Tuesday Poster Session
Category: Infections and Microbiome
P5643 - Diagnosis of Whipple Disease in a Patient Misdiagnosed With Seronegative Rheumatoid Arthritis: Uncovering the Cause of Anemia and Positive Occult Blood
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Thaddeus Sullivan, DO
Arnot Ogden Medical Center
Clinton, NY
Presenting Author(s)
Thaddeus Sullivan, DO1, Bradley Sklar, MD2, Gurtej Dhaliwal, MD3, Tenzin Tseky, DO3, Brian Sowka, DO3, Brendan Gregg, DO3, Jose Russe-Russe, MD3, Gary Valvano, DO3, Bruno Mazza, MD3
1Arnot Ogden Medical Center, Clinton, NY; 2Digestive Disease Medicine, New Hartford, NY; 3Arnot Ogden Medical Center, Elmira, NY
Introduction: Whipple’s disease is a rare bacterial infection caused by Tropheryma whipplei and most commonly affects White males of European descent. It can affect not only the gastrointestinal tract, but also the musculoskeletal, cardiovascular and neurological systems. Early diagnosis is key to preventing significant health issues.
Case Description/
Methods: A 63-year-old male with past medical history of hypertension, hyperlipidemia, atrial fibrillation status post ablation, not on anticoagulation, unexplained congestive heart failure with EF 40-45% and seronegative rheumatoid arthritis (RA) on Rinvoq presented to emergency department with shortness of breath, diarrhea, and abdominal distension for 3 days. Hemoglobin (Hg) on admission was 10 with a baseline of 12. The patient's last colonoscopy was 3 years prior showing tubular adenoma in cecum and diverticulosis in sigmoid/descending colon. Patient had no prior EGD. Guaiac stool was positive. He denied any history of reflux, antacid, NSAID, tobacco or alcohol use. Patient underwent EGD to rule out gastritis, esophagitis, peptic ulcers or AVM’s. Findings included severe gastritis with erosions in the gastric body and antrum and severe duodenitis in the bulb, 3rd and 4th portion of duodenum. Differentials included Histoplasmosis and Whipple's disease. Pathology showed expansion of the duodenal villi by foamy macrophages and scattered dilated lacteals. The foamy macrophages contained PAS-positive diastase resistant coarse granules, characteristic of Whipple's disease. They were positive for GMS, but morphology is consistent with bacillary forms not the larger ovoid budding yeast of histoplasmosis. Patient started IV ceftriaxone for 4 weeks and then transitioned to Bactrim BID for one year. Patient was taken off Rinvoq and prednisone as his joint pain was likely from Whipple disease and not RA. He lost 30 lbs prior to his diagnosis and gained it back one year later. Migratory arthritis and GI symptoms have improved significantly. Pathology report from repeat EGD one year later showed 80% reduction in number of foamy histiocytes with pale staining PAS indicative of therapeutic response. Bactrim was extended to 2 years per protocol as there was improvement.
Discussion: This case highlights the importance of early diagnosis of Whipple’s disease to prevent widespread damage. It is important to keep Whipple’s disease in the differential especially in patients with seronegative rheumatoid factor with persistent arthritis not improving on immunosuppressive therapy.
