Tuesday Poster Session
Category: Interventional Endoscopy
P5696 - The Impact of Duodenal versus Jejunal Stent Placement for Endoscopic Ultrasound-Guided Gastroenterostomy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chinmay Guralwar, MBBS (he/him/his)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Chinmay Guralwar, MBBS1, Rishad Khan, MD1, Ryan Law, DO1, Jacob Bauss, MD1, Andrew Storm, MD1, Eric J.. Vargas, MD, MS1, Samuel Han, MD1, Jad AbiMansour, MD1, Barham Abu Dayyeh, MD, MPH2, Vinay Chandrasekhara, MD1
1Mayo Clinic, Rochester, MN; 2Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) with lumen apposing metal stents (LAMS) is a safe and effective option for the palliation of gastric outlet obstruction (GOO). While the endoscopic procedure was initially intended to replicate surgical gastrojejunostomy (EUS-GJ), it became apparent that the distal duodenum may be a suitable target for endoscopic anastomosis (EUS-GD). As EUS-GD represents a physiologically different approach from surgical GJ, the hypothesis of this study is that EUS-GD is similar to EUS-GJ with respect to clinical outcomes, adverse events (AEs), and reintervention rates.
Methods: Patients who underwent EUS-GE for management of GOO between January 2020 and June 2023 were identified from a procedural database at a large referral center. Cases were categorized as having duodenal or jejunal placement of a LAMS during EUS-GE through review of post-procedural cross-sectional imaging. Baseline demographics, clinical variables, and outcomes data were collected. All stents were 15mm (diameter) x 10mm (length) in size. The primary outcome was clinical success, defined as the ability to tolerate a diet following EUS-GE. Secondary outcomes were immediate (bleeding, perforation, and death) and delayed (stent obstruction, stent migration) AEs. Continuous and categorical variables were compared using the unpaired t-test and Fisher’s exact test, respectively, with statistical significance at p< 0.05.
Results: One hundred and thirty-nine patients were included. Eighty-seven (63%) underwent EUS-GJ and 52 (37%) underwent EUS-GD. There were no significant baseline differences between groups (Table 1). There was no significant difference between groups for the primary outcome of clinical success (EUS-GD 98% vs EUS-GJ 97%, odds ratio [OR] 1.20, 95% CI 0.1-13.6, p >0.99) and secondary outcomes of bleeding (4% vs. 2%, OR 1.70, 95% CI 0.23-12.4, p=0.63), death (2% vs 1%, OR 1.69, 95% CI 0.1-27.5, p >0.99), perforation (6% vs. 1%, OR 0.54, 95% CI 0.06 – 5.4, p=0.15), and stent obstruction (6% vs. 14%, OR 0.38, 95% CI 0.1-1.4, p=0.17) (Table 1).
Discussion: Clinical success rates overall were excellent, with EUS-GD having comparable outcomes as EUS-GJ. Endoscopists should consider these data alongside other factors, such as the technical feasibility of targeting different bowel loops and the anticipated need for future biliary intervention, when performing EUS-GE.
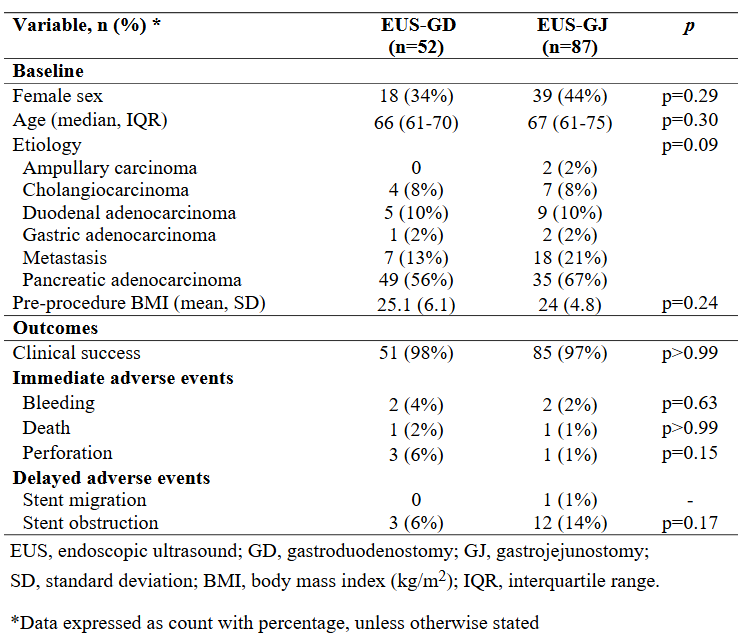
Figure: Table: Baseline demographics, clinical variables, and outcomes for endoscopic ultrasound-guided gastroduodenostomy compared to gastrojejunostomy.
Disclosures:
Chinmay Guralwar indicated no relevant financial relationships.
Rishad Khan indicated no relevant financial relationships.
Ryan Law: Boston Scientific – Consultant, Grant/Research Support. Neptune Medical – Data safety monitoring board. Olympus America – Consultant, Grant/Research Support. UpToDate – Royalties.
Jacob Bauss indicated no relevant financial relationships.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Consultant, Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-Tagss – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Microtech – Consultant. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support. Sotelix – Consultant. Steris – Consultant.
Eric Vargas indicated no relevant financial relationships.
Samuel Han: Boston Scientific – Consultant.
Jad AbiMansour: Ruhof Inc. – Royalties.
Barham Abu Dayyeh indicated no relevant financial relationships.
Vinay Chandrasekhara indicated no relevant financial relationships.
