Tuesday Poster Session
Category: Interventional Endoscopy
P5687 - Transforming Cardiovascular Risk Through Endoscopic Sleeve Gastroplasty: 1-Year Outcomes in a Real-World Population
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- WG
Wissam Ghusn, MD
Boston Medical Center
Boston, MA
Presenting Author(s)
Wissam Ghusn, MD1, Yara Salameh, MD2, Maria Antonia Espinosa, MD3, Jose Villamarin, MD3, Karim Al Annan, MD4, Lea Sayegh, MD5, Serena J. Rahme, MD3, Kamal Abi Mosleh, MD3, Johnny Bou Saba, MD6, Khushboo Gala, MBBS3, Eric J.. Vargas, MD, MS3, Andrew Storm, MD3
1Boston Medical Center, Boston, MA; 2Mayo Foundation for Medical Education and Research, Rochester, MN; 3Mayo Clinic, Rochester, MN; 4University of Connecticut Health Center, Hartford, CT; 5Yale New Haven Hospital, New Haven, CT; 6St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Endoscopic sleeve gastroplasty (ESG) is a novel, minimally invasive endoscopic bariatric procedure that induces significant weight loss and metabolic improvement by reducing gastric volume and delaying gastric emptying. While ESG has shown promise in prospective clinical trials, its impact on long-term cardiovascular risk, particularly atherosclerotic cardiovascular disease (ASCVD) risk has not been well characterized in real-world populations. This study evaluates 1-year changes in weight, lipid profiles, blood pressure, and both 10-year and lifetime ASCVD risk following ESG in a real-world cohort at a tertiary academic center.
Methods: We conducted a retrospective cohort study of adult patients with obesity who underwent ESG between 2013 and 2022. Inclusion criteria were age ≥18 years, available pre-procedure and 1-year follow-up data, and absence of prior metabolic or bariatric surgery. Clinical parameters were collected including age, sex, race, weight, height, BMI, blood pressure, and lipid profiles. The primary outcomes were changes in 10-year and lifetime ASCVD risk scores, calculated using the ACC/AHA pooled cohort equations. Secondary outcomes included total body weight loss percentage (TBWL%) and changes in systolic and diastolic blood pressure, total cholesterol, LDL-C, and HDL-C. Matched paired t-tests were used for comparisons of pre- and post-ESG values.
Results: Out of 183 patients, a total of 33 patients with pre- and post-ESG data were included in the analysis (mean age 49.6 ± 11.1 years; 84.9% female; 93.9% White). Baseline demographics and clinical data are presented in Table 1. At 1-year post-ESG, 10-year ASCVD risk dropped from 1.8% to 1.1% (mean change −0.7%, p< 0.01; Figure 1A), while lifetime ASCVD risk decreased from 37.3% to 32.9% (mean change −4.4%, p=0.09; Figure 1B). Patients experienced significant TBWL% (−12.9 ± 2.2%, p< 0.01; Figure 1C). Lipid changes were not statistically significant: LDL-C (−2.3 mg/dL, p=0.58; Figure 1D), total cholesterol (−6.3 mg/dL, p=0.19; Figure 1E), and HDL-C (+2.7 mg/dL, p=0.07 Figure 1F). Systolic blood pressure declined by −6.9 mmHg (p=0.006; Figure 1G), while changes in diastolic pressure were modest and non-significant (−1.9 mmHg, p=0.36; Figure 1H).
Discussion: In this clinical cohort, ESG was associated with significant weight loss and clinically meaningful improvements in 10-year ASCVD risk. Further prospective and comparative studies with larger cohort size are warranted to validate these findings.
