Tuesday Poster Session
Category: Interventional Endoscopy
P5715 - Duodenal-Cutaneous Fistula Closure via LAMS Stent: A Minimally Invasive Solution for Post-Graham Patch Failure
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vishnu Yanamaladoddi, MD
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Award: ACG Presidential Poster Award
Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Shree Laya Vemula, MD2, Sandeep Chikkam, MD, DNBSS3, Pir Shah, MD1, Indu Srinivasan, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2NYC Health + Hospitals/South Brooklyn Health, Brooklyn, NY; 3Asian Institute of Gastroenterology, Hyderabad, Telangana, India
Introduction: Duodenal ulcers are surgical emergencies often managed with a Graham patch repair. Persistent leaks may occur, sometimes progressing to entero-cutaneous fistulas. Traditionally, these complications are treated with surgical re-patching or gastrojejunostomy to divert enteric contents and promote healing. Lumen-apposing metal stents (LAMS), originally designed to create secure fistulous tracts, have seen expanded clinical use. We present the case of a 70-year-old who developed a duodenal-cutaneous fistula following Graham patch repair and was successfully treated with a LAMS.
Case Description/
Methods: A 70-year-old female with type 2 diabetes and complex surgical history including Graham patch repair of a perforated duodenal ulcer and open cholecystectomy presented with two weeks of right upper quadrant pain, erythema over a surgical scar, and fever. She had chronic postoperative drainage and recurrent abscesses for two years. Imaging revealed a 6.5 cm gas and fluid collection with a fistulous tract from the duodenal bulb to a collection in the gallbladder fossa extending into the abdominal wall, consistent with an enteric-origin abscess. Initial management included bedside incision and drainage with empiric antibiotics. Endoscopy identified a duodenal ulcer with an embedded suture but no active bleeding or visible fistula. A percutaneous drain was placed for abdominal abscess drainage, and the suture was removed endoscopically using a loop cutter and Roth forceps. To promote healing, a LAMS was placed endoscopically from the pylorus to the second portion of the duodenum, bypassing the affected area. The patient’s symptoms improved, and follow-up CT with oral contrast showed no leakage. On serial follow-up, the cutaneous wound healed completely. After elective LAMS removal, a duodenal stricture was noted and dilated. The patient reported complete resolution of her symptoms.
Discussion: Endoscopic creation of a stomach-to-small bowel bypass using LAMS represents a groundbreaking advancement in managing complex duodenal ulcer complications. This minimally invasive approach offers a promising alternative for persistent duodenal leaks or fistulas, especially after Graham patch failure where surgical options carry significant risk. Early reports demonstrate high technical success with ulcer healing and fistula closure, avoiding invasive reoperation. While this approach shows remarkable promise, long-term data is needed to validate durability and safety.
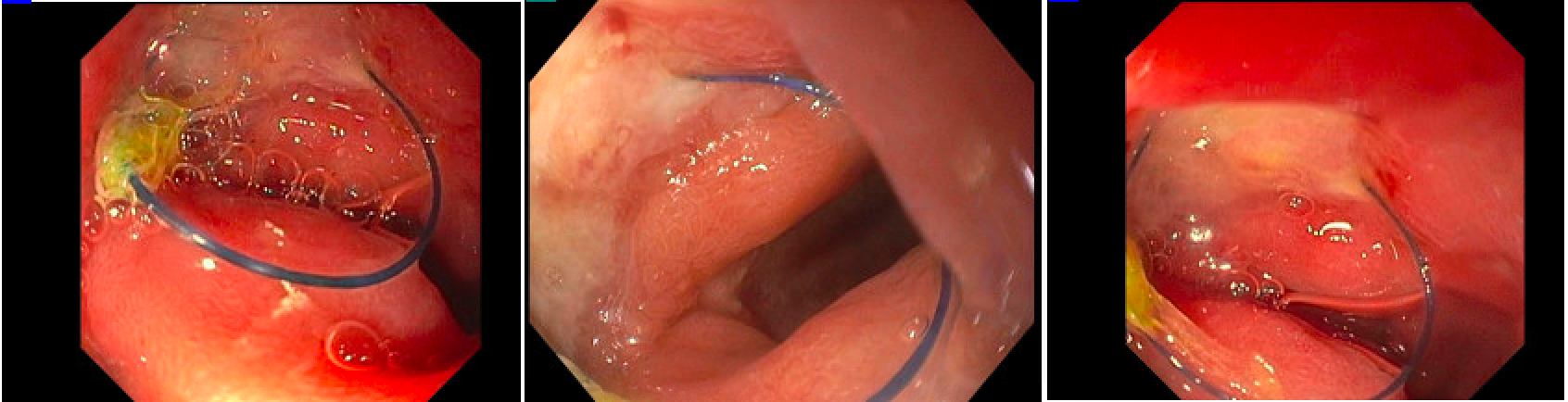
Figure: 1 - Persistent duodenal suture from Graham patch repair

Figure: 2A - Lumen apposing metallic stent (LAMS) placement creating duodenal bypass
2B - Axial CT showing stent placement
Disclosures:
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Shree Laya Vemula indicated no relevant financial relationships.
Sandeep Chikkam indicated no relevant financial relationships.
