Tuesday Poster Session
Category: Interventional Endoscopy
P5725 - Salvage Endoscopic Submucosal Dissection After Neoadjuvant Chemoradiation for Esophageal Adenocarcinoma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Connor J. Eggleston, MD (he/him/his)
University of Colorado Anschutz Medical Campus
Aurora, CO
Presenting Author(s)
Connor J. Eggleston, MD1, Thomas Enke, MD2, Mohammad Bilal, MD1
1University of Colorado Anschutz Medical Campus, Aurora, CO; 2University of Colorado, Aurora, CO
Introduction: Definitive chemoradiotherapy (CRT) for locally advanced esophageal adenocarcinoma (EAC) is used in non-operative candidates or those who wish to avoid the morbidity associated with esophagectomy. Locoregional failure following CRT is common. The role of salvage endoscopic submucosal dissection (ESD) for EAC following locoregional failure is not clear.
We report the case of salvage ESD in a patient with residual malignancy following CRT who deferred esophagectomy.
Case Description/
Methods: An 81-year-old male with a history of Barrett’s esophagus (BE) was found to have a 3 cm mass in the distal esophagus during surveillance upper endoscopy (EGD). Biopsies confirmed EAC and was staged T3 N0 M0 by endoscopic ultrasound (EUS) and positron emission tomography-computed tomography. Esophagectomy was recommended but declined by patient in favor of definitive CRT. EGD (Figure 1) and EUS following CRT revealed residual disease extending to the submucosa. Esophagectomy was recommended but again declined by patient. After extensive multidisciplinary discussion, decision was made to attempt salvage ESD.
ESD (Figure 2) was performed and was challenging due to scarring and fibrosis due to prior CRT. Intra-procedure course was complicated by significant bleeding after 80% of the lesion had been resected from the muscularis propria. The source of bleeding could not be visualized and hemostasis was unsuccessful despite multiple attempts using various modalities. Decision was made to convert to hybrid ESD. A snare was used to resect the