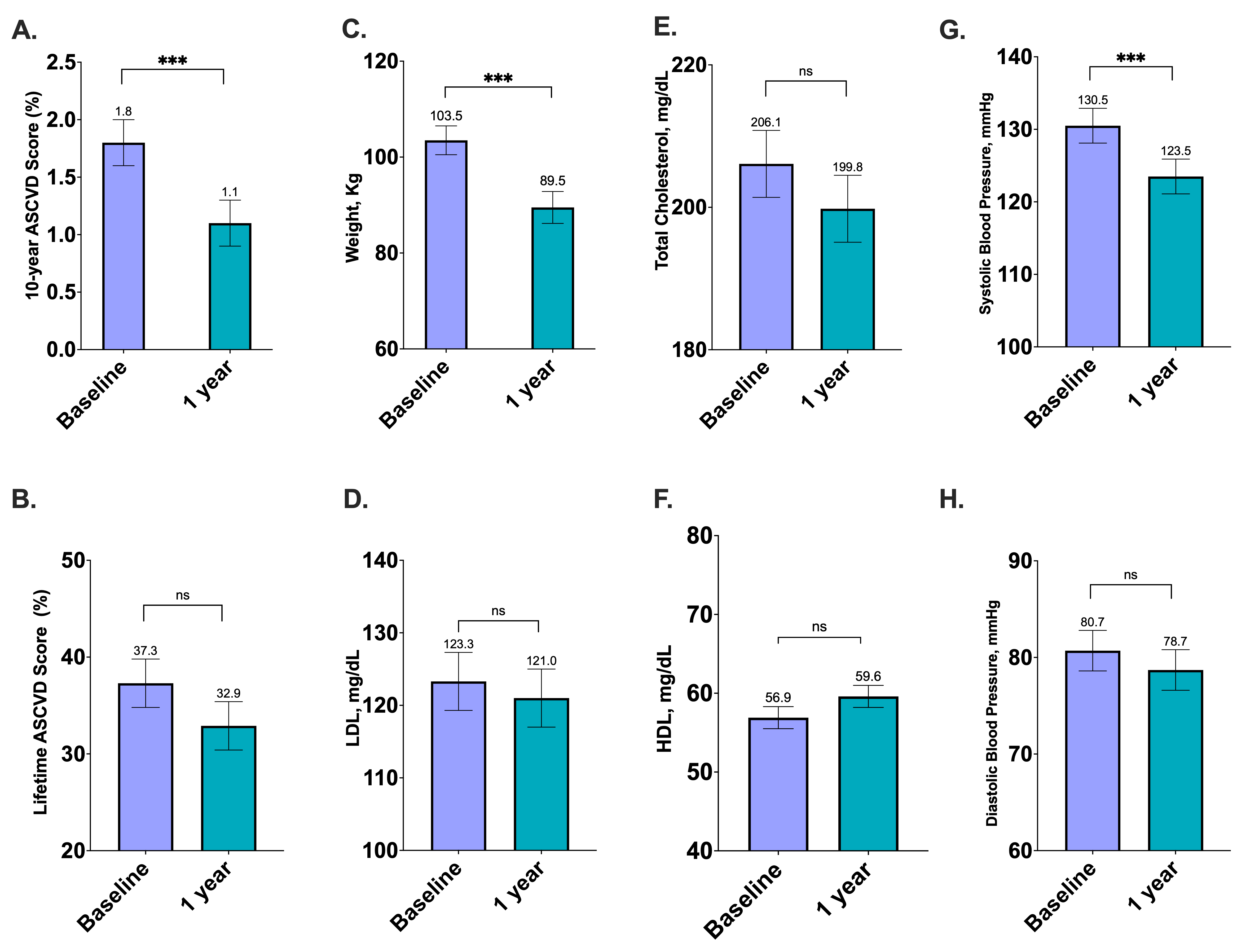
Figure: Table 1: Baseline Demographic and Cardiometabolic Characteristics of Patients Undergoing Endoscopic Sleeve Gastroplasty.
