Tuesday Poster Session
Category: Interventional Endoscopy
P5655 - Incidence and Severity of Post-ESD Bleeding in a Heterogenous Population: A Retrospective Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- ES
Eitan Scheinthal, DO
Aurora Healthcare
Milwaukee, WI
Presenting Author(s)
Eitan Scheinthal, DO1, Naaz Khan, BS2, Wesley Vu, BS2, Caitlyn Spencer, BSN, RN3, Sarah Clark, MSN, APNP3, Mohammed Qadeer, MD, MPH3
1Aurora Healthcare, Milwaukee, WI; 2Rosalind Franklin University of Medicine and Science, North Chicago, IL; 3Aurora Healthcare, Kenosha, WI
Introduction: Endoscopic submucosal dissection (ESD) has emerged as a minimally invasive technique for resecting premalignant and early-stage gastrointestinal neoplasms. Compared to endoscopic mucosal resection (EMR), ESD is reported to have higher rates of adverse outcomes such as bleeding and perforation. Data on post-ESD bleeding in Western populations is limited. We aimed to assess the incidence and severity of bleeding associated with ESD.
Methods: We conducted a retrospective analysis of a prospectively collected database of patients who underwent ESD between April 2014 and September 2024 at a regional referral center in Wisconsin, USA. All ESDs were performed by a single operator. The study was IRB-approved. Data collected included demographic information, procedural details, adverse events and post-ESD clinical course and management, intraprocedural complications, hospital admission for bleeding, hemodynamic instability defined as hypotension and tachycardia, hemoglobin (Hgb) drop from baseline, transfusion requirements, and recurrent bleeding. Descriptive statistics were reported; continuous variables were summarized using means and standard deviations.
Results: A total of 460 ESDs were performed during the study period. No surgical or interventional radiology intervention was needed for intraprocedural bleeding. A total of 16 patients (3.47%) developed delayed bleeding (Table 1). Of these 16 patients, 11 (2.4%) had significant bleeding that required hospital admission (Table 2). Patients with delayed bleeding were more likely to