Tuesday Poster Session
Category: Interventional Endoscopy
P5691 - Prevalence, Predictors, and Outcomes of Post-POEM GERD in Achalasia: Endoscopic and Quality-of-Life Assessment
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Omar Shamaa, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Omar Shamaa, MD1, Jonathan A. Montrose, DO1, Ammad Javaid. Chaudhary, MD1, Maria Chavarria-Viales, 1, Razan Aburumman, MD1, Agustin Gavidia Rosario, MD1, Ali Kadouh, MD1, Ammaar Abbasi, MD1, Faisal Nimri, MD2, Brian Ginnebaugh, MD1, Eva Alsheik, MD1, Tobias Zuchelli, 2, Cyrus Piraka, MD1
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Peroral endoscopic myotomy (POEM) is an increasingly utilized treatment for achalasia. While effective in relieving dysphagia, POEM carries a risk of gastroesophageal reflux disease (GERD), though the true incidence and severity of post-POEM GERD remain unclear. This study aims to evaluate GERD following POEM, including its prevalence, long-term complications and impact on quality of life.
Methods: This single-center retrospective study analyzed achalasia patients who underwent POEM between 10/2017 and 3/2025. Baseline data included Eckardt scores, upper endoscopy (EGD), EndoFLIP, and high-resolution manometry findings. Post-procedure GERD was assessed via EGD, and its subjective impact was evaluated using GERD Health-Related Quality of Life (GERD-HRQL) questionnaire (score range: 0–75); a higher score denotes worse symptoms.
Results: A total of 152 patients were included, with a mean baseline Eckardt score of 7.37 (mean follow up, 15.2 months). Posterior tunnel location (70%) and circular myotomies (65%) were most frequently performed, with an average myotomy length of 101 mm. Mean post-procedure Eckardt score was 1.17. Younger patients with more severe baseline symptoms had greater symptom improvement. Post-POEM GERD was identified on initial EGD in 7.2%(n=11) of patients. Subsequent follow up EGDs noted evidence of GERD in 3.3% (n=5), two of whom had identified GERD on index post-POEM EGD with progression of esophagitis and new peptic stricture formation. GERD incidence was associated with older age, higher baseline Eckardt scores, higher baseline EGJ-DI, and longer myotomy lengths. Among the 47 patients who completed the GERD-HRQL, the average score was 14.4. Overall, 77% of patients reported satisfaction with their reflux symptoms, while 13% were dissatisfied and 10% were neutral. Higher GERD-HRQL scores were observed in younger patients and those with full-thickness myotomies; this group also had more frequent clinic visits and follow-up EGDs. Only three cases required subsequent fundoplication, all with achalasia type III and lower baseline IRP values. No correlation was found between achalasia subtype and GERD incidence.
Discussion: POEM is an effective intervention with low rates of post-procedure GERD, as well as minimal reflux-related complications and symptom burden. However, several factors were found to increase the risk of post-POEM GERD, emphasizing the importance of personalized procedural planning and close follow up in high-risk patients.
