Tuesday Poster Session
Category: Interventional Endoscopy
P5723 - Lumen-Apposing Metal Stent Placement for Refractory Gastrojejunal Anastomosis Stricture Management
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DP
Deep Patel, BS, MD
University of South Florida Health
Valrico, FL
Presenting Author(s)
Deep Patel, BS, MD1, Brijesh B. Patel, MD2
1University of South Florida Health, Valrico, FL; 2University of South Florida, James A. Haley VA Hospital, Tampa, FL
Introduction: Roux-en-Y gastric bypass involves connecting the distal small bowel with a newly created gastric pouch with a gastrojejunal (GJ) anastomosis. These anastomoses can stricture with some literature estimating incidence ranging from 2-7%. One meta-analysis showed that a wide majority of cases are managed with the less invasive Through The Scope (TTS) balloon dilation though surgical revision also is an option. We present a case of a severe anastomosis stricture persisting after multiple balloon dilations, leading to placement of a Lumen-Apposing Metal Stent (LAMS).
Case Description/
Methods: Patient is a 53-year-old male with prior Roux-en-Y that presented with nausea, vomiting, and epigastric pain suggestive of gastric outlet obstruction (GOO). Endoscopy showed a GJ anastomotic stricture and was successfully managed with a TTS balloon dilation.
3 months later, patient presented for worsening symptoms. Urine drug screen was positive for cocaine, causing endoscopy to be delayed. Given prolonged NPO course, TPN was initiated. EGD showed a dilated gastric pouch with multiple large ulcerations, and severely stenosed and ulcerated GJ anastomosis with obliterated lumen. The stricture was successfully dilated and repeat endoscopy after 2 days showed the anastomosis appearing more patent though still strictured. TTS dilation was successful with a 10mm balloon and a jejunal dobhoff tube (DHT) was placed. The patient was weaned off TPN with increase tolerance to tube feeds and liquid diet. However, DHT became dislodged, so repeat endoscopy was done showing a strictured down anastomosis. TTS dilation was performed again with a 10mm balloon but unable to traverse even the XP scope.
A few weeks later, another EGD with dilation was performed and placement of 8 mm fully covered metal stent (biliary stent) was placed though subsequent endoscopy showed stent migration (Figure 1) leading to placement of a 15mm x 10mm LAMS (Figure 2). After placement of LAMS, patient tolerated oral intake without any symptoms of gastric outlet obstruction. He has been off TPN and has not required enteral nutrition. Patient continues to maintain steady weight.
Discussion: LAMS are a newer option offering a minimally invasive approach that theoretically decreases risk of stent migration and mucosal ingrowth. Multiple studies looking at LAMS managed GJ stricture have shown ~ 60% success in resolution with minimal adverse risks making it a viable option that can become mainstay of GJ anastomotic stricture management in the future.
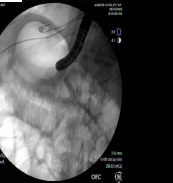
Figure: Pinpoint GJ anastomotic stricture prior to LAMS placement.

Figure: Fluoroscopic evaluation following LAMS placement.
Disclosures:
Deep Patel indicated no relevant financial relationships.
Brijesh Patel indicated no relevant financial relationships.
Deep Patel, BS, MD1, Brijesh B. Patel, MD2. P5723 - Lumen-Apposing Metal Stent Placement for Refractory Gastrojejunal Anastomosis Stricture Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of South Florida Health, Valrico, FL; 2University of South Florida, James A. Haley VA Hospital, Tampa, FL
Introduction: Roux-en-Y gastric bypass involves connecting the distal small bowel with a newly created gastric pouch with a gastrojejunal (GJ) anastomosis. These anastomoses can stricture with some literature estimating incidence ranging from 2-7%. One meta-analysis showed that a wide majority of cases are managed with the less invasive Through The Scope (TTS) balloon dilation though surgical revision also is an option. We present a case of a severe anastomosis stricture persisting after multiple balloon dilations, leading to placement of a Lumen-Apposing Metal Stent (LAMS).
Case Description/
Methods: Patient is a 53-year-old male with prior Roux-en-Y that presented with nausea, vomiting, and epigastric pain suggestive of gastric outlet obstruction (GOO). Endoscopy showed a GJ anastomotic stricture and was successfully managed with a TTS balloon dilation.
3 months later, patient presented for worsening symptoms. Urine drug screen was positive for cocaine, causing endoscopy to be delayed. Given prolonged NPO course, TPN was initiated. EGD showed a dilated gastric pouch with multiple large ulcerations, and severely stenosed and ulcerated GJ anastomosis with obliterated lumen. The stricture was successfully dilated and repeat endoscopy after 2 days showed the anastomosis appearing more patent though still strictured. TTS dilation was successful with a 10mm balloon and a jejunal dobhoff tube (DHT) was placed. The patient was weaned off TPN with increase tolerance to tube feeds and liquid diet. However, DHT became dislodged, so repeat endoscopy was done showing a strictured down anastomosis. TTS dilation was performed again with a 10mm balloon but unable to traverse even the XP scope.
A few weeks later, another EGD with dilation was performed and placement of 8 mm fully covered metal stent (biliary stent) was placed though subsequent endoscopy showed stent migration (Figure 1) leading to placement of a 15mm x 10mm LAMS (Figure 2). After placement of LAMS, patient tolerated oral intake without any symptoms of gastric outlet obstruction. He has been off TPN and has not required enteral nutrition. Patient continues to maintain steady weight.
Discussion: LAMS are a newer option offering a minimally invasive approach that theoretically decreases risk of stent migration and mucosal ingrowth. Multiple studies looking at LAMS managed GJ stricture have shown ~ 60% success in resolution with minimal adverse risks making it a viable option that can become mainstay of GJ anastomotic stricture management in the future.
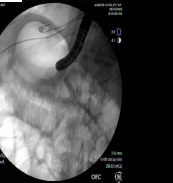
Figure: Pinpoint GJ anastomotic stricture prior to LAMS placement.

Figure: Fluoroscopic evaluation following LAMS placement.
Disclosures:
Deep Patel indicated no relevant financial relationships.
Brijesh Patel indicated no relevant financial relationships.
Deep Patel, BS, MD1, Brijesh B. Patel, MD2. P5723 - Lumen-Apposing Metal Stent Placement for Refractory Gastrojejunal Anastomosis Stricture Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