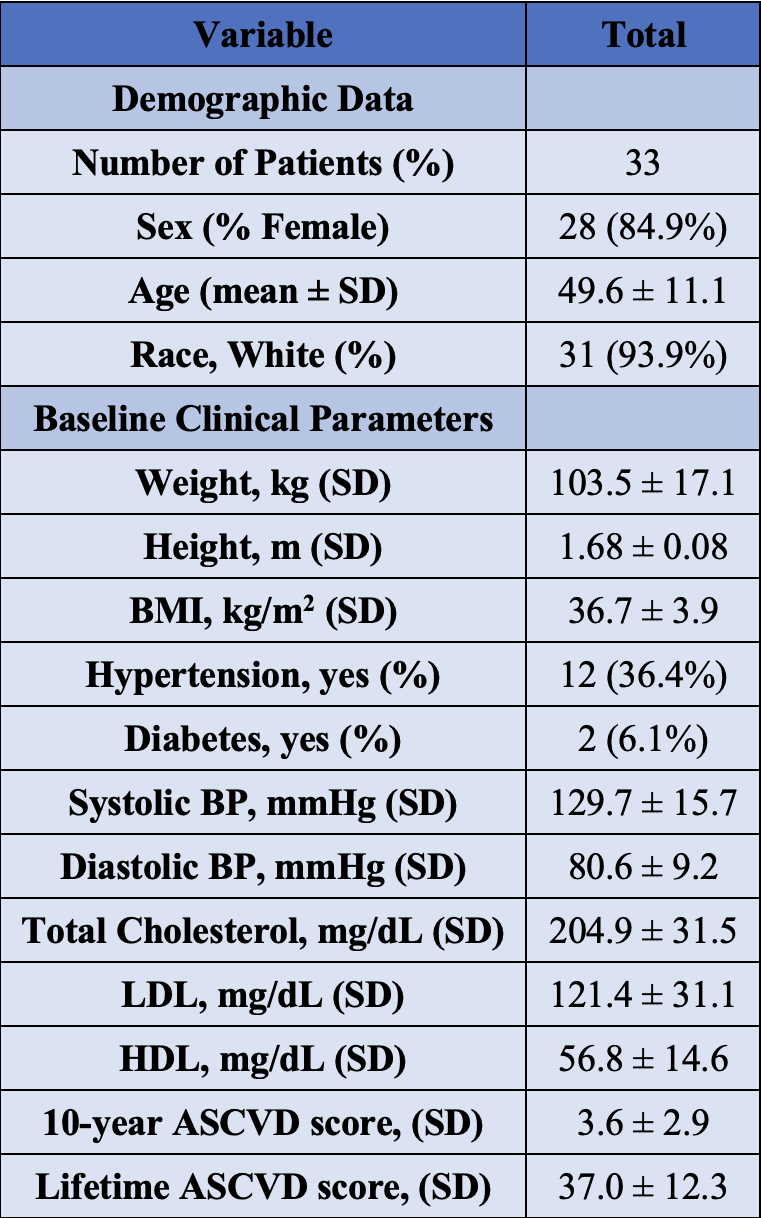
Figure: Figure 1: One-Year Changes in Cardiometabolic Risk Markers Following Endoscopic Sleeve Gastroplasty. (***: p<0.01; ns: Non-significant)
Disclosures:
Wissam Ghusn indicated no relevant financial relationships.
Yara Salameh indicated no relevant financial relationships.
Maria Antonia Espinosa indicated no relevant financial relationships.
Jose Villamarin indicated no relevant financial relationships.
Karim Al Annan indicated no relevant financial relationships.
Lea Sayegh indicated no relevant financial relationships.
Serena J. Rahme indicated no relevant financial relationships.
Kamal Abi Mosleh indicated no relevant financial relationships.
Johnny Bou Saba indicated no relevant financial relationships.
Khushboo Gala indicated no relevant financial relationships.
Eric Vargas indicated no relevant financial relationships.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Consultant, Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-Tagss – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Microtech – Consultant. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support. Sotelix – Consultant. Steris – Consultant.