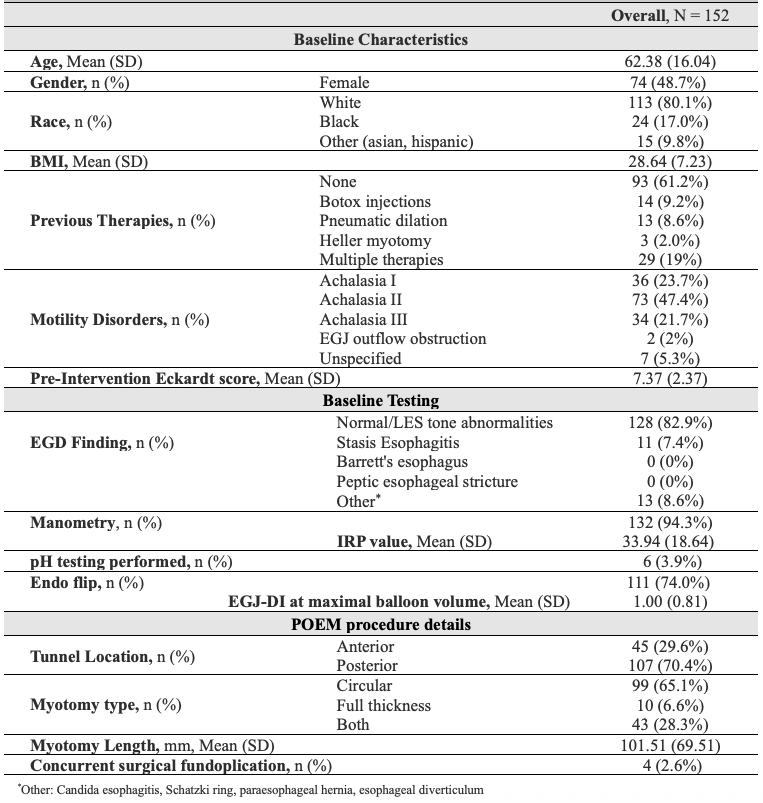
Figure: Table 1. Patient baseline characteristics, baseline testing & intraprocedural details
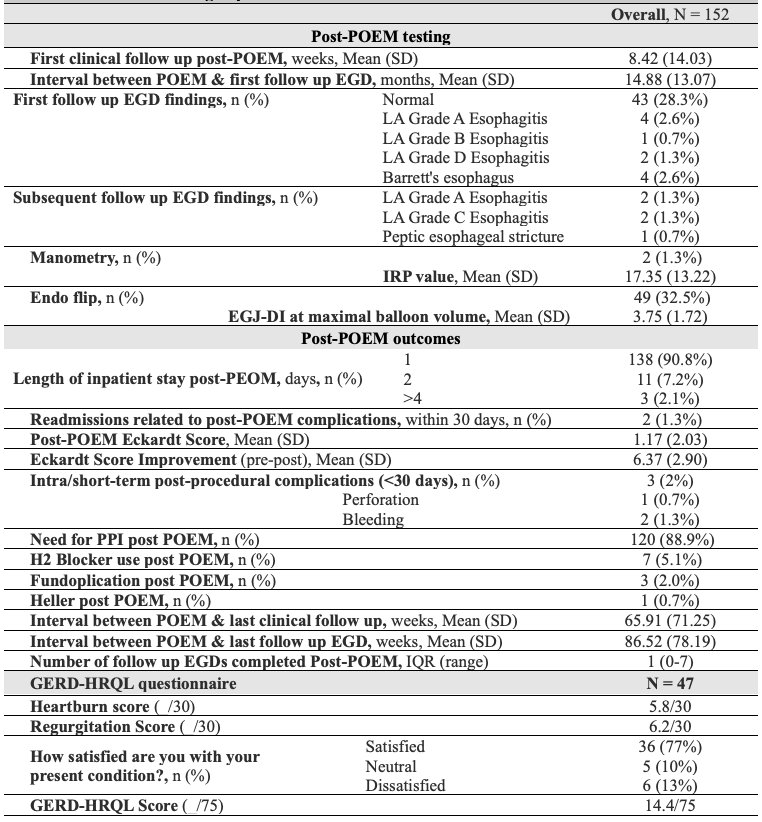
Figure: Table 2. Post-POEM testing & patient outcomes
Disclosures:
Omar Shamaa indicated no relevant financial relationships.
Jonathan Montrose indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Maria Chavarria-Viales indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Ali Kadouh indicated no relevant financial relationships.
Ammaar Abbasi indicated no relevant financial relationships.
Faisal Nimri indicated no relevant financial relationships.
Brian Ginnebaugh: Ardelyx – Speakers Bureau.
Eva Alsheik indicated no relevant financial relationships.
Tobias Zuchelli: Boston Scientific – Consultant.
Cyrus Piraka indicated no relevant financial relationships.