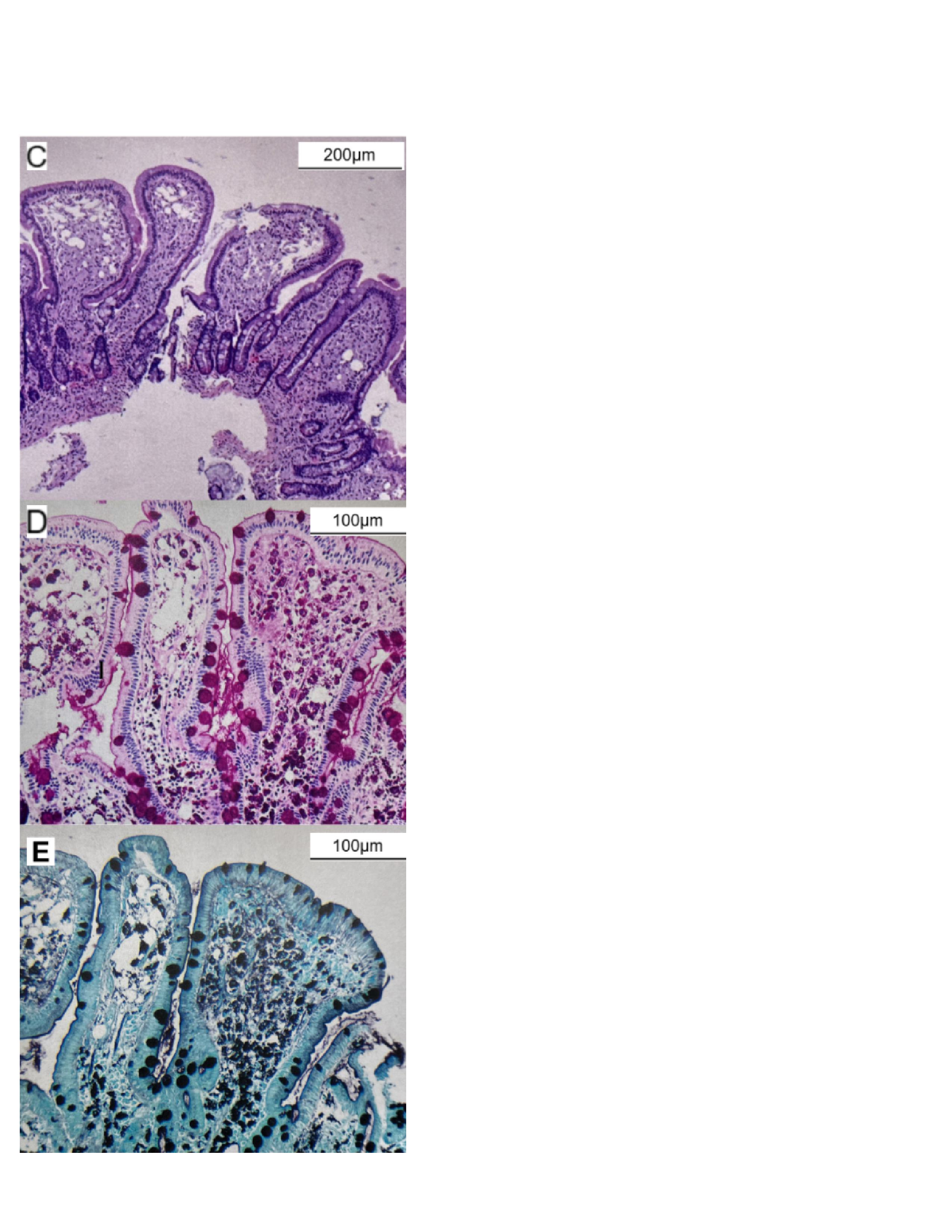
Figure: A. Severe gastritis with erosions in the antrum
B. Severe duodenitis
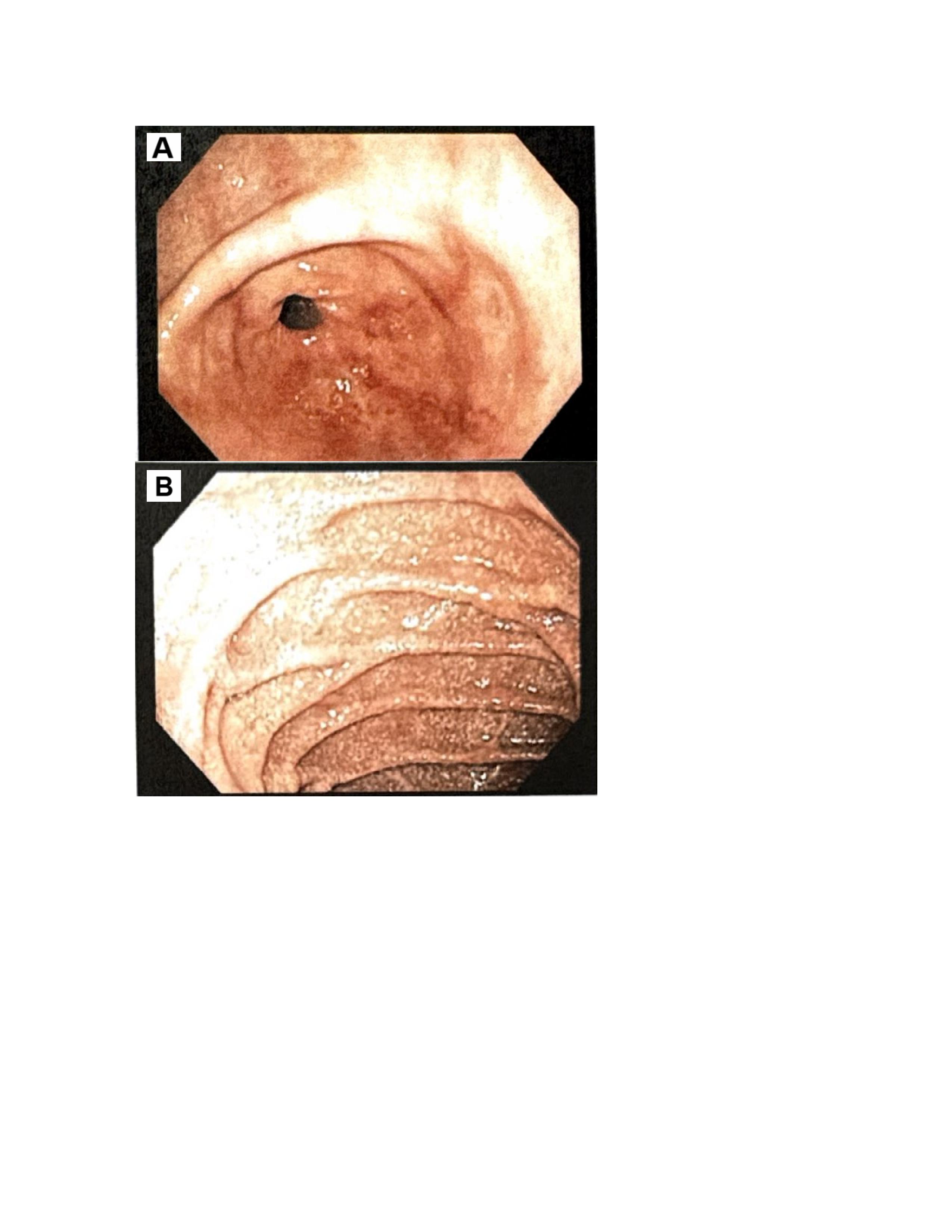
Figure: C. Hematoxylin and eosin (H&E) staining
D. Periodic acid–Schiff (PAS) staining
E. Grocott-Gomori's methenamine silver (GMS) staining
Disclosures:
Thaddeus Sullivan indicated no relevant financial relationships.
Bradley Sklar indicated no relevant financial relationships.
Gurtej Dhaliwal indicated no relevant financial relationships.
Tenzin Tseky indicated no relevant financial relationships.
Brian Sowka indicated no relevant financial relationships.
Brendan Gregg indicated no relevant financial relationships.
Jose Russe-Russe indicated no relevant financial relationships.
Gary Valvano indicated no relevant financial relationships.
Bruno Mazza indicated no relevant financial relationships.