remaining lesion. The bleeding was localized and treated with hemostatic forceps. A covered esophageal stent was placed for secondary to reduce the risk of stricture formation. Post-procedure course was uncomplicated, and the patient was discharged home the following day. Pathology revealed poorly differentiated EAC extending to the submucosa with positive deep margins. Surgical resection was again recommended but deferred. Over four months follow-up, there has been no evidence of recurrent EAC at the site of prior ESD. High-grade dysplasia has been detected on biopsies from the residual segment of BE and treated with endoscopic mucosal resection.
Discussion: This case demonstrates that ESD can be a viable salvage therapy for locoregional failure of EAC following definitive CRT in non-operative candidates. However, ESD in these cases can be technically challenging due to scarring and fibrosis from previous therapy.
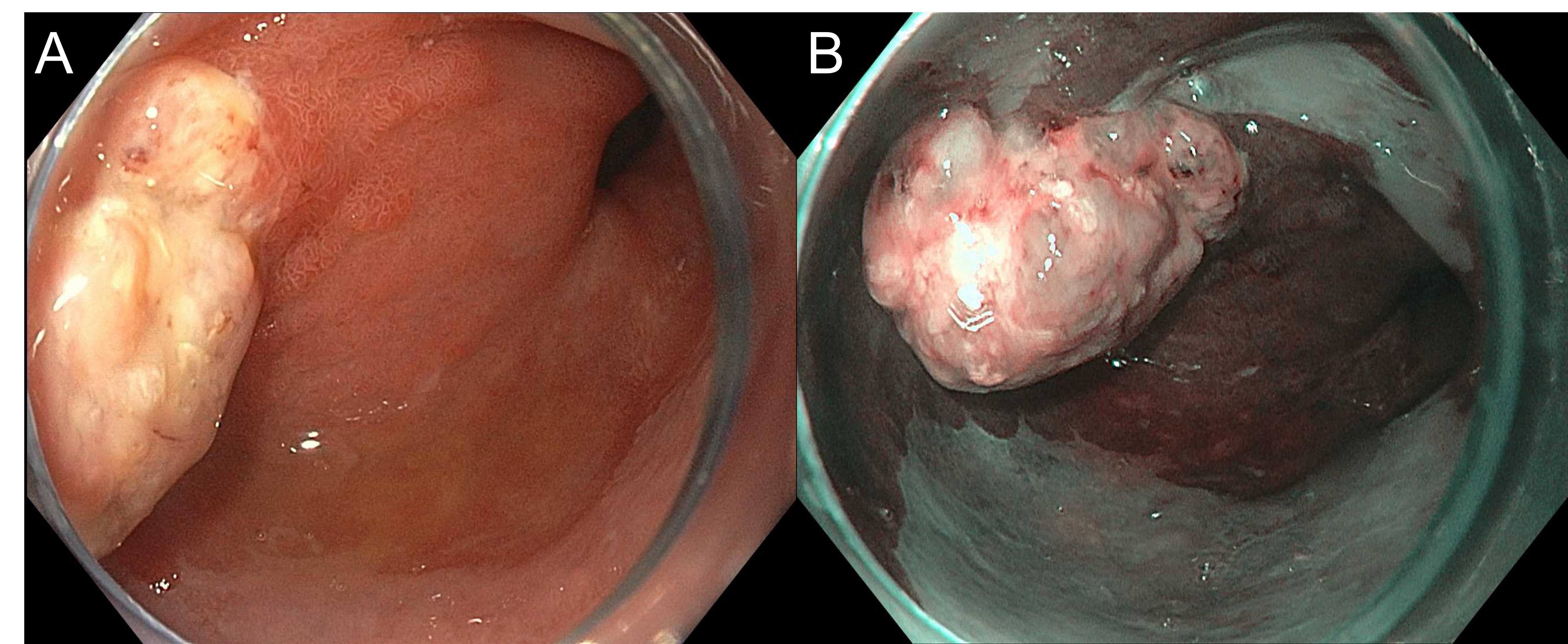
Figure: Figure 1. Residual esophageal adenocarcinoma following definitive chemoradiotherapy visualized using high-definition white light endoscopy (A) and virtual chromoendoscopy (B).
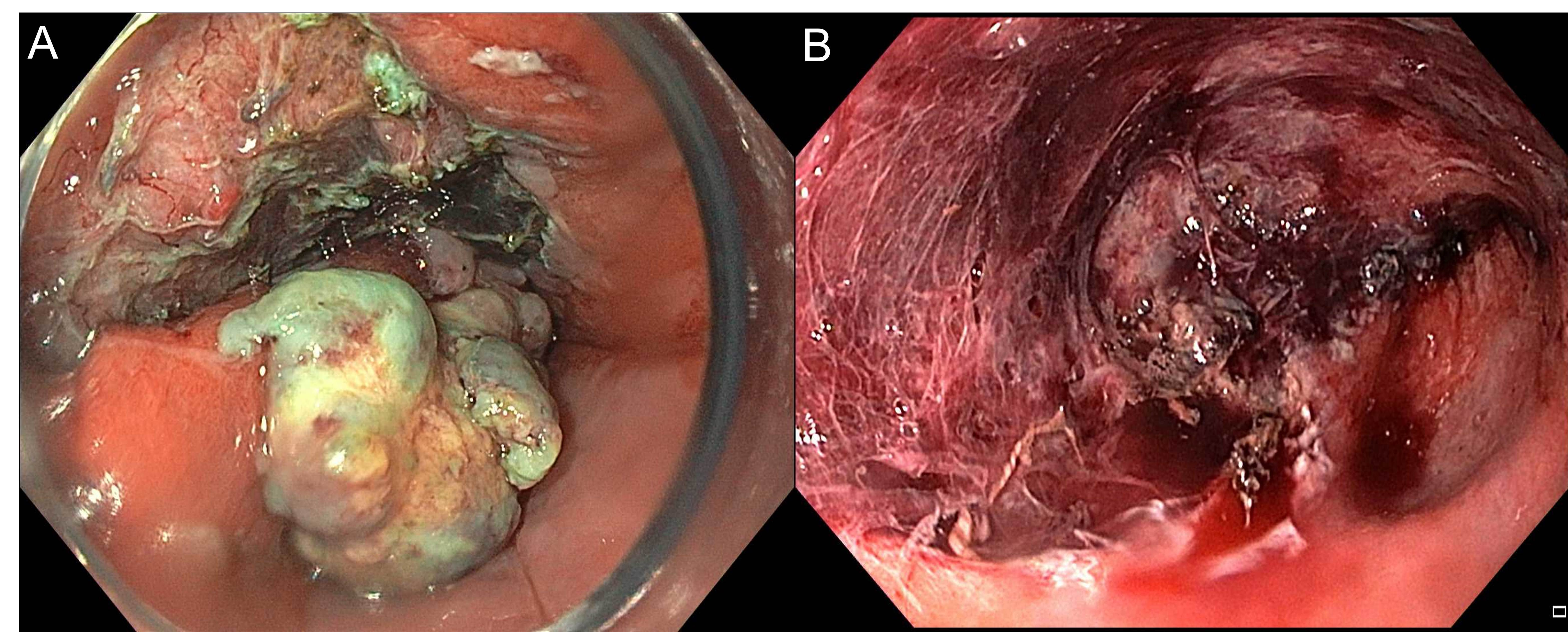
Figure: Figure 2. Representative hybrid endoscopic submucosal dissection images demonstrating initial dissection (A) and final resection margins (B).
Disclosures:
Connor Eggleston indicated no relevant financial relationships.
Thomas Enke indicated no relevant financial relationships.
Mohammad Bilal: Aspero Medical – Consultant. Boston Scientific – Consultant. Cook Endoscopy – Consultant. Steris Endoscopy – Consultant.
Connor J. Eggleston, MD1, Thomas Enke, MD2, Mohammad Bilal, MD1. P5725 - Salvage Endoscopic Submucosal Dissection After Neoadjuvant Chemoradiation for Esophageal Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Colorado Anschutz Medical Campus, Aurora, CO; 2University of Colorado, Aurora, CO