Omar Shamaa, MD1, Jonathan A. Montrose, DO1, Ammad Javaid. Chaudhary, MD1, Maria Chavarria-Viales, 1, Razan Aburumman, MD1, Agustin Gavidia Rosario, MD1, Ali Kadouh, MD1, Ammaar Abbasi, MD1, Faisal Nimri, MD2, Brian Ginnebaugh, MD1, Eva Alsheik, MD1, Tobias Zuchelli, 2, Cyrus Piraka, MD1. P5691 - Prevalence, Predictors, and Outcomes of Post-POEM GERD in Achalasia: Endoscopic and Quality-of-Life Assessment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI
Introduction: Peroral endoscopic myotomy (POEM) is an increasingly utilized treatment for achalasia. While effective in relieving dysphagia, POEM carries a risk of gastroesophageal reflux disease (GERD), though the true incidence and severity of post-POEM GERD remain unclear. This study aims to evaluate GERD following POEM, including its prevalence, long-term complications and impact on quality of life.
Methods: This single-center retrospective study analyzed achalasia patients who underwent POEM between 10/2017 and 3/2025. Baseline data included Eckardt scores, upper endoscopy (EGD), EndoFLIP, and high-resolution manometry findings. Post-procedure GERD was assessed via EGD, and its subjective impact was evaluated using GERD Health-Related Quality of Life (GERD-HRQL) questionnaire (score range: 0–75); a higher score denotes worse symptoms.
Results: A total of 152 patients were included, with a mean baseline Eckardt score of 7.37 (mean follow up, 15.2 months). Posterior tunnel location (70%) and circular myotomies (65%) were most frequently performed, with an average myotomy length of 101 mm. Mean post-procedure Eckardt score was 1.17. Younger patients with more severe baseline symptoms had greater symptom improvement. Post-POEM GERD was identified on initial EGD in 7.2%(n=11) of patients. Subsequent follow up EGDs noted evidence of GERD in 3.3% (n=5), two of whom had identified GERD on index post-POEM EGD with progression of esophagitis and new peptic stricture formation. GERD incidence was associated with older age, higher baseline Eckardt scores, higher baseline EGJ-DI, and longer myotomy lengths. Among the 47 patients who completed the GERD-HRQL, the