Pir Shah indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Shree Laya Vemula, MD2, Sandeep Chikkam, MD, DNBSS3, Pir Shah, MD1, Indu Srinivasan, MD1. P5715 - Duodenal-Cutaneous Fistula Closure via LAMS Stent: A Minimally Invasive Solution for Post-Graham Patch Failure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Shree Laya Vemula, MD2, Sandeep Chikkam, MD, DNBSS3, Pir Shah, MD1, Indu Srinivasan, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2NYC Health + Hospitals/South Brooklyn Health, Brooklyn, NY; 3Asian Institute of Gastroenterology, Hyderabad, Telangana, India
Introduction: Duodenal ulcers are surgical emergencies often managed with a Graham patch repair. Persistent leaks may occur, sometimes progressing to entero-cutaneous fistulas. Traditionally, these complications are treated with surgical re-patching or gastrojejunostomy to divert enteric contents and promote healing. Lumen-apposing metal stents (LAMS), originally designed to create secure fistulous tracts, have seen expanded clinical use. We present the case of a 70-year-old who developed a duodenal-cutaneous fistula following Graham patch repair and was successfully treated with a LAMS.
Case Description/
Methods: A 70-year-old female with type 2 diabetes and complex surgical history including Graham patch repair of a perforated duodenal ulcer and open cholecystectomy presented with two weeks of right upper quadrant pain, erythema over a surgical scar, and fever. She had chronic postoperative drainage and recurrent abscesses for two years. Imaging revealed a 6.5 cm gas and fluid collection with a fistulous tract from the duodenal bulb to a collection in the gallbladder fossa extending into the abdominal wall, consistent with an enteric-origin abscess. Initial management included bedside incision and drainage with empiric antibiotics. Endoscopy identified a duodenal ulcer with an embedded suture but no active bleeding or visible fistula. A percutaneous drain was placed for abdominal abscess drainage, and the suture was removed endoscopically using a loop cutter and Roth forceps. To promote healing, a LAMS was placed endoscopically from the pylorus to the second portion of the duodenum, bypassing the affected area. The patient’s symptoms improved, and follow-up CT with oral contrast showed no leakage. On serial follow-up, the cutaneous wound healed completely. After elective LAMS removal, a duodenal stricture was noted and dilated. The patient reported complete resolution of her symptoms.
Discussion: Endoscopic creation of a stomach-to-small bowel bypass using LAMS represents a groundbreaking advancement in managing complex duodenal ulcer complications. This minimally invasive approach offers a promising alternative for persistent duodenal leaks or fistulas, especially after Graham patch failure where surgical options carry significant risk. Early reports demonstrate high technical success with ulcer healing and fistula closure, avoiding invasive reoperation. While this approach shows remarkable promise, long-term data is needed to validate durability and safety.
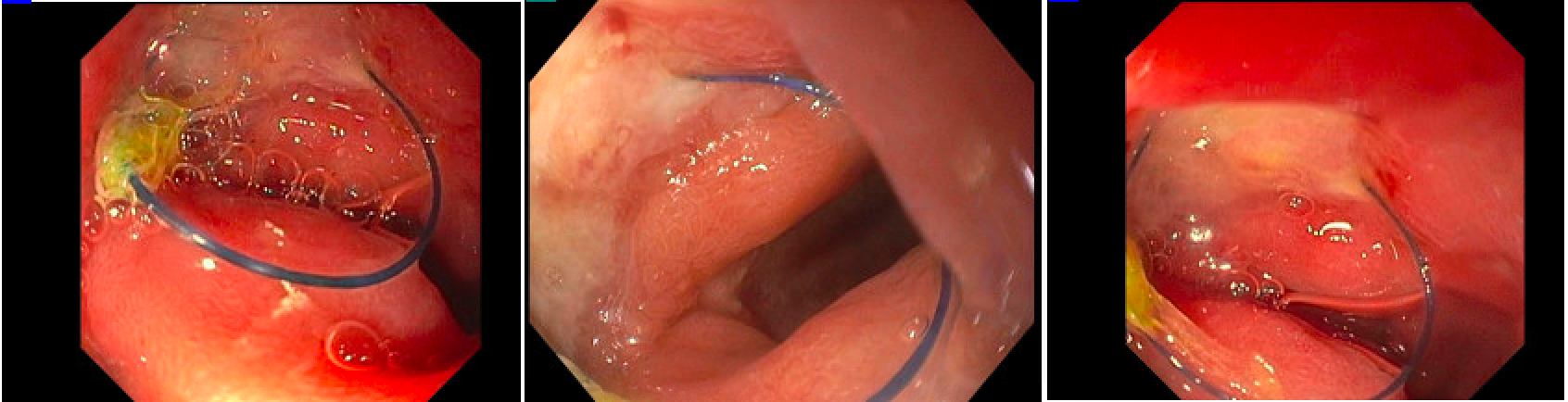
Figure: 1 - Persistent duodenal suture from Graham patch repair

Figure: 2A - Lumen apposing metallic stent (LAMS) placement creating duodenal bypass
2B - Axial CT showing stent placement
Disclosures:
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Shree Laya Vemula indicated no relevant financial relationships.
Sandeep Chikkam indicated no relevant financial relationships.
Pir Shah indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Shree Laya Vemula, MD2, Sandeep Chikkam, MD, DNBSS3, Pir Shah, MD1, Indu Srinivasan, MD1. P5715 - Duodenal-Cutaneous Fistula Closure via LAMS Stent: A Minimally Invasive Solution for Post-Graham Patch Failure, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

