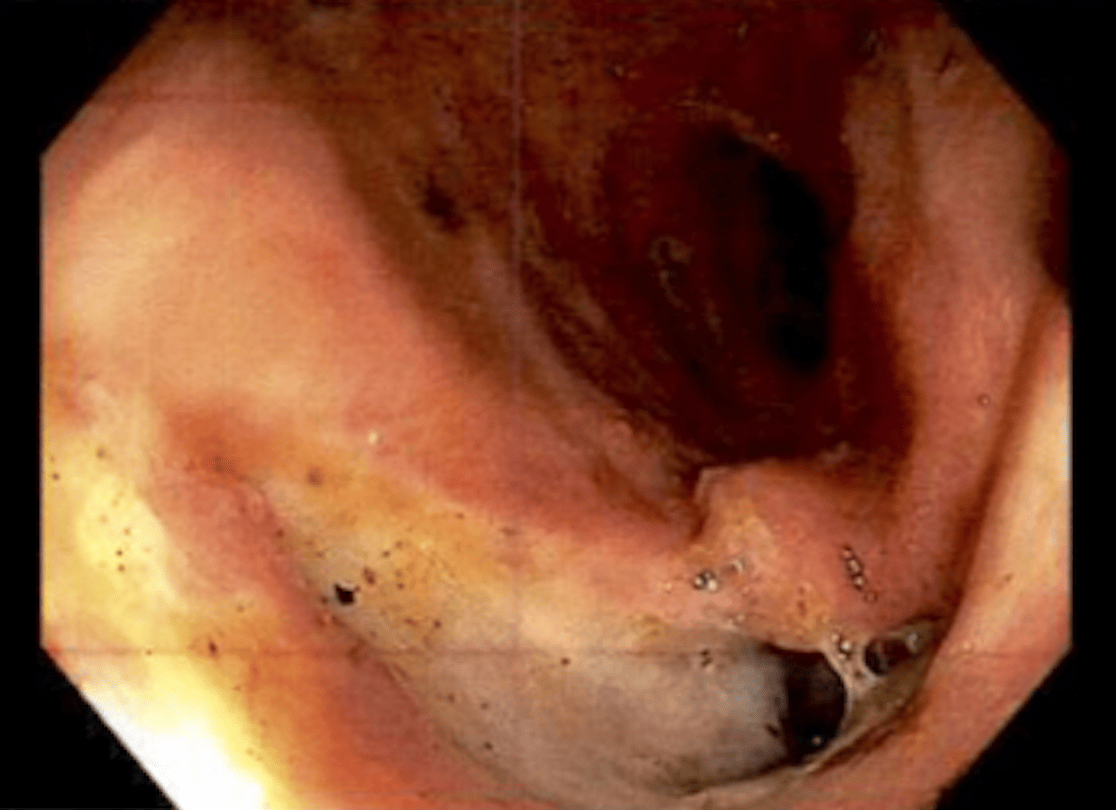
Figure: Endoscopic view of a 4 cm impacted gallstone causing gastric outlet obstruction in the duodenal bulb, consistent with Bouveret syndrome.

Figure: Endoscopic view of the cholecystogastric fistula. An opening between the gallbladder and duodenal bulb is seen, confirming the route of gallstone migration in Bouveret syndrome.
Disclosures:
Meghana Vankina indicated no relevant financial relationships.
Jayaprakash Sreenarasimhaiah indicated no relevant financial relationships.
Meghana Vankina, MD1, Jayaprakash Sreenarasimhaiah, MD, FACG2. P5728 - Endoscopic Management of Bouveret Syndrome in a High-Risk Surgical Candidate, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