average score was 14.4. Overall, 77% of patients reported satisfaction with their reflux symptoms, while 13% were dissatisfied and 10% were neutral. Higher GERD-HRQL scores were observed in younger patients and those with full-thickness myotomies; this group also had more frequent clinic visits and follow-up EGDs. Only three cases required subsequent fundoplication, all with achalasia type III and lower baseline IRP values. No correlation was found between achalasia subtype and GERD incidence.
Discussion: POEM is an effective intervention with low rates of post-procedure GERD, as well as minimal reflux-related complications and symptom burden. However, several factors were found to increase the risk of post-POEM GERD, emphasizing the importance of personalized procedural planning and close follow up in high-risk patients.
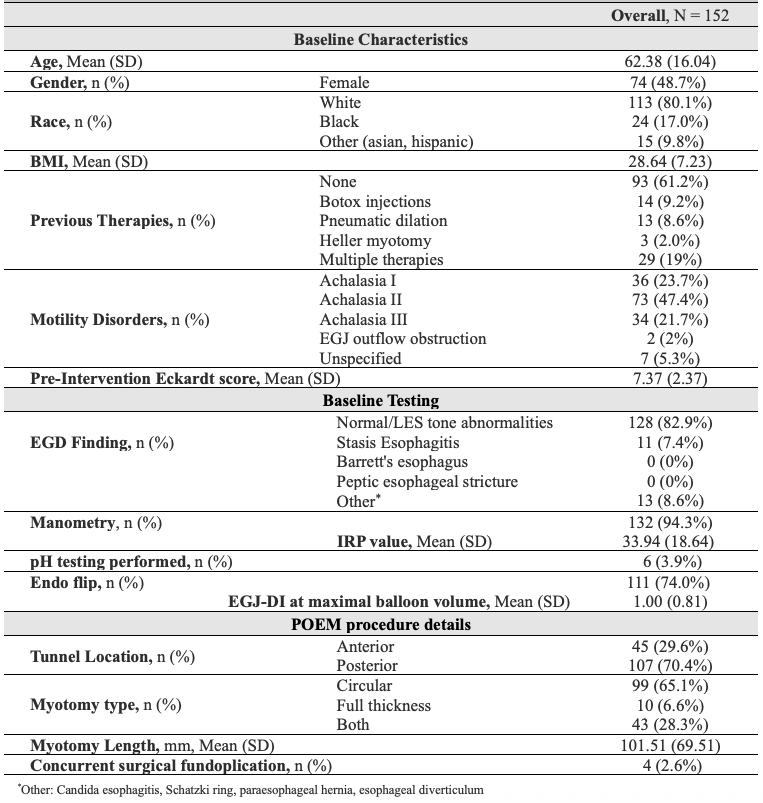
Figure: Table 1. Patient baseline characteristics, baseline testing & intraprocedural details
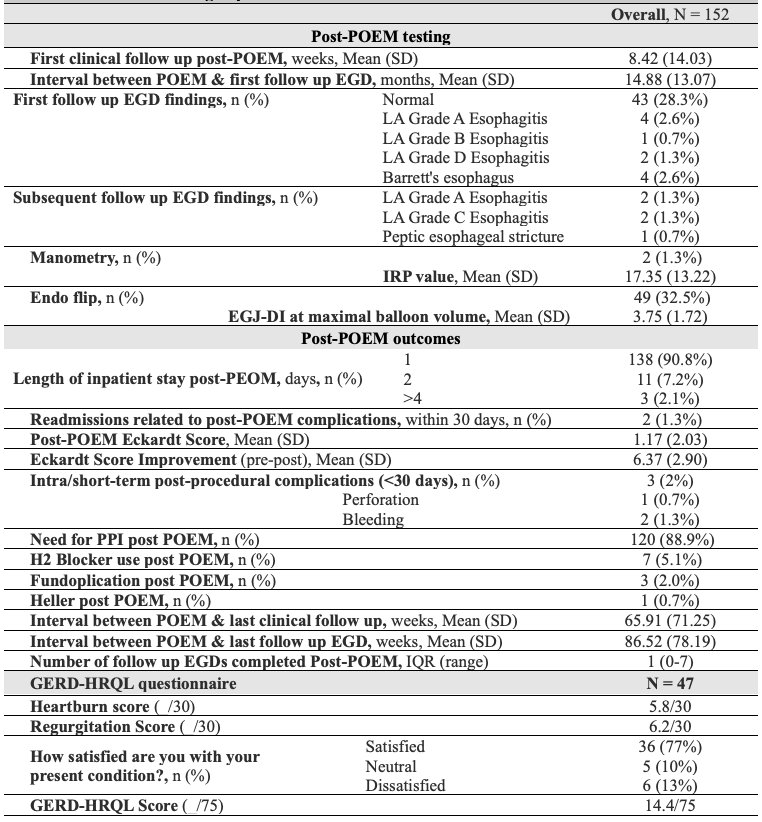
Figure: Table 2. Post-POEM testing & patient outcomes
Disclosures:
Omar Shamaa indicated no relevant financial relationships.
Jonathan Montrose indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Maria Chavarria-Viales indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Ali Kadouh indicated no relevant financial relationships.
Ammaar Abbasi indicated no relevant financial relationships.
Faisal Nimri indicated no relevant financial relationships.
Brian Ginnebaugh: Ardelyx – Speakers Bureau.
Eva Alsheik indicated no relevant financial relationships.
Tobias Zuchelli: Boston Scientific – Consultant.
Cyrus Piraka indicated no relevant financial relationships.
Omar Shamaa, MD1, Jonathan A. Montrose, DO1, Ammad Javaid. Chaudhary, MD1, Maria Chavarria-Viales, 1, Razan Aburumman, MD1, Agustin Gavidia Rosario, MD1, Ali Kadouh, MD1, Ammaar Abbasi, MD1, Faisal Nimri, MD2, Brian Ginnebaugh, MD1, Eva Alsheik, MD1, Tobias Zuchelli, 2, Cyrus Piraka, MD1. P5691 - Prevalence, Predictors, and Outcomes of Post-POEM GERD in Achalasia: Endoscopic and Quality-of-Life Assessment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