Wissam Ghusn, MD1, Yara Salameh, MD2, Maria Antonia Espinosa, MD3, Jose Villamarin, MD3, Karim Al Annan, MD4, Lea Sayegh, MD5, Serena J. Rahme, MD3, Kamal Abi Mosleh, MD3, Johnny Bou Saba, MD6, Khushboo Gala, MBBS3, Eric J.. Vargas, MD, MS3, Andrew Storm, MD3. P5687 - Transforming Cardiovascular Risk Through Endoscopic Sleeve Gastroplasty: 1-Year Outcomes in a Real-World Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Boston Medical Center, Boston, MA; 2Mayo Foundation for Medical Education and Research, Rochester, MN; 3Mayo Clinic, Rochester, MN; 4University of Connecticut Health Center, Hartford, CT; 5Yale New Haven Hospital, New Haven, CT; 6St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA
Introduction: Endoscopic sleeve gastroplasty (ESG) is a novel, minimally invasive endoscopic bariatric procedure that induces significant weight loss and metabolic improvement by reducing gastric volume and delaying gastric emptying. While ESG has shown promise in prospective clinical trials, its impact on long-term cardiovascular risk, particularly atherosclerotic cardiovascular disease (ASCVD) risk has not been well characterized in real-world populations. This study evaluates 1-year changes in weight, lipid profiles, blood pressure, and both 10-year and lifetime ASCVD risk following ESG in a real-world cohort at a tertiary academic center.
Methods: We conducted a retrospective cohort study of adult patients with obesity who underwent ESG between 2013 and 2022. Inclusion criteria were age ≥18 years, available pre-procedure and 1-year follow-up data, and absence of prior metabolic or bariatric surgery. Clinical parameters were collected including age, sex, race, weight, height, BMI, blood pressure, and lipid profiles. The primary outcomes were changes in 10-year and lifetime ASCVD risk scores, calculated using the ACC/AHA pooled cohort equations. Secondary outcomes included total body weight loss percentage (TBWL%) and changes in systolic and diastolic blood pressure, total cholesterol, LDL-C, and HDL-C. Matched paired t-tests were used for comparisons of pre- and post-ESG values.
Results: Out of 183 patients, a total of 33 patients with pre- and post-ESG data were included in the analysis (mean age 49.6 ± 11.1 years; 84.9% female; 93.9% White). Baseline demographics and clinical data are presented in Table 1. At 1-year post-ESG, 10-year ASCVD risk dropped from 1.8% to 1.1% (mean change −0.7%, p< 0.01; Figure 1A), while lifetime ASCVD risk decreased from 37.3% to 32.9% (mean change −4.4%, p=0.09; Figure 1B). Patients experienced significant TBWL% (−12.9 ± 2.2%, p< 0.01; Figure 1C). Lipid changes were not statistically significant: LDL-C (−2.3 mg/dL, p=0.58; Figure 1D), total cholesterol (−6.3 mg/dL, p=0.19; Figure 1E), and HDL-C (+2.7 mg/dL, p=0.07 Figure 1F). Systolic blood pressure declined by −6.9 mmHg (p=0.006; Figure 1G), while changes in diastolic pressure were modest and non-significant (−1.9 mmHg, p=0.36; Figure 1H).
Discussion: In this clinical cohort, ESG was associated with significant weight loss and clinically meaningful improvements in 10-year ASCVD risk. Further prospective and comparative studies with larger cohort size are warranted to validate these findings.
