Tuesday Poster Session
Category: Infections and Microbiome
P5639 - When Suspicion Outpaces Confirmation: A Case of Suspected Invasive Entamoeba Histolytica
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Arvin Razmdideh, DO
University of Texas Health Science Center at Tyler
Tyler, TX
Presenting Author(s)
Arvin Razmdideh, DO, John Martino, DO, Seth Tatel, MD
University of Texas Health Science Center at Tyler, Tyler, TX
Introduction: Entamoeba histolytica is a protozoan parasite notable for causing amebiasis. The global prevalence is about 1%, with the highest burden in regions with poor sanitation. Most cases are subclinical, but around 10% progress to invasive E. histolytica, leading to amoebic colitis and liver abscess. Risk groups include migrants from endemic areas, long-term travelers and immunocompromised individuals. This case presents a suspected invasive E. histolytica infection in a patient with intermittent fevers and no significant risk factors.
Case Description/
Methods: We describe a 56-year-old male with hypertension, presenting with intermittent fevers for five days and one episode of diarrhea. Imaging showed asymmetric wall thickening in the cecum, hepatic lesions, and an enhancing right mesentery lymph node. Given concerns for malignancy, general surgery was consulted who requested gastroenterology’s input prior to surgical intervention. Colonoscopy revealed large patchy ulceration in the cecum and smaller ulcerations in the ascending colon. Biopsies showed ulcerated mucosa with acute inflammation and reactive epithelial changes, negative for dysplasia or malignancy. Infectious disease was consulted, and the workup—including blood cultures, ova and parasite, cryptosporidium antigen, giardia antigen, and E. histolytica antigen—was negative. However, E. histolytica antibody was elevated. The patient underwent IR-guided drainage of liver lesions, yielding 120 ml of "chocolate" fluid which cultured rare gram-negative bacilli. He was started on flagyl and ceftriaxone, and a PICC line was placed for prolonged antibiotic treatment. He was discharged for outpatient follow-up with infectious disease.
Discussion: This report underscores the need to consider E. histolytica in the differential diagnosis, particularly in patients with atypical presentations, no clear risk factors, or inconclusive test results. E. histolytica antigen is often negative in extraintestinal disease despite colonic involvement, as fewer trophozoites are shed into the colon as the infection progresses to the liver, lowering antigen sensitivity. Even in low-prevalence areas like the U.S., a broad differential is crucial in patients with intermittent fevers and liver lesions.
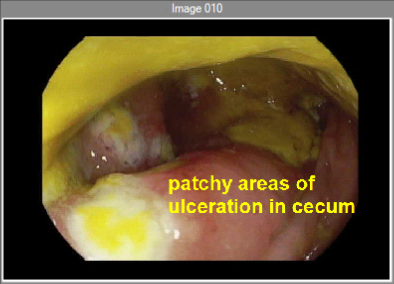
Figure: Patchy areas of ulceration seen in the cecum
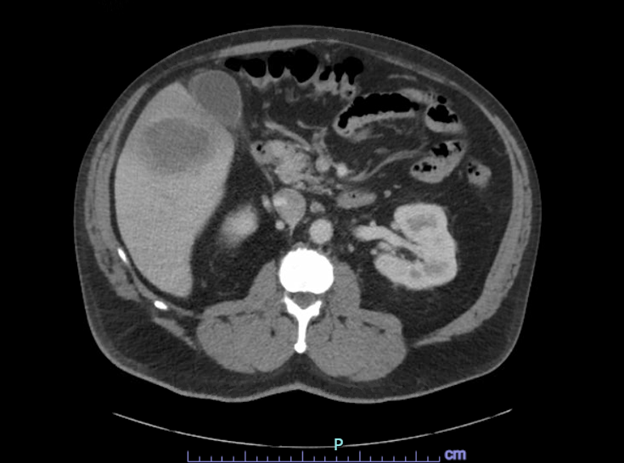
Figure: Liver mass seen on CT of the abdomen and pelvis
Disclosures:
Arvin Razmdideh indicated no relevant financial relationships.
John Martino indicated no relevant financial relationships.
Seth Tatel indicated no relevant financial relationships.
