Tuesday Poster Session
Category: Interventional Endoscopy
P5707 - Stent with Helix Tack Fixation for the Treatment of Refractory Gastro-Jejunal Stricture
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- CT
Christopher N. Ton (he/him/his)
Kaiser Permanente
Vacaville, CA
Presenting Author(s)
Christopher N. Ton, 1, Madison Piao, 2, Cindy Piao, MD3, Ashwini Mulgaonkar, MD3, John Erikson Yap, MD, MBA, FACG4, Loc Ton, MD3
1Kaiser Permanente, Vacaville, CA; 2University of California Berkeley, San Diego, CA; 3Kaiser Permanente, Sacramento, CA; 4University of Utah Health, Salt Lake City, UT
Introduction: Gastric anastomotic strictures are a known complication after Roux-en-Y gastric bypass (RYGB) and this incidence is estimated to be around 15%. Patients can present with obstructive symptoms of nausea, vomiting, dysphagia, and weight loss. Refractory gastric anastomotic strictures can prove challenging to treat endoscopically.
Case Description/
Methods: A 72-year-old female with a Roux-en-Y gastric bypass with a revision in 1/2025 for a anastomotic perforation, atrial fibrillation, ischemic stroke (2/2025), dementia, coronary artery disease with STEMI with PCI to LAD (3/2025) admitted for oral intolerance and weight loss. The patient was on apixaban and clopidogrel outpatient due to recent stroke and myocardial infarction with coronary stent placement.
After holding apixaban, an upper endoscopy revealed a high-grade gastro-jejunal anastomotic stricture measuring approximately 4-mm. Balloon dilation was performed to the stricture to 10-mm with improvement in liquid intake . However, shortly at 48 hours she re-developed nausea and intermittent emesis. Total parental nutrition was started on Day 5 due to unmet nutritional goals.
With recurrent dysphagia, the family requested for more aggressive management. Serial upper endoscopies with dilations while the patient was to be on antiplatelet and anticoagulation long term posed a significant dilemma. Off-label use of a fully covered, self-expanding metal esophageal stent to palliate the refractory stricture in this complex scenario was proposed. The option for lumen-apposing metal stents (LAMS) was not available at our institution.
A 18 mm x 97 mm fully covered esophageal stent was placed across the distal esophagus to the gastro-jejunal anastomosis and fixated with a helix tack and endoclip to prevent stent migration. The patient had full tolerance of liquid intake and was able to advance to purees and a soft diet.
Discussion: Gastric anastomotic strictures are common after gastric bypass and minimally invasive therapeutic endoscopic treatments are the preferred first-line therapy over surgery. Refractory gastric anastomotic strictures can be challenging to manage and moreso in a patient requiring anticoagulation and antiplatelet therapy. Options for stent placement (esophageal stent or newer lumen-apposing metal stents) should be evaluated early on in these selected patients. The risk for esophageal stent migration can be as high as one-third of patients but can be mitigated by using different anchoring techniques.
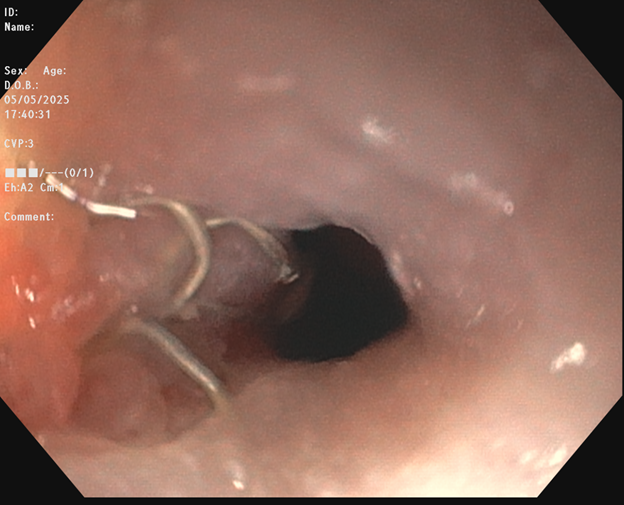
Figure: Severe gastro-jejunal stricture with exposed clips.
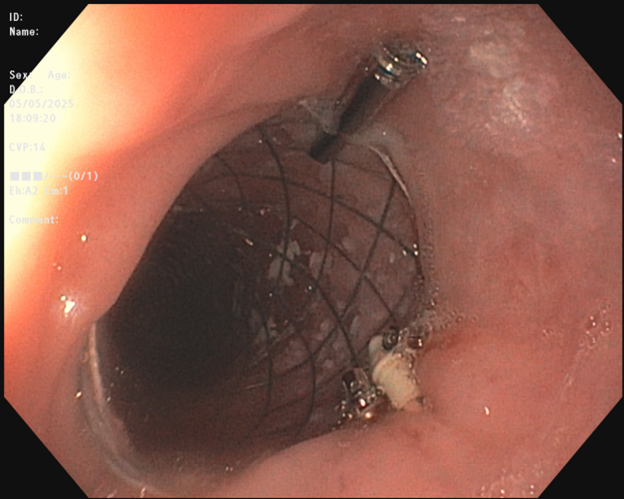
Figure: Stent placement with helix tack and endoclip for treatment of refractory gastro-jejunal stricture
Disclosures:
Christopher Ton indicated no relevant financial relationships.
Madison Piao indicated no relevant financial relationships.
Cindy Piao indicated no relevant financial relationships.
Ashwini Mulgaonkar indicated no relevant financial relationships.
John Erikson Yap: Steris – Consultant.
Loc Ton indicated no relevant financial relationships.