have ASA ≥3 and multiple co-morbidities. Sixty-two percent of these patients had mucosal closure after ESD. Bleeding started after a mean duration of 4.6 days following ESD [range 1-12 days]. Among hospitalized patients for clinically significant bleeding 37.5% required packed red blood cell (PRBC) transfusion. Mean Hgb decline from baseline was 2.5g/dL. An average of 2.67 units PRBC transfusions were given along with endoscopic intervention for bleeding. One patient underwent embolization to control delayed bleeding. The mean hospital stay was 2.4 days [range 1-9]. Recurrent bleeding occurred in 25% of these patients. There were no long-term sequelae or mortality associated with bleeding.
Discussion: Although the incidence of clinically significant delayed bleeding after ESD is low at 2.4%, it is resource intensive requiring multiple interventions and potentially a protracted hospital course. Further research is needed to develop risk models for delayed bleeding.
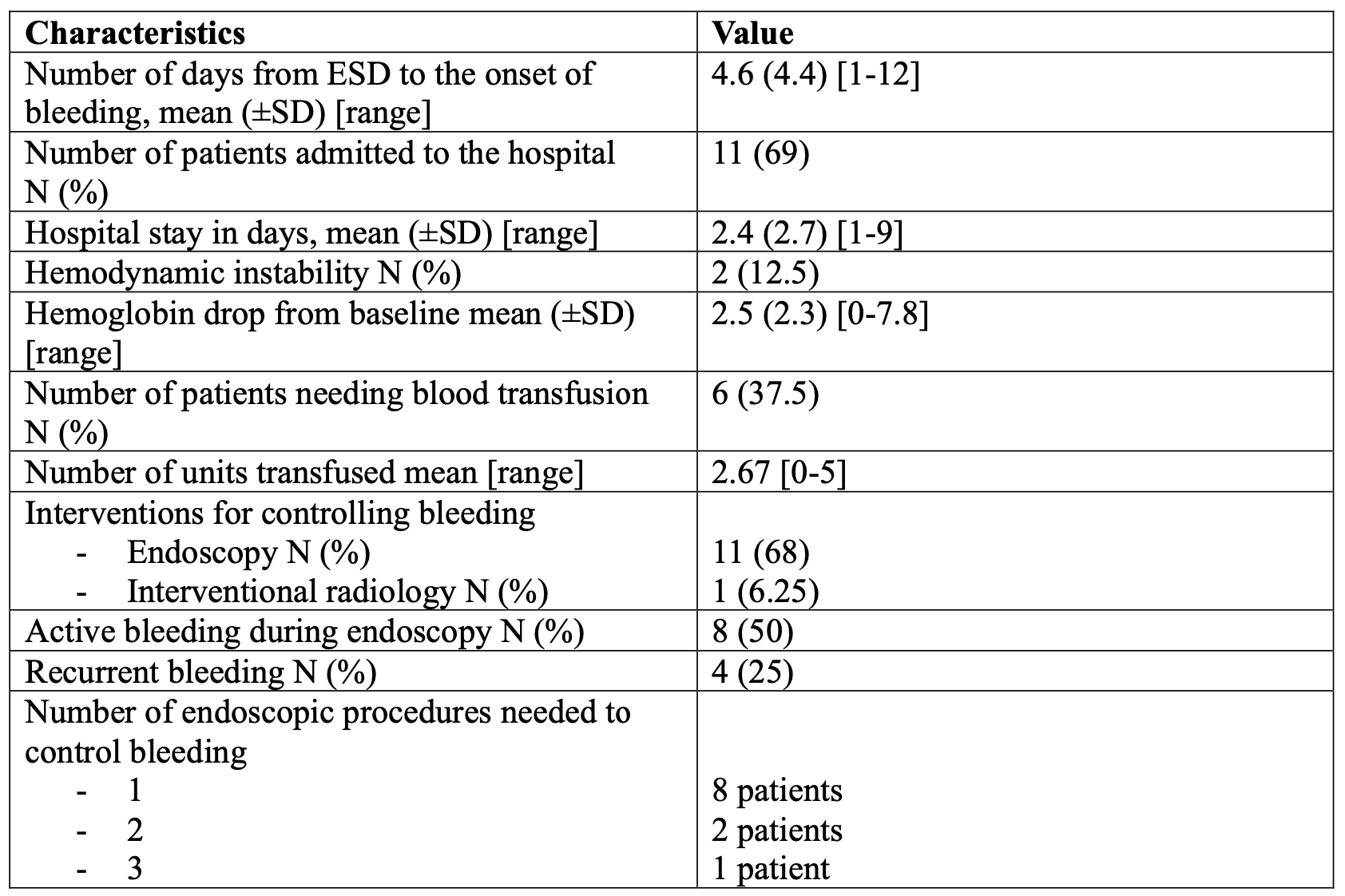
Figure: Table 1. Baseline characteristics of patients with delayed post ESD bleeding
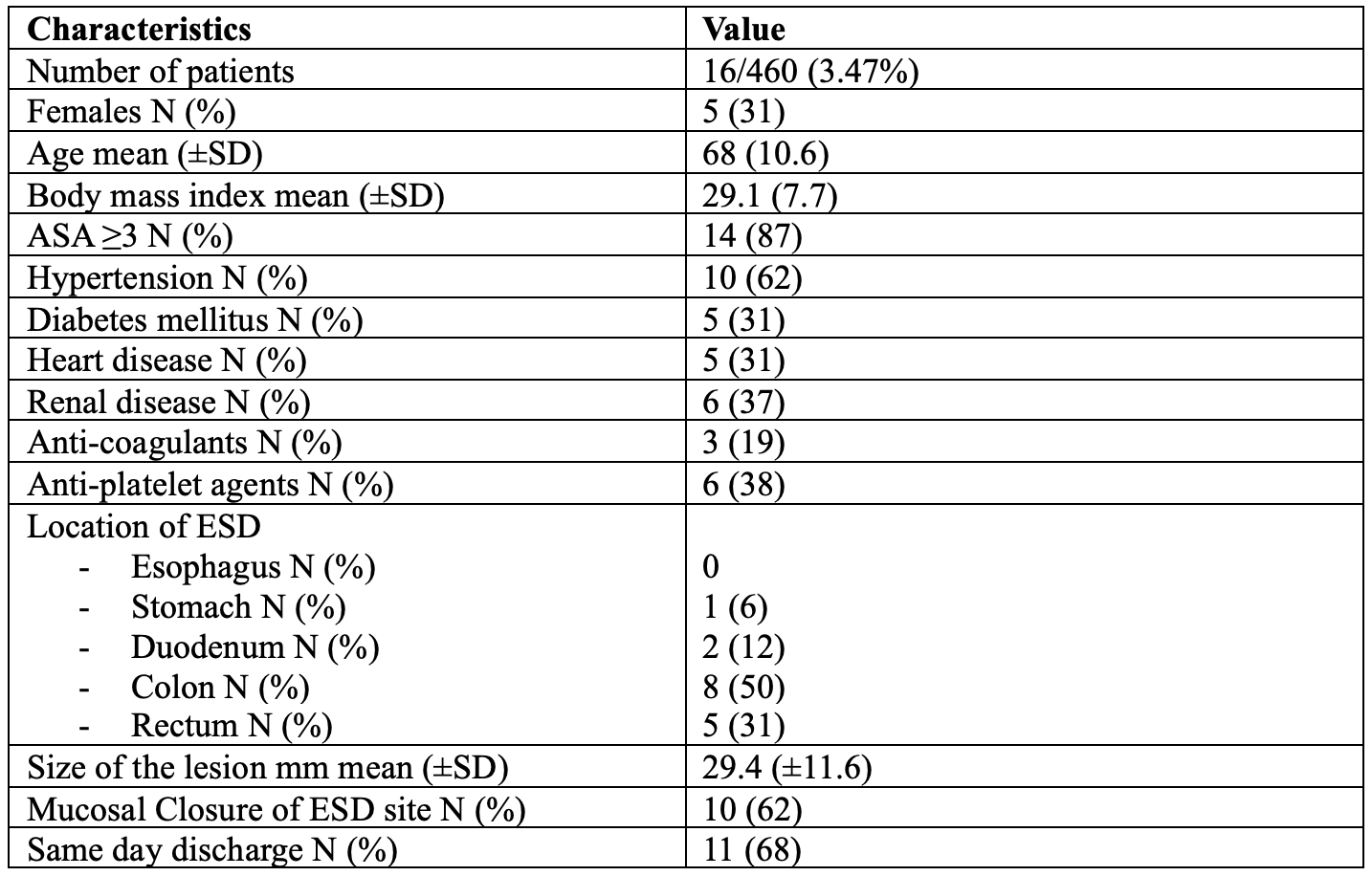
Figure: Table 2. Characteristics of delayed bleeding after ESD
Disclosures:
Eitan Scheinthal indicated no relevant financial relationships.
Naaz Khan indicated no relevant financial relationships.
Wesley Vu indicated no relevant financial relationships.
Caitlyn Spencer indicated no relevant financial relationships.
Sarah Clark indicated no relevant financial relationships.
Mohammed Qadeer indicated no relevant financial relationships.
Eitan Scheinthal, DO1, Naaz Khan, BS2, Wesley Vu, BS2, Caitlyn Spencer, BSN, RN3, Sarah Clark, MSN, APNP3, Mohammed Qadeer, MD, MPH3. P5655 - Incidence and Severity of Post-ESD Bleeding in a Heterogenous Population: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Aurora Healthcare, Milwaukee, WI; 2Rosalind Franklin University of Medicine and Science, North Chicago, IL; 3Aurora Healthcare, Kenosha, WI
