Tuesday Poster Session
Category: Interventional Endoscopy
P5684 - Increased Risk of ERCP-Related Complications in Patients With Decompensated Cirrhosis: A Real-World Multicenter Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hazem Abosheaishaa, MD
Mount Sinai West, Icahn School of Medicine at Mount Sinai
Queens, NY
Presenting Author(s)
Hazem Abosheaishaa, MD1, Mohamed Eldesouki, MD2, Ahmed Ibrahim, MD3, Ahmed Salem, MD4, Mohammed Abusuliman, MD5, Nermin Elhossiny, 6, Omar Abdelhalim, MD7, Mohammed Y. Youssef, MD8, Mohamed Mahmoud, MD9, Mahmoud Nassar, MD, PhD, MSc, MPA10, Mohammad Bilal, MD, FACG11
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 2Saint Michael's Medical Center, New York Medical College, Newark, NJ; 3Medical University of South Carolina, Charleston, SC; 4Maimonides Medical Center, Brooklyn, NY; 5Henry Ford Hospital, Detroit, MI; 6St Mary General hospital prime healthcare , NJ , USA, Passaic, NJ; 7Icahn School of Medicine at Mount Sinai, Queens, NY; 8Hunt Regional Medical Center, Greenville, TX; 9Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 10Division of Endocrinology and Diabetes, Larner College of Medicine, University of Vermont, Burlington, Vermont, USA, Buffalo, NY; 11University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) is often needed in patients with liver disease. However, the safety of ERCP in those with decompensated cirrhosis remains uncertain. We aimed to evaluate the risk of post-ERCP adverse events (AEs) in patients with compensated versus decompensated cirrhosis.
Methods: We queried the TriNetX Research Network, a national research database, to identify adult patients (≥ 18 years) with cirrhosis who underwent ERCP between 2010 and 2025. Patients were stratified into compensated and decompensated cirrhosis based on ICD-10 codes for hepatic decompensating events (ascites, hepatic encephalopathy, variceal hemorrhage, or spontaneous bacterial peritonitis). Propensity score matching (1:1) was used to adjust for baseline demographics, comorbidities, and laboratory values. We evaluated post-ERCP outcomes using odds ratios (OR) with 95% confidence intervals (CI).
Results: A total of 54,039 patients with cirrhosis were identified, including 5,939 with decompensated cirrhosis. The mean age was 61 years in compensated cirrhosis vs. 60 years in decompensated cirrhosis. After matching, each group had 5,939 patients (mean [SD] age, 61 [15] years; 42% women, and were evenly matched in baseline characteristics and liver disease severity (Table 1). Compared to compensated cirrhosis, patients with decompensated cirrhosis had significantly higher odds of post-ERCP pancreatitis (4.4% vs 3.1%; OR: 1.40, 95% CI: 1.13–1.74, p = 0.002), bleeding (4.5% vs 2.6%; OR: 1.79, 95% CI: 1.52–2.11, p < 0.001), cholangitis (5.5% vs 3.3%; OR: 1.71, 95% CI: 1.46–2.01, p < 0.001), and perforation (0.4% vs 0.2%; OR: 2.64, 95% CI: 1.21–5.76, p = 0.01; Table 2). Decompensated cirrhosis was also associated with increased 30-day mortality (5.6% vs 1.9%; OR: 2.82, 95% CI: 2.32–3.55, p < 0.001; Table 2). There were no significant differences in the rates of cholecystitis between the two groups (1.5% vs 1.6%; OR: 0.95, 95% CI: 0.79–1.14, p = 0.57; Table 2).
Discussion: In this large, real-world cohort, patients with decompensated cirrhosis undergoing ERCP had significantly increased risks of post-procedural AEs, including pancreatitis, bleeding, cholangitis, perforation, and 30-day mortality. These findings suggest that the severity of liver disease should be a critical consideration when assessing the risks and benefits of ERCP.
