Tuesday Poster Session
Category: Interventional Endoscopy
P5694 - Novel Argon Plasma Coagulation Resurfacing for Management of Recalcitrant Marginal Ulceration
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yara Salameh, MD
Mayo Foundation for Medical Education and Research
Rochester, MN
Presenting Author(s)
Yara Salameh, MD1, Hadi Khaled. Abou Zeid, MD2, Jad AbiMansour, MD2, Andrew Storm, MD2
1Mayo Foundation for Medical Education and Research, Rochester, MN; 2Mayo Clinic, Rochester, MN
Introduction: Marginal ulcers (MUs) may occur after Roux-en-Y gastric bypass (RYGB) and may be recurring or resistant to medical treatment. Endoscopic repair with sutures or clips may be attempted prior to considering revisional surgery. We hypothesized that adjuvant argon plasma coagulation (APC) resurfacing of the ulcer bed and adjacent mucosa followed by overstitch repair could improve healing rates.
Methods: We conducted a retrospective chart review of adult patients with a history of RYGB undergoing APC for recurrent or recalcitrant MUs. Ulcers were recurrent if previously healed and reappeared, or recalcitrant if unresponsive to an intensive eight-week proton pump inhibitor course. Healing was evaluated by follow-up endoscopy or symptom resolution four weeks post-procedure.
Results: Thirteen patients (11 females 78.6%; median age 46 years, IQR 40–56) with MU were included. Median time since RYGB was 21 months (IQR 11–48). Conventional risk factors were absent: all were negative for Helicobacter pylori, none smoked, and one intermittently used NSAIDs. All ulcers had undergone previous unsuccessful treatments, up to 5 interventions per ulcer, including endoscopic suturing without APC, intensive medical therapy, and surgical staple removal. Median pouch size was 5 cm (IQR 4–7). Forrest class III ulcers were most common (n=10, 76.9%), followed by class IIa (n=2, 15.4%) and IIc (n=1, 7.7%). Ulcer beds were resurfaced using APC (flow: 0.8 L/min in 6 cases, 1.0 L/min in 7 cases; power: 15–35 W), followed by sutured repair in all cases. Two patients experienced transient post-procedural abdominal pain. Complete healing occurred in 7 patients after a single intervention, and in one additional patient after a second session, yielding a total success rate of 61.5%. Healing primarily occurred in ulcers without prior endoscopic manipulation, while all five treatment failures involved previously manipulated, deep ulcers.
Discussion: In this pilot study, adjuvant APC resurfacing before sutured repair of MUs appears safe and may enhance ulcer healing, potentially avoiding revisional surgery. The technique was most beneficial in treatment-naïve or minimally manipulated ulcers, highlighting the importance of ulcer chronicity and mucosal integrity. Further studies are warranted to refine patient selection and confirm ideal technical aspects of this new technique.
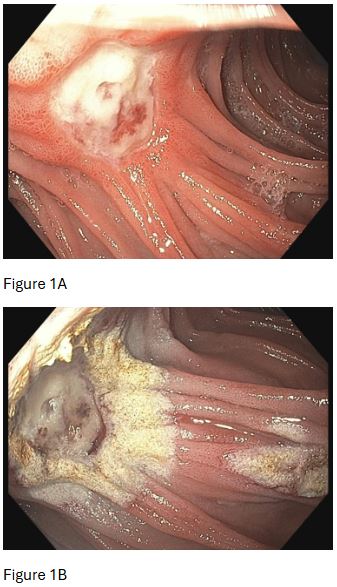
Figure: Figure 1A: Deep Forrest Class 3 ulcer at the GJ anastomosis
Figure 1B: Marginal ulcer after treatment with APC (1L/min, 35W)
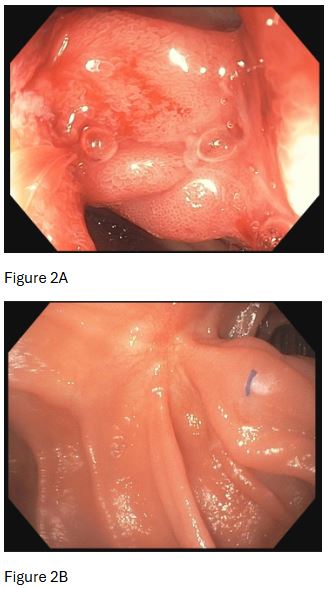
Figure: Figure 2A: APC treated ulcer bed sutured in a running fashion using Overstitch
Figure 2B: Fusion at site of repair, excellent resolution of ulcer three months post-procedure
Disclosures:
Yara Salameh indicated no relevant financial relationships.
Hadi Abou Zeid indicated no relevant financial relationships.
Jad AbiMansour: Ruhof Inc. – Royalties.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Grant/Research Support. Boston Scientific – Consultant. Boston Scientific – Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-TAGSS – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support.