Introduction: Endoscopic submucosal dissection (ESD) has emerged as a minimally invasive technique for resecting premalignant and early-stage gastrointestinal neoplasms. Compared to endoscopic mucosal resection (EMR), ESD is reported to have higher rates of adverse outcomes such as bleeding and perforation. Data on post-ESD bleeding in Western populations is limited. We aimed to assess the incidence and severity of bleeding associated with ESD.
Methods: We conducted a retrospective analysis of a prospectively collected database of patients who underwent ESD between April 2014 and September 2024 at a regional referral center in Wisconsin, USA. All ESDs were performed by a single operator. The study was IRB-approved. Data collected included demographic information, procedural details, adverse events and post-ESD clinical course and management, intraprocedural complications, hospital admission for bleeding, hemodynamic instability defined as hypotension and tachycardia, hemoglobin (Hgb) drop from baseline, transfusion requirements, and recurrent bleeding. Descriptive statistics were reported; continuous variables were summarized using means and standard deviations.
Results: A total of 460 ESDs were performed during the study period. No surgical or interventional radiology intervention was needed for intraprocedural bleeding. A total of 16 patients (3.47%) developed delayed bleeding (Table 1). Of these 16 patients, 11 (2.4%) had significant bleeding that required hospital admission (Table 2). Patients with delayed bleeding were more likely to have ASA ≥3 and multiple co-morbidities. Sixty-two percent of these patients had mucosal closure after ESD. Bleeding started after a mean duration of 4.6 days following ESD [range 1-12 days]. Among hospitalized patients for clinically significant bleeding 37.5% required packed red blood cell (PRBC) transfusion. Mean Hgb decline from baseline was 2.5g/dL. An average of 2.67 units PRBC transfusions were given along with endoscopic intervention for bleeding. One patient underwent embolization to control delayed bleeding. The mean hospital stay was 2.4 days [range 1-9]. Recurrent bleeding occurred in 25% of these patients. There were no long-term sequelae or mortality associated with bleeding.