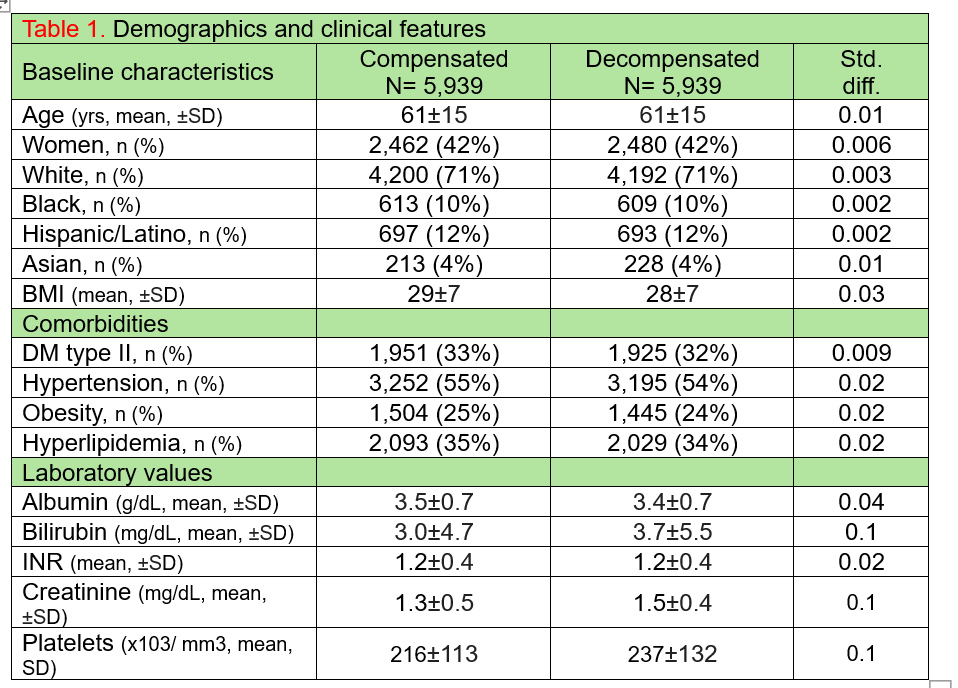
Figure: Demographics and clinical features
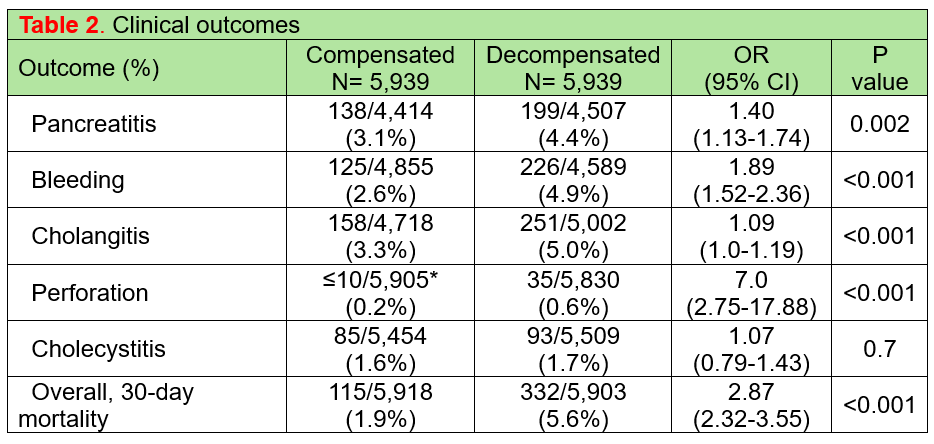
Figure: Clinical outcomes
Disclosures:
Hazem Abosheaishaa indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Ahmed Ibrahim indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Mohammed Abusuliman indicated no relevant financial relationships.
Nermin Elhossiny indicated no relevant financial relationships.
Omar Abdelhalim indicated no relevant financial relationships.
Mohammed Y. Youssef indicated no relevant financial relationships.
Mohamed Mahmoud indicated no relevant financial relationships.