Yara Salameh, MD1, Hadi Khaled. Abou Zeid, MD2, Jad AbiMansour, MD2, Andrew Storm, MD2. P5694 - Novel Argon Plasma Coagulation Resurfacing for Management of Recalcitrant Marginal Ulceration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Foundation for Medical Education and Research, Rochester, MN; 2Mayo Clinic, Rochester, MN
Introduction: Marginal ulcers (MUs) may occur after Roux-en-Y gastric bypass (RYGB) and may be recurring or resistant to medical treatment. Endoscopic repair with sutures or clips may be attempted prior to considering revisional surgery. We hypothesized that adjuvant argon plasma coagulation (APC) resurfacing of the ulcer bed and adjacent mucosa followed by overstitch repair could improve healing rates.
Methods: We conducted a retrospective chart review of adult patients with a history of RYGB undergoing APC for recurrent or recalcitrant MUs. Ulcers were recurrent if previously healed and reappeared, or recalcitrant if unresponsive to an intensive eight-week proton pump inhibitor course. Healing was evaluated by follow-up endoscopy or symptom resolution four weeks post-procedure.
Results: Thirteen patients (11 females 78.6%; median age 46 years, IQR 40–56) with MU were included. Median time since RYGB was 21 months (IQR 11–48). Conventional risk factors were absent: all were negative for Helicobacter pylori, none smoked, and one intermittently used NSAIDs. All ulcers had undergone previous unsuccessful treatments, up to 5 interventions per ulcer, including endoscopic suturing without APC, intensive medical therapy, and surgical staple removal. Median pouch size was 5 cm (IQR 4–7). Forrest class III ulcers were most common (n=10, 76.9%), followed by class IIa (n=2, 15.4%) and IIc (n=1, 7.7%). Ulcer beds were resurfaced using APC (flow: 0.8 L/min in 6 cases, 1.0 L/min in 7 cases; power: 15–35 W), followed by sutured repair in all cases. Two patients experienced transient post-procedural abdominal pain. Complete healing occurred in 7 patients after a single intervention, and in one additional patient after a second session, yielding a total success rate of 61.5%. Healing primarily occurred in ulcers without prior endoscopic manipulation, while all five treatment failures involved previously manipulated, deep ulcers.
Discussion: In this pilot study, adjuvant APC resurfacing before sutured repair of MUs appears safe and may enhance ulcer healing, potentially avoiding revisional surgery. The technique was most beneficial in treatment-naïve or minimally manipulated ulcers, highlighting the importance of ulcer chronicity and mucosal integrity. Further studies are warranted to refine patient selection and confirm ideal technical aspects of this new technique.
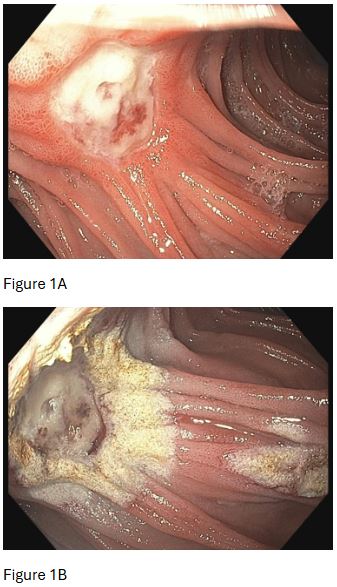
Figure: Figure 1A: Deep Forrest Class 3 ulcer at the GJ anastomosis
Figure 1B: Marginal ulcer after treatment with APC (1L/min, 35W)
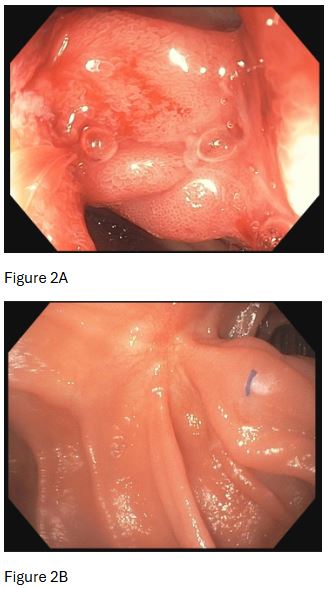
Figure: Figure 2A: APC treated ulcer bed sutured in a running fashion using Overstitch
Figure 2B: Fusion at site of repair, excellent resolution of ulcer three months post-procedure
Disclosures:
Yara Salameh indicated no relevant financial relationships.
Hadi Abou Zeid indicated no relevant financial relationships.
Jad AbiMansour: Ruhof Inc. – Royalties.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Grant/Research Support. Boston Scientific – Consultant. Boston Scientific – Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-TAGSS – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support.
Yara Salameh, MD1, Hadi Khaled. Abou Zeid, MD2, Jad AbiMansour, MD2, Andrew Storm, MD2. P5694 - Novel Argon Plasma Coagulation Resurfacing for Management of Recalcitrant Marginal Ulceration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