Discussion: Although the incidence of clinically significant delayed bleeding after ESD is low at 2.4%, it is resource intensive requiring multiple interventions and potentially a protracted hospital course. Further research is needed to develop risk models for delayed bleeding.
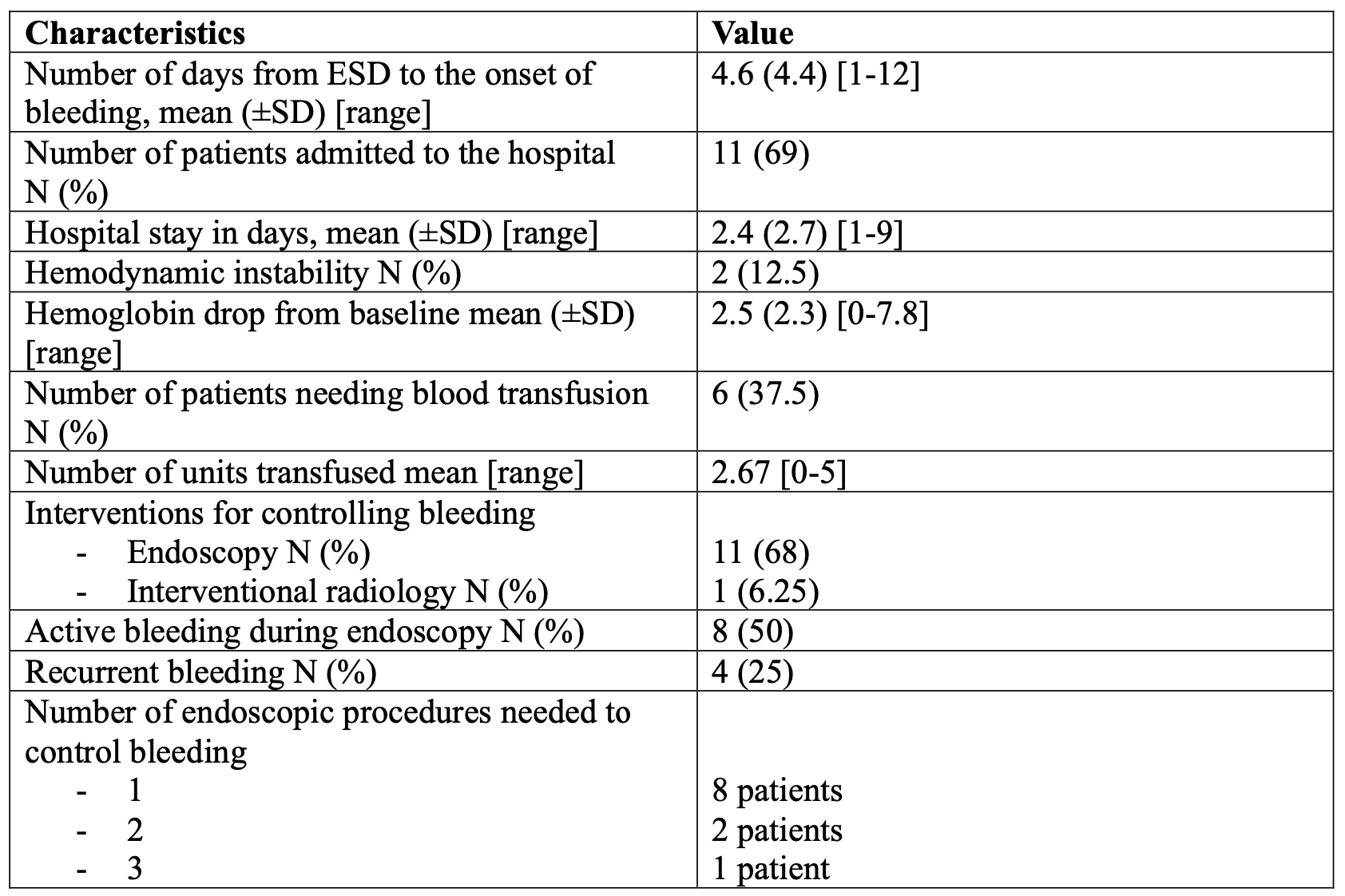
Figure: Table 1. Baseline characteristics of patients with delayed post ESD bleeding
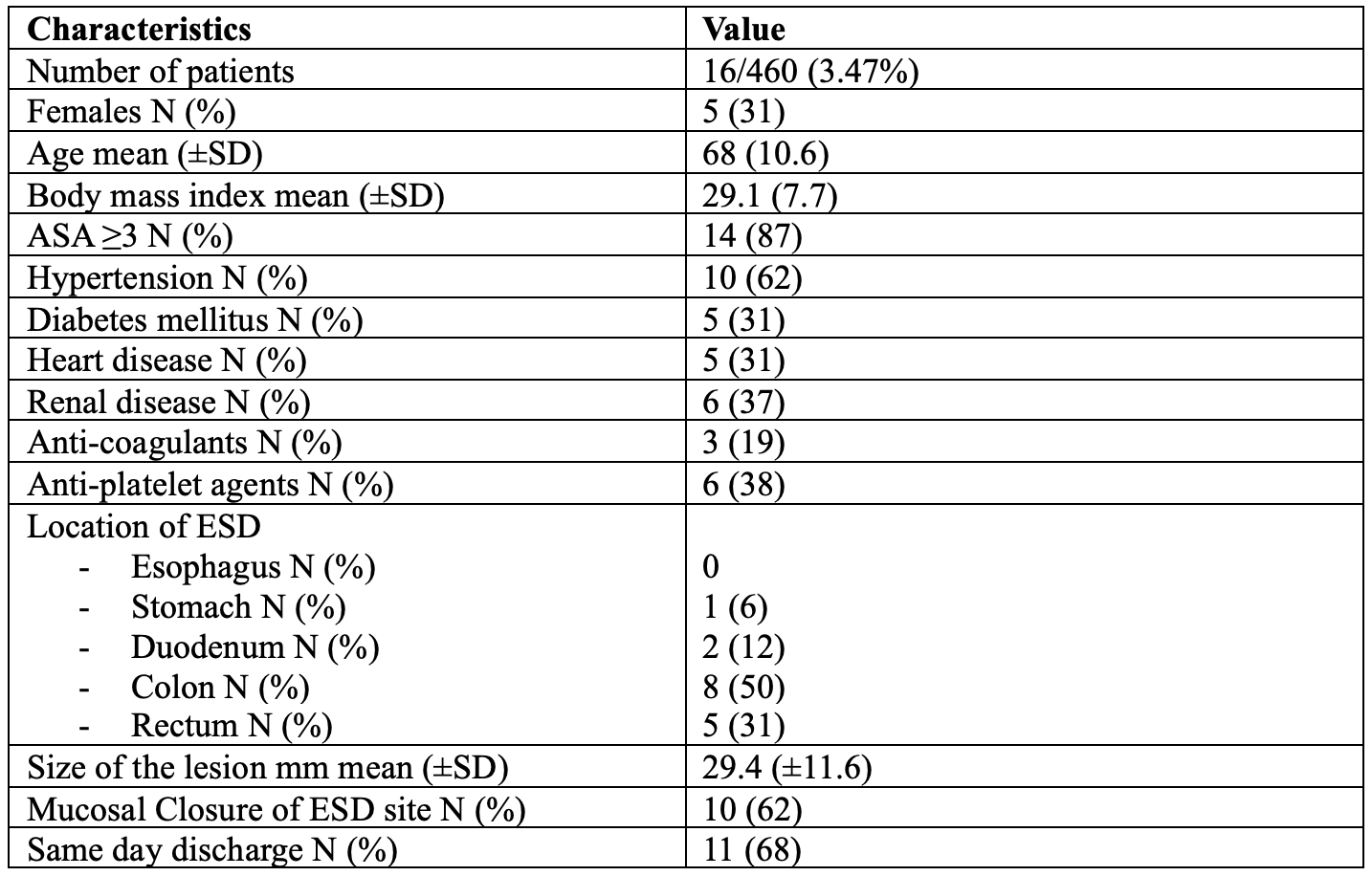
Figure: Table 2. Characteristics of delayed bleeding after ESD
Disclosures:
Eitan Scheinthal indicated no relevant financial relationships.
Naaz Khan indicated no relevant financial relationships.
Wesley Vu indicated no relevant financial relationships.
Caitlyn Spencer indicated no relevant financial relationships.
Sarah Clark indicated no relevant financial relationships.
Mohammed Qadeer indicated no relevant financial relationships.
Eitan Scheinthal, DO1, Naaz Khan, BS2, Wesley Vu, BS2, Caitlyn Spencer, BSN, RN3, Sarah Clark, MSN, APNP3, Mohammed Qadeer, MD, MPH3. P5655 - Incidence and Severity of Post-ESD Bleeding in a Heterogenous Population: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