Mahmoud Nassar indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Hazem Abosheaishaa, MD1, Mohamed Eldesouki, MD2, Ahmed Ibrahim, MD3, Ahmed Salem, MD4, Mohammed Abusuliman, MD5, Nermin Elhossiny, 6, Omar Abdelhalim, MD7, Mohammed Y. Youssef, MD8, Mohamed Mahmoud, MD9, Mahmoud Nassar, MD, PhD, MSc, MPA10, Mohammad Bilal, MD, FACG11. P5684 - Increased Risk of ERCP-Related Complications in Patients With Decompensated Cirrhosis: A Real-World Multicenter Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 2Saint Michael's Medical Center, New York Medical College, Newark, NJ; 3Medical University of South Carolina, Charleston, SC; 4Maimonides Medical Center, Brooklyn, NY; 5Henry Ford Hospital, Detroit, MI; 6St Mary General hospital prime healthcare , NJ , USA, Passaic, NJ; 7Icahn School of Medicine at Mount Sinai, Queens, NY; 8Hunt Regional Medical Center, Greenville, TX; 9Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 10Division of Endocrinology and Diabetes, Larner College of Medicine, University of Vermont, Burlington, Vermont, USA, Buffalo, NY; 11University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) is often needed in patients with liver disease. However, the safety of ERCP in those with decompensated cirrhosis remains uncertain. We aimed to evaluate the risk of post-ERCP adverse events (AEs) in patients with compensated versus decompensated cirrhosis.
Methods: We queried the TriNetX Research Network, a national research database, to identify adult patients (≥ 18 years) with cirrhosis who underwent ERCP between 2010 and 2025. Patients were stratified into compensated and decompensated cirrhosis based on ICD-10 codes for hepatic decompensating events (ascites, hepatic encephalopathy, variceal hemorrhage, or spontaneous bacterial peritonitis). Propensity score matching (1:1) was used to adjust for baseline demographics, comorbidities, and laboratory values. We evaluated post-ERCP outcomes using odds ratios (OR) with 95% confidence intervals (CI).
Results: A total of 54,039 patients with cirrhosis were identified, including 5,939 with decompensated cirrhosis. The mean age was 61 years in compensated cirrhosis vs. 60 years in decompensated cirrhosis. After matching, each group had 5,939 patients (mean [SD] age, 61 [15] years; 42% women, and were evenly matched in baseline characteristics and liver disease severity (Table 1). Compared to compensated cirrhosis, patients with decompensated cirrhosis had significantly higher odds of post-ERCP pancreatitis (4.4% vs 3.1%; OR: 1.40, 95% CI: 1.13–1.74, p = 0.002), bleeding (4.5% vs 2.6%; OR: 1.79, 95% CI: 1.52–2.11, p < 0.001), cholangitis (5.5% vs 3.3%; OR: 1.71, 95% CI: 1.46–2.01, p < 0.001), and perforation (0.4% vs 0.2%; OR: 2.64, 95% CI: 1.21–5.76, p = 0.01; Table 2). Decompensated cirrhosis was also associated with increased 30-day mortality (5.6% vs 1.9%; OR: 2.82, 95% CI: 2.32–3.55, p < 0.001; Table 2). There were no significant differences in the rates of cholecystitis between the two groups (1.5% vs 1.6%; OR: 0.95, 95% CI: 0.79–1.14, p = 0.57; Table 2).
Discussion: In this large, real-world cohort, patients with decompensated cirrhosis undergoing ERCP had significantly increased risks of post-procedural AEs, including pancreatitis, bleeding, cholangitis, perforation, and 30-day mortality. These findings suggest that the severity of liver disease should be a critical consideration when assessing the risks and benefits of ERCP.