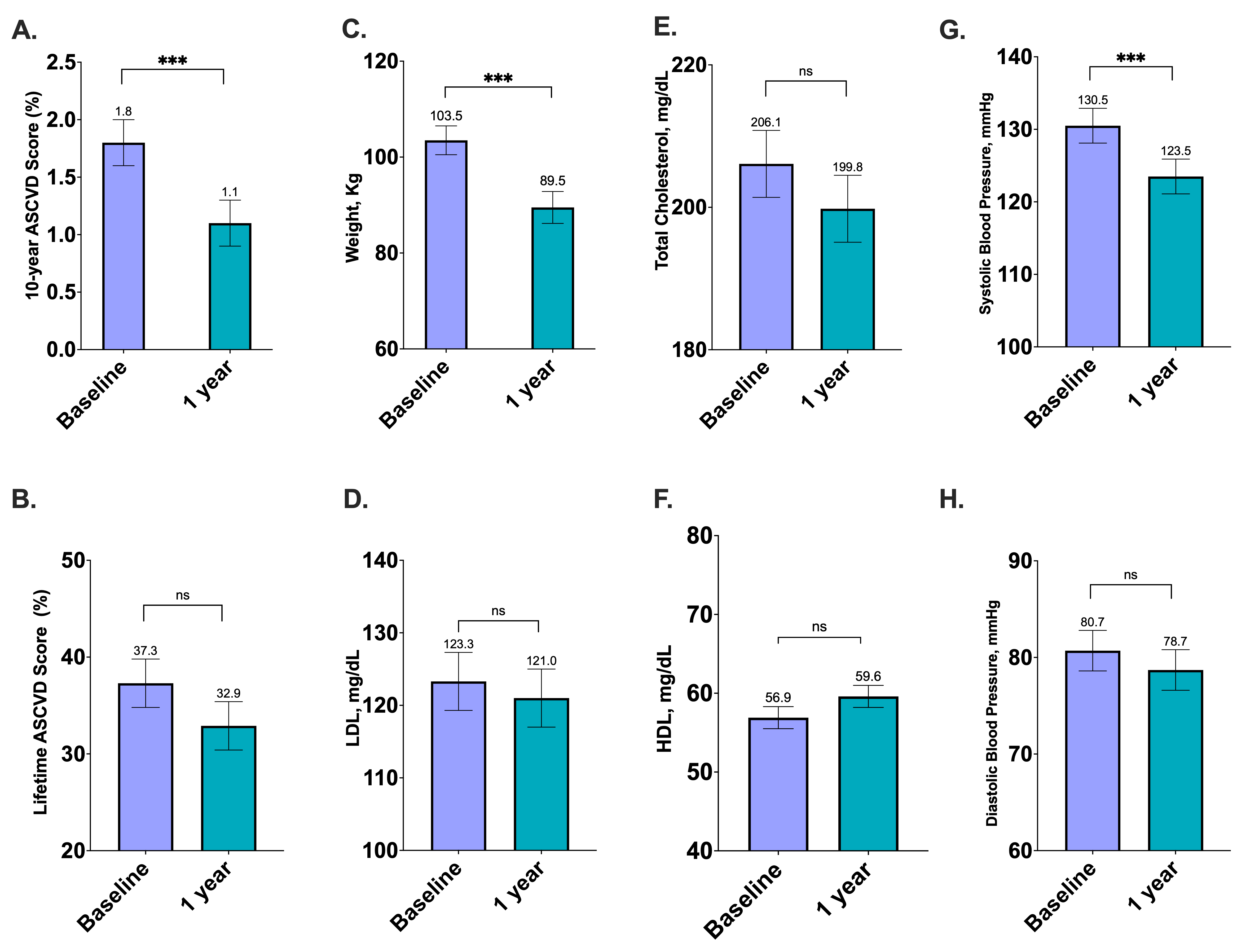
Figure: Table 1: Baseline Demographic and Cardiometabolic Characteristics of Patients Undergoing Endoscopic Sleeve Gastroplasty.