Thaddeus Sullivan, DO1, Bradley Sklar, MD2, Gurtej Dhaliwal, MD3, Tenzin Tseky, DO3, Brian Sowka, DO3, Brendan Gregg, DO3, Jose Russe-Russe, MD3, Gary Valvano, DO3, Bruno Mazza, MD3. P5643 - Diagnosis of Whipple Disease in a Patient Misdiagnosed With Seronegative Rheumatoid Arthritis: Uncovering the Cause of Anemia and Positive Occult Blood, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Arnot Ogden Medical Center, Clinton, NY; 2Digestive Disease Medicine, New Hartford, NY; 3Arnot Ogden Medical Center, Elmira, NY
Introduction: Whipple’s disease is a rare bacterial infection caused by Tropheryma whipplei and most commonly affects White males of European descent. It can affect not only the gastrointestinal tract, but also the musculoskeletal, cardiovascular and neurological systems. Early diagnosis is key to preventing significant health issues.
Case Description/
Methods: A 63-year-old male with past medical history of hypertension, hyperlipidemia, atrial fibrillation status post ablation, not on anticoagulation, unexplained congestive heart failure with EF 40-45% and seronegative rheumatoid arthritis (RA) on Rinvoq presented to emergency department with shortness of breath, diarrhea, and abdominal distension for 3 days. Hemoglobin (Hg) on admission was 10 with a baseline of 12. The patient's last colonoscopy was 3 years prior showing tubular adenoma in cecum and diverticulosis in sigmoid/descending colon. Patient had no prior EGD. Guaiac stool was positive. He denied any history of reflux, antacid, NSAID, tobacco or alcohol use. Patient underwent EGD to rule out gastritis, esophagitis, peptic ulcers or AVM’s. Findings included severe gastritis with erosions in the gastric body and antrum and severe duodenitis in the bulb, 3rd and 4th portion of duodenum. Differentials included Histoplasmosis and Whipple's disease. Pathology showed expansion of the duodenal villi by foamy macrophages and scattered dilated lacteals. The foamy macrophages contained PAS-positive diastase resistant coarse granules, characteristic of Whipple's disease. They were positive for GMS, but morphology is consistent with bacillary forms not the larger ovoid budding yeast of histoplasmosis. Patient started IV ceftriaxone for 4 weeks and then transitioned to Bactrim BID for one year. Patient was taken off Rinvoq and prednisone as his joint pain was likely from Whipple disease and not RA. He lost 30 lbs prior to his diagnosis and gained it back one year later. Migratory arthritis and GI symptoms have improved significantly. Pathology report from repeat EGD one year later showed 80% reduction in number of foamy histiocytes with pale staining PAS indicative of therapeutic response. Bactrim was extended to 2 years per protocol as there was improvement.
Discussion: This case highlights the importance of early diagnosis of Whipple’s disease to prevent widespread damage. It is important to keep Whipple’s disease in the differential especially in patients with seronegative rheumatoid factor with persistent arthritis not improving on immunosuppressive therapy.