Christopher N. Ton, 1, Madison Piao, 2, Cindy Piao, MD3, Ashwini Mulgaonkar, MD3, John Erikson Yap, MD, MBA, FACG4, Loc Ton, MD3. P5707 - Stent with Helix Tack Fixation for the Treatment of Refractory Gastro-Jejunal Stricture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kaiser Permanente, Vacaville, CA; 2University of California Berkeley, San Diego, CA; 3Kaiser Permanente, Sacramento, CA; 4University of Utah Health, Salt Lake City, UT
Introduction: Gastric anastomotic strictures are a known complication after Roux-en-Y gastric bypass (RYGB) and this incidence is estimated to be around 15%. Patients can present with obstructive symptoms of nausea, vomiting, dysphagia, and weight loss. Refractory gastric anastomotic strictures can prove challenging to treat endoscopically.
Case Description/
Methods: A 72-year-old female with a Roux-en-Y gastric bypass with a revision in 1/2025 for a anastomotic perforation, atrial fibrillation, ischemic stroke (2/2025), dementia, coronary artery disease with STEMI with PCI to LAD (3/2025) admitted for oral intolerance and weight loss. The patient was on apixaban and clopidogrel outpatient due to recent stroke and myocardial infarction with coronary stent placement.
After holding apixaban, an upper endoscopy revealed a high-grade gastro-jejunal anastomotic stricture measuring approximately 4-mm. Balloon dilation was performed to the stricture to 10-mm with improvement in liquid intake . However, shortly at 48 hours she re-developed nausea and intermittent emesis. Total parental nutrition was started on Day 5 due to unmet nutritional goals.
With recurrent dysphagia, the family requested for more aggressive management. Serial upper endoscopies with dilations while the patient was to be on antiplatelet and anticoagulation long term posed a significant dilemma. Off-label use of a fully covered, self-expanding metal esophageal stent to palliate the refractory stricture in this complex scenario was proposed. The option for lumen-apposing metal stents (LAMS) was not available at our institution.
A 18 mm x 97 mm fully covered esophageal stent was placed across the distal esophagus to the gastro-jejunal anastomosis and fixated with a helix tack and endoclip to prevent stent migration. The patient had full tolerance of liquid intake and was able to advance to purees and a soft diet.
Discussion: Gastric anastomotic strictures are common after gastric bypass and minimally invasive therapeutic endoscopic treatments are the preferred first-line therapy over surgery. Refractory gastric anastomotic strictures can be challenging to manage and moreso in a patient requiring anticoagulation and antiplatelet therapy. Options for stent placement (esophageal stent or newer lumen-apposing metal stents) should be evaluated early on in these selected patients. The risk for esophageal stent migration can be as high as one-third of patients but can be mitigated by using different anchoring techniques.
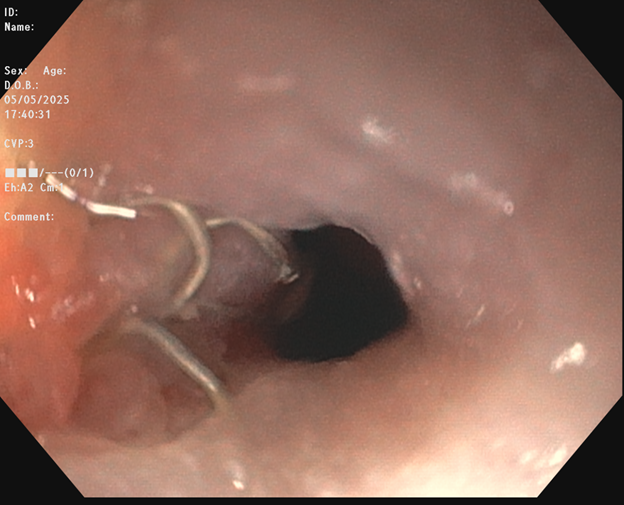
Figure: Severe gastro-jejunal stricture with exposed clips.
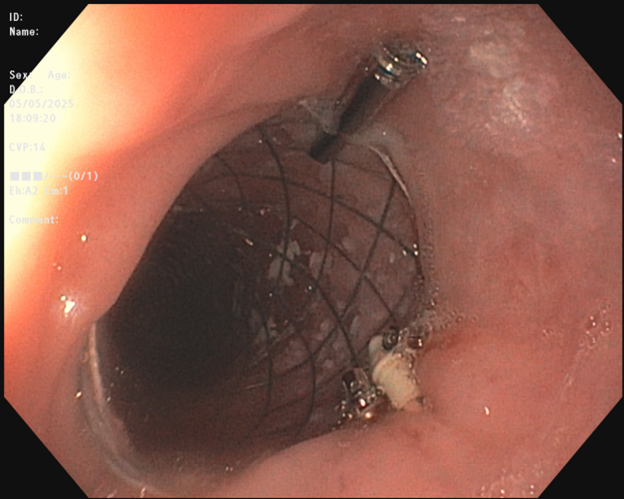
Figure: Stent placement with helix tack and endoclip for treatment of refractory gastro-jejunal stricture
Disclosures:
Christopher Ton indicated no relevant financial relationships.
Madison Piao indicated no relevant financial relationships.
Cindy Piao indicated no relevant financial relationships.
Ashwini Mulgaonkar indicated no relevant financial relationships.
John Erikson Yap: Steris – Consultant.
Loc Ton indicated no relevant financial relationships.
Christopher N. Ton, 1, Madison Piao, 2, Cindy Piao, MD3, Ashwini Mulgaonkar, MD3, John Erikson Yap, MD, MBA, FACG4, Loc Ton, MD3. P5707 - Stent with Helix Tack Fixation for the Treatment of Refractory Gastro-Jejunal Stricture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