Chinmay Guralwar, MBBS1, Rishad Khan, MD1, Ryan Law, DO1, Jacob Bauss, MD1, Andrew Storm, MD1, Eric J.. Vargas, MD, MS1, Samuel Han, MD1, Jad AbiMansour, MD1, Barham Abu Dayyeh, MD, MPH2, Vinay Chandrasekhara, MD1. P5696 - The Impact of Duodenal versus Jejunal Stent Placement for Endoscopic Ultrasound-Guided Gastroenterostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) with lumen apposing metal stents (LAMS) is a safe and effective option for the palliation of gastric outlet obstruction (GOO). While the endoscopic procedure was initially intended to replicate surgical gastrojejunostomy (EUS-GJ), it became apparent that the distal duodenum may be a suitable target for endoscopic anastomosis (EUS-GD). As EUS-GD represents a physiologically different approach from surgical GJ, the hypothesis of this study is that EUS-GD is similar to EUS-GJ with respect to clinical outcomes, adverse events (AEs), and reintervention rates.
Methods: Patients who underwent EUS-GE for management of GOO between January 2020 and June 2023 were identified from a procedural database at a large referral center. Cases were categorized as having duodenal or jejunal placement of a LAMS during EUS-GE through review of post-procedural cross-sectional imaging. Baseline demographics, clinical variables, and outcomes data were collected. All stents were 15mm (diameter) x 10mm (length) in size. The primary outcome was clinical success, defined as the ability to tolerate a diet following EUS-GE. Secondary outcomes were immediate (bleeding, perforation, and death) and delayed (stent obstruction, stent migration) AEs. Continuous and categorical variables were compared using the unpaired t-test and Fisher’s exact test, respectively, with statistical significance at p< 0.05.
Results: One hundred and thirty-nine patients were included. Eighty-seven (63%) underwent EUS-GJ and 52 (37%) underwent EUS-GD. There were no significant baseline differences between groups (Table 1). There was no significant difference between groups for the primary outcome of clinical success (EUS-GD 98% vs EUS-GJ 97%, odds ratio [OR] 1.20, 95% CI 0.1-13.6, p >0.99) and secondary outcomes of bleeding (4% vs. 2%, OR 1.70, 95% CI 0.23-12.4, p=0.63), death (2% vs 1%, OR 1.69, 95% CI 0.1-27.5, p >0.99), perforation (6% vs. 1%, OR 0.54, 95% CI 0.06 – 5.4, p=0.15), and stent obstruction (6% vs. 14%, OR 0.38, 95% CI 0.1-1.4, p=0.17) (Table 1).
Discussion: Clinical success rates overall were excellent, with EUS-GD having comparable outcomes as EUS-GJ. Endoscopists should consider these data alongside other factors, such as the technical feasibility of targeting different bowel loops and the anticipated need for future biliary intervention, when performing EUS-GE.
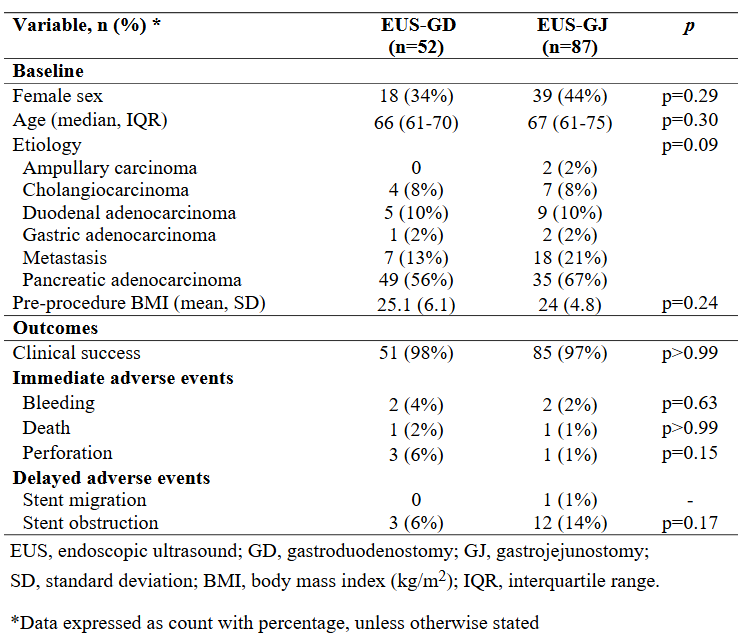
Figure: Table: Baseline demographics, clinical variables, and outcomes for endoscopic ultrasound-guided gastroduodenostomy compared to gastrojejunostomy.
Disclosures:
Chinmay Guralwar indicated no relevant financial relationships.
Rishad Khan indicated no relevant financial relationships.
Ryan Law: Boston Scientific – Consultant, Grant/Research Support. Neptune Medical – Data safety monitoring board. Olympus America – Consultant, Grant/Research Support. UpToDate – Royalties.
Jacob Bauss indicated no relevant financial relationships.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Consultant, Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-Tagss – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Microtech – Consultant. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support. Sotelix – Consultant. Steris – Consultant.
Eric Vargas indicated no relevant financial relationships.
Samuel Han: Boston Scientific – Consultant.
Jad AbiMansour: Ruhof Inc. – Royalties.
Barham Abu Dayyeh indicated no relevant financial relationships.
Vinay Chandrasekhara indicated no relevant financial relationships.
Chinmay Guralwar, MBBS1, Rishad Khan, MD1, Ryan Law, DO1, Jacob Bauss, MD1, Andrew Storm, MD1, Eric J.. Vargas, MD, MS1, Samuel Han, MD1, Jad AbiMansour, MD1, Barham Abu Dayyeh, MD, MPH2, Vinay Chandrasekhara, MD1. P5696 - The Impact of Duodenal versus Jejunal Stent Placement for Endoscopic Ultrasound-Guided Gastroenterostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