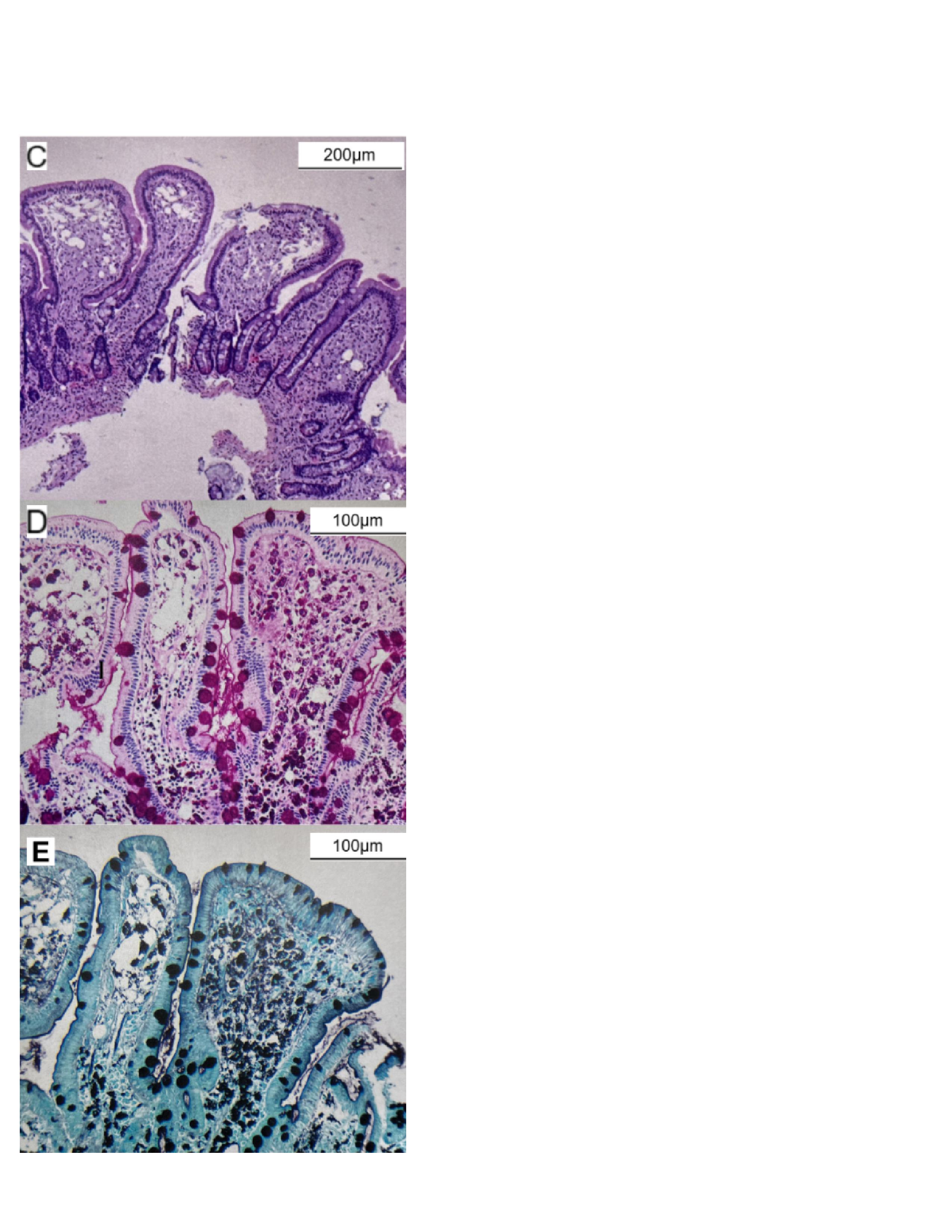
Figure: A. Severe gastritis with erosions in the antrum
B. Severe duodenitis
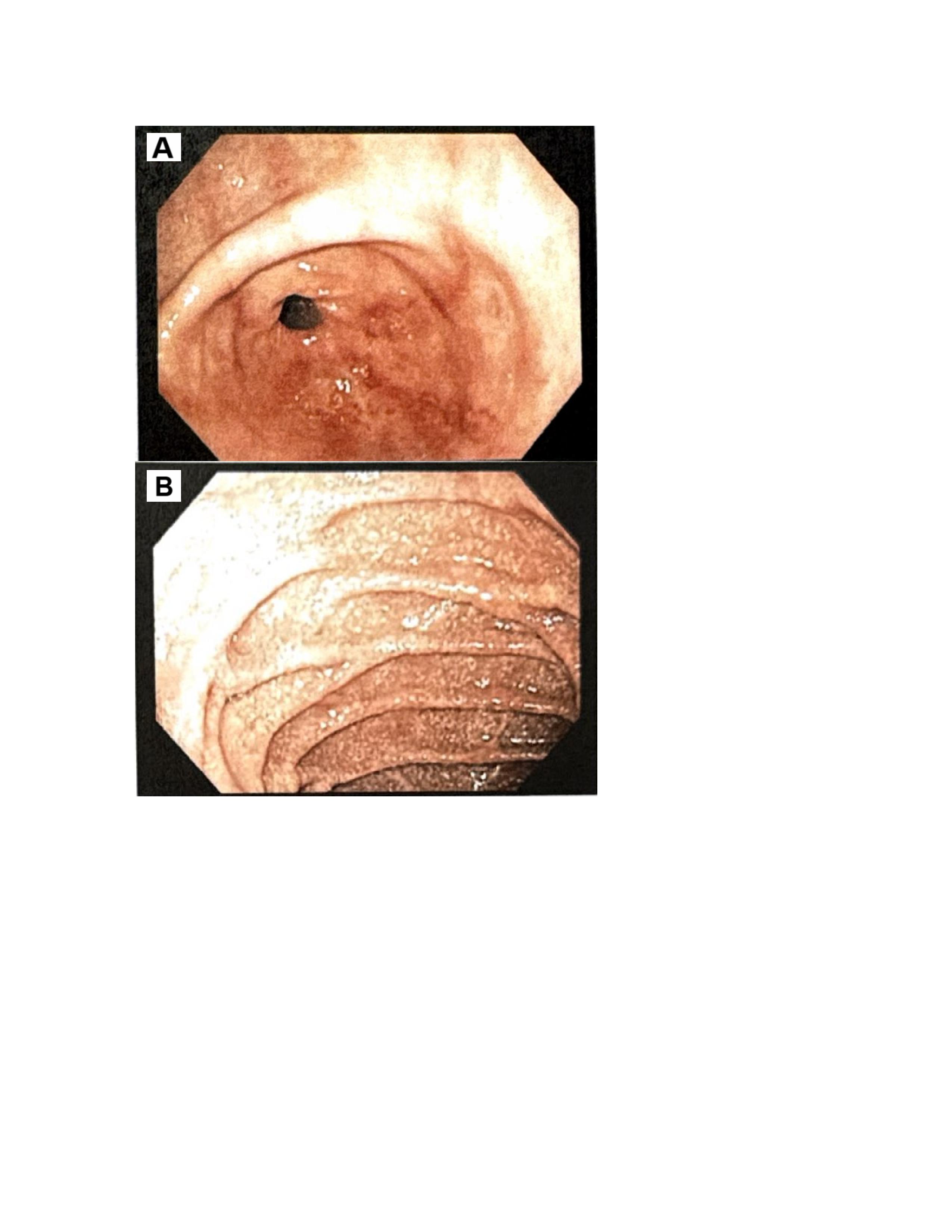
Figure: C. Hematoxylin and eosin (H&E) staining
D. Periodic acid–Schiff (PAS) staining
E. Grocott-Gomori's methenamine silver (GMS) staining
Disclosures:
Thaddeus Sullivan indicated no relevant financial relationships.
Bradley Sklar indicated no relevant financial relationships.
Gurtej Dhaliwal indicated no relevant financial relationships.
Tenzin Tseky indicated no relevant financial relationships.
Brian Sowka indicated no relevant financial relationships.
Brendan Gregg indicated no relevant financial relationships.
Jose Russe-Russe indicated no relevant financial relationships.
Gary Valvano indicated no relevant financial relationships.
Bruno Mazza indicated no relevant financial relationships.
Thaddeus Sullivan, DO1, Bradley Sklar, MD2, Gurtej Dhaliwal, MD3, Tenzin Tseky, DO3, Brian Sowka, DO3, Brendan Gregg, DO3, Jose Russe-Russe, MD3, Gary Valvano, DO3, Bruno Mazza, MD3. P5643 - Diagnosis of Whipple Disease in a Patient Misdiagnosed With Seronegative Rheumatoid Arthritis: Uncovering the Cause of Anemia and Positive Occult Blood, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