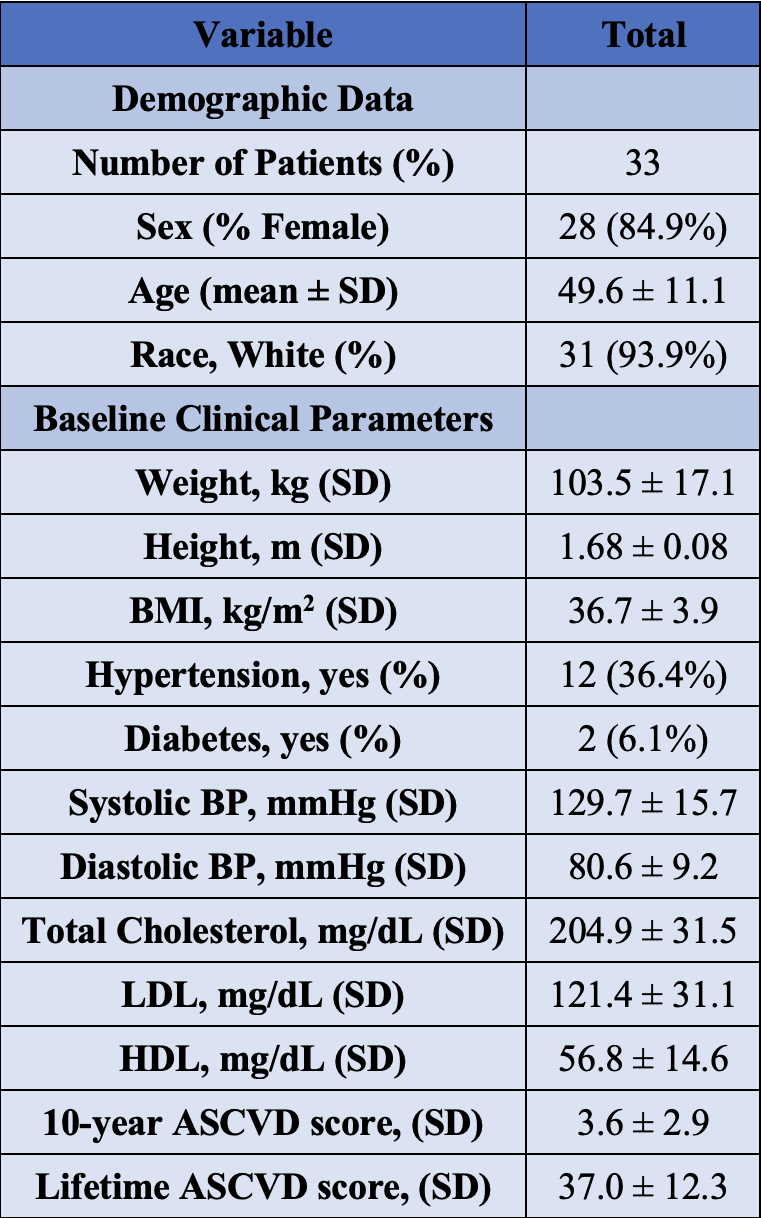
Figure: Figure 1: One-Year Changes in Cardiometabolic Risk Markers Following Endoscopic Sleeve Gastroplasty. (***: p<0.01; ns: Non-significant)
Disclosures:
Wissam Ghusn indicated no relevant financial relationships.
Yara Salameh indicated no relevant financial relationships.
Maria Antonia Espinosa indicated no relevant financial relationships.
Jose Villamarin indicated no relevant financial relationships.
Karim Al Annan indicated no relevant financial relationships.
Lea Sayegh indicated no relevant financial relationships.
Serena J. Rahme indicated no relevant financial relationships.
Kamal Abi Mosleh indicated no relevant financial relationships.
Johnny Bou Saba indicated no relevant financial relationships.
Khushboo Gala indicated no relevant financial relationships.
Eric Vargas indicated no relevant financial relationships.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Consultant, Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-Tagss – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Microtech – Consultant. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support. Sotelix – Consultant. Steris – Consultant.
Wissam Ghusn, MD1, Yara Salameh, MD2, Maria Antonia Espinosa, MD3, Jose Villamarin, MD3, Karim Al Annan, MD4, Lea Sayegh, MD5, Serena J. Rahme, MD3, Kamal Abi Mosleh, MD3, Johnny Bou Saba, MD6, Khushboo Gala, MBBS3, Eric J.. Vargas, MD, MS3, Andrew Storm, MD3. P5687 - Transforming Cardiovascular Risk Through Endoscopic Sleeve Gastroplasty: 1-Year Outcomes in a Real-World Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