Introduction: Definitive chemoradiotherapy (CRT) for locally advanced esophageal adenocarcinoma (EAC) is used in non-operative candidates or those who wish to avoid the morbidity associated with esophagectomy. Locoregional failure following CRT is common. The role of salvage endoscopic submucosal dissection (ESD) for EAC following locoregional failure is not clear.
We report the case of salvage ESD in a patient with residual malignancy following CRT who deferred esophagectomy.
Case Description/
Methods: An 81-year-old male with a history of Barrett’s esophagus (BE) was found to have a 3 cm mass in the distal esophagus during surveillance upper endoscopy (EGD). Biopsies confirmed EAC and was staged T3 N0 M0 by endoscopic ultrasound (EUS) and positron emission tomography-computed tomography. Esophagectomy was recommended but declined by patient in favor of definitive CRT. EGD (Figure 1) and EUS following CRT revealed residual disease extending to the submucosa. Esophagectomy was recommended but again declined by patient. After extensive multidisciplinary discussion, decision was made to attempt salvage ESD.
ESD (Figure 2) was performed and was challenging due to scarring and fibrosis due to prior CRT. Intra-procedure course was complicated by significant bleeding after 80% of the lesion had been resected from the muscularis propria. The source of bleeding could not be visualized and hemostasis was unsuccessful despite multiple attempts using various modalities. Decision was made to convert to hybrid ESD. A snare was used to resect the remaining lesion. The bleeding was localized and treated with hemostatic forceps. A covered esophageal stent was placed for secondary to reduce the risk of stricture formation. Post-procedure course was uncomplicated, and the patient was discharged home the following day. Pathology revealed poorly differentiated EAC extending to the submucosa with positive deep margins. Surgical resection was again recommended but deferred. Over four months follow-up, there has been no evidence of recurrent EAC at the site of prior ESD. High-grade dysplasia has been detected on biopsies from the residual segment of BE and treated with endoscopic mucosal resection.