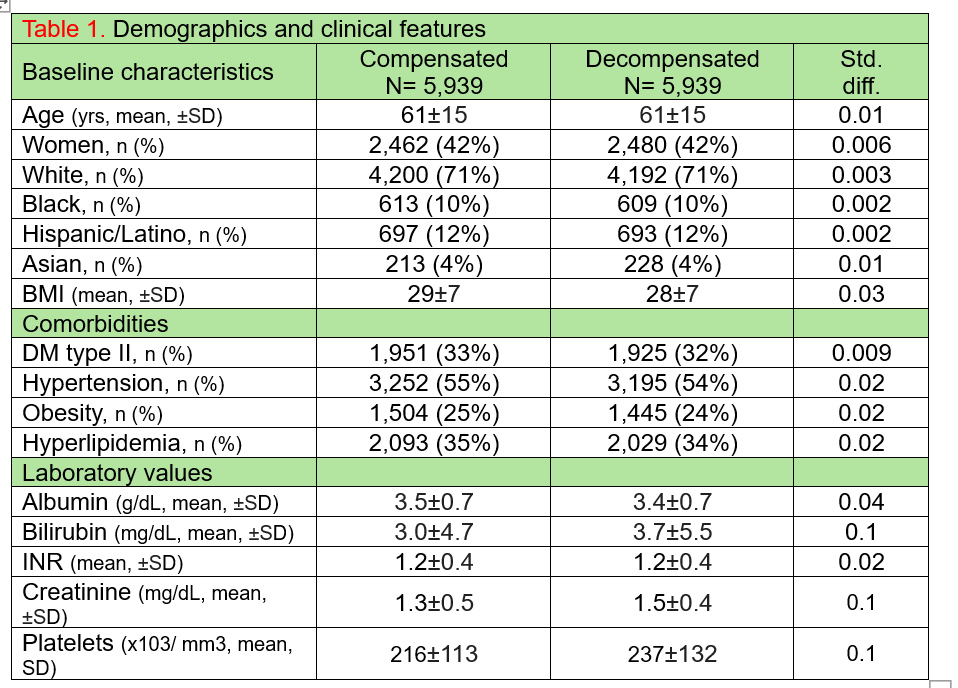
Figure: Demographics and clinical features
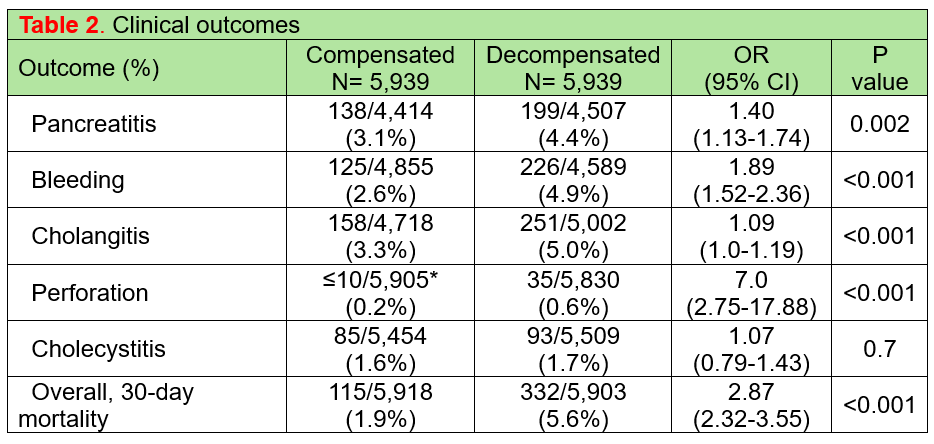
Figure: Clinical outcomes
Disclosures:
Hazem Abosheaishaa indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Ahmed Ibrahim indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Mohammed Abusuliman indicated no relevant financial relationships.
Nermin Elhossiny indicated no relevant financial relationships.
Omar Abdelhalim indicated no relevant financial relationships.
Mohammed Y. Youssef indicated no relevant financial relationships.
Mohamed Mahmoud indicated no relevant financial relationships.
Mahmoud Nassar indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Hazem Abosheaishaa, MD1, Mohamed Eldesouki, MD2, Ahmed Ibrahim, MD3, Ahmed Salem, MD4, Mohammed Abusuliman, MD5, Nermin Elhossiny, 6, Omar Abdelhalim, MD7, Mohammed Y. Youssef, MD8, Mohamed Mahmoud, MD9, Mahmoud Nassar, MD, PhD, MSc, MPA10, Mohammad Bilal, MD, FACG11. P5684 - Increased Risk of ERCP-Related Complications in Patients With Decompensated Cirrhosis: A Real-World Multicenter Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