Arvin Razmdideh, DO, John Martino, DO, Seth Tatel, MD. P5639 - When Suspicion Outpaces Confirmation: A Case of Suspected Invasive Entamoeba Histolytica, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Texas Health Science Center at Tyler, Tyler, TX
Introduction: Entamoeba histolytica is a protozoan parasite notable for causing amebiasis. The global prevalence is about 1%, with the highest burden in regions with poor sanitation. Most cases are subclinical, but around 10% progress to invasive E. histolytica, leading to amoebic colitis and liver abscess. Risk groups include migrants from endemic areas, long-term travelers and immunocompromised individuals. This case presents a suspected invasive E. histolytica infection in a patient with intermittent fevers and no significant risk factors.
Case Description/
Methods: We describe a 56-year-old male with hypertension, presenting with intermittent fevers for five days and one episode of diarrhea. Imaging showed asymmetric wall thickening in the cecum, hepatic lesions, and an enhancing right mesentery lymph node. Given concerns for malignancy, general surgery was consulted who requested gastroenterology’s input prior to surgical intervention. Colonoscopy revealed large patchy ulceration in the cecum and smaller ulcerations in the ascending colon. Biopsies showed ulcerated mucosa with acute inflammation and reactive epithelial changes, negative for dysplasia or malignancy. Infectious disease was consulted, and the workup—including blood cultures, ova and parasite, cryptosporidium antigen, giardia antigen, and E. histolytica antigen—was negative. However, E. histolytica antibody was elevated. The patient underwent IR-guided drainage of liver lesions, yielding 120 ml of "chocolate" fluid which cultured rare gram-negative bacilli. He was started on flagyl and ceftriaxone, and a PICC line was placed for prolonged antibiotic treatment. He was discharged for outpatient follow-up with infectious disease.
Discussion: This report underscores the need to consider E. histolytica in the differential diagnosis, particularly in patients with atypical presentations, no clear risk factors, or inconclusive test results. E. histolytica antigen is often negative in extraintestinal disease despite colonic involvement, as fewer trophozoites are shed into the colon as the infection progresses to the liver, lowering antigen sensitivity. Even in low-prevalence areas like the U.S., a broad differential is crucial in patients with intermittent fevers and liver lesions.
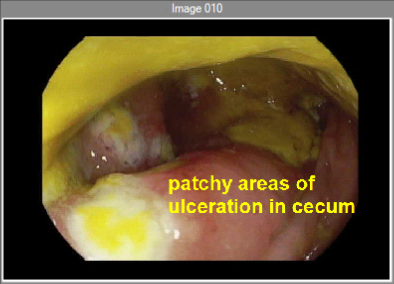
Figure: Patchy areas of ulceration seen in the cecum
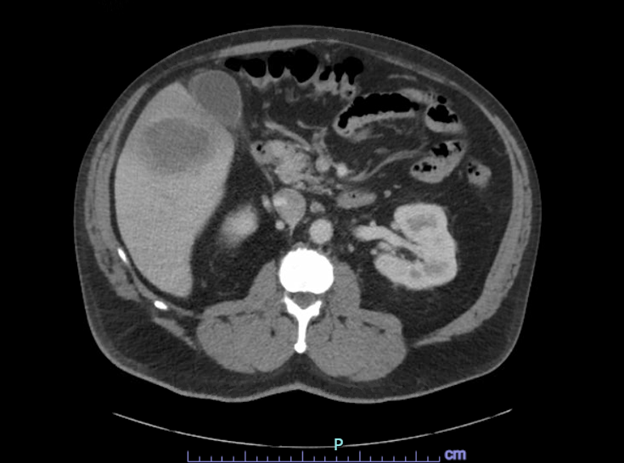
Figure: Liver mass seen on CT of the abdomen and pelvis
Disclosures:
Arvin Razmdideh indicated no relevant financial relationships.
John Martino indicated no relevant financial relationships.
Seth Tatel indicated no relevant financial relationships.
Arvin Razmdideh, DO, John Martino, DO, Seth Tatel, MD. P5639 - When Suspicion Outpaces Confirmation: A Case of Suspected Invasive Entamoeba Histolytica, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