Discussion: This case demonstrates that ESD can be a viable salvage therapy for locoregional failure of EAC following definitive CRT in non-operative candidates. However, ESD in these cases can be technically challenging due to scarring and fibrosis from previous therapy.
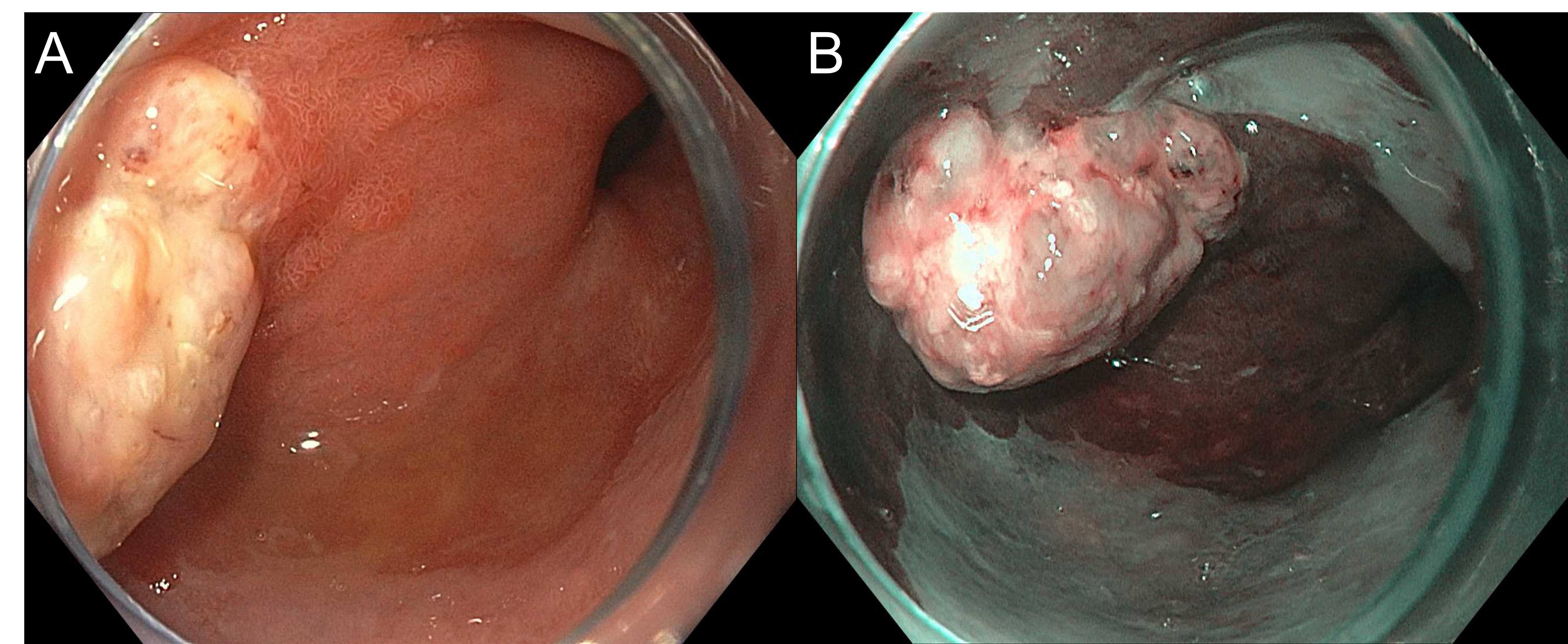
Figure: Figure 1. Residual esophageal adenocarcinoma following definitive chemoradiotherapy visualized using high-definition white light endoscopy (A) and virtual chromoendoscopy (B).
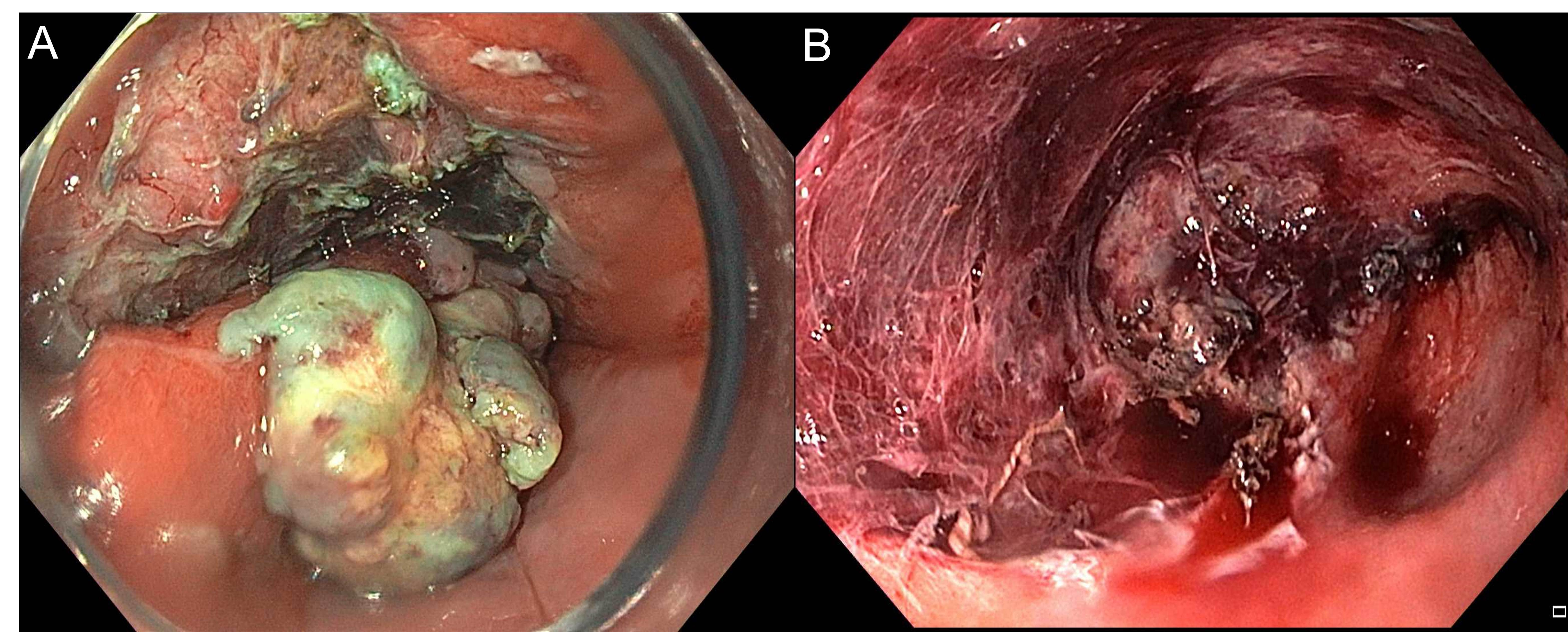
Figure: Figure 2. Representative hybrid endoscopic submucosal dissection images demonstrating initial dissection (A) and final resection margins (B).
Disclosures:
Connor Eggleston indicated no relevant financial relationships.
Thomas Enke indicated no relevant financial relationships.
Mohammad Bilal: Aspero Medical – Consultant. Boston Scientific – Consultant. Cook Endoscopy – Consultant. Steris Endoscopy – Consultant.
Connor J. Eggleston, MD1, Thomas Enke, MD2, Mohammad Bilal, MD1. P5725 - Salvage Endoscopic Submucosal Dissection After Neoadjuvant Chemoradiation for Esophageal Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
