Tuesday Poster Session
Category: Infections and Microbiome
A Rare Case of Hemorrhagic <i>Clostridioides difficile</i> Colitis
P5638 - A Rare Case of Hemorrhagic Clostridioides difficile Colitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DJ
Danielle Jackson, DO
University of Texas Health East Texas Physicians
Tyler, TX
Presenting Author(s)
Danielle Jackson, DO, Eugene Lee, DO, Bixuan Lin, MD
University of Texas Health East Texas Physicians, Tyler, TX
Introduction: Clostridioides difficile infection (CDI) is a common opportunistic infection that often occurs in the setting of recent antibiotic use or recent hospitalization. Its clinical spectrum ranges from mild diarrhea to fulminant colitis. Here we present a rare case of fulminant hemorrhagic colitis resulting from CDI.
Case Description/
Methods: A 57 year old male with medical history of alcoholic cirrhosis and end stage renal disease was admitted for decompensation by ascites. He had recent antibiotic use due to Serratia bacteremia from a complicated urinary tract infection. Hospital course was complicated by episodes of melena. Esophagogastroduodenoscopy (EGD) revealed a large duodenal bulb ulcer with oozing from a visible vessel, treated with epinephrine and bipolar cautery. Patient continued to require transfusions and then developed hematochezia. Relook EGD now showed clean-based duodenal ulcers. Next, colonoscopy showed exudative hemorrhagic colitis with large amounts of blood clots throughout the colon (Figures 1 and 2). Findings were suspicious for infectious or ischemic etiology. Pathology of colon biopsies were unremarkable, but stool test was positive for C. difficile toxin. The patient was diagnosed with fulminant hemorrhagic C. difficile colitis and treated with antibiotics; the bleeding soon resolved and the patient improved clinically.
Discussion: Dysentery is typically caused by infections such as Shiga toxin producing Escherichia coli or by non-infectious causes such as ischemic colitis. Clostridioides difficile is a common cause of watery diarrhea in adults with endoscopic features of yellow-white pseudomembranes on an erythematous base. However, concurrent hematochezia is rare, with only two case reports available in our research. CDI can lead to hemorrhagic colitis through toxins which disrupt the colonic epithelial barrier, inducing inflammation and barrier breakdown, leading to ulcerations and bleeding. On endoscopy, hemorrhagic colitis presents as patchy mucosal erythema, friability, ulceration and bleeding associated with right sided colonic edema, as seen in our patient. There are limited data on risk factors that increase the incidence of hemorrhagic presentation of C. diff colitis. Patients with cirrhosis and chronic renal disease are at increased risk of having mucosal bleed due to the compounding effect of hemostatic disturbances and platelet dysfunction. It is important to keep a broad differential with hemorrhagic colitis, including typically non-infectious causes.

Figure: Figure 1. Exudative hemorrhagic colitis seen on the right colon.
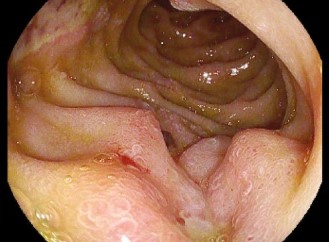
Figure: Figure 2. Exudative colitis seen on the left colon.
Disclosures:
Danielle Jackson indicated no relevant financial relationships.
Eugene Lee indicated no relevant financial relationships.
Bixuan Lin indicated no relevant financial relationships.
Danielle Jackson, DO, Eugene Lee, DO, Bixuan Lin, MD. P5638 - A Rare Case of Hemorrhagic <i>Clostridioides difficile</i> Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Texas Health East Texas Physicians, Tyler, TX
Introduction: Clostridioides difficile infection (CDI) is a common opportunistic infection that often occurs in the setting of recent antibiotic use or recent hospitalization. Its clinical spectrum ranges from mild diarrhea to fulminant colitis. Here we present a rare case of fulminant hemorrhagic colitis resulting from CDI.
Case Description/
Methods: A 57 year old male with medical history of alcoholic cirrhosis and end stage renal disease was admitted for decompensation by ascites. He had recent antibiotic use due to Serratia bacteremia from a complicated urinary tract infection. Hospital course was complicated by episodes of melena. Esophagogastroduodenoscopy (EGD) revealed a large duodenal bulb ulcer with oozing from a visible vessel, treated with epinephrine and bipolar cautery. Patient continued to require transfusions and then developed hematochezia. Relook EGD now showed clean-based duodenal ulcers. Next, colonoscopy showed exudative hemorrhagic colitis with large amounts of blood clots throughout the colon (Figures 1 and 2). Findings were suspicious for infectious or ischemic etiology. Pathology of colon biopsies were unremarkable, but stool test was positive for C. difficile toxin. The patient was diagnosed with fulminant hemorrhagic C. difficile colitis and treated with antibiotics; the bleeding soon resolved and the patient improved clinically.
Discussion: Dysentery is typically caused by infections such as Shiga toxin producing Escherichia coli or by non-infectious causes such as ischemic colitis. Clostridioides difficile is a common cause of watery diarrhea in adults with endoscopic features of yellow-white pseudomembranes on an erythematous base. However, concurrent hematochezia is rare, with only two case reports available in our research. CDI can lead to hemorrhagic colitis through toxins which disrupt the colonic epithelial barrier, inducing inflammation and barrier breakdown, leading to ulcerations and bleeding. On endoscopy, hemorrhagic colitis presents as patchy mucosal erythema, friability, ulceration and bleeding associated with right sided colonic edema, as seen in our patient. There are limited data on risk factors that increase the incidence of hemorrhagic presentation of C. diff colitis. Patients with cirrhosis and chronic renal disease are at increased risk of having mucosal bleed due to the compounding effect of hemostatic disturbances and platelet dysfunction. It is important to keep a broad differential with hemorrhagic colitis, including typically non-infectious causes.

Figure: Figure 1. Exudative hemorrhagic colitis seen on the right colon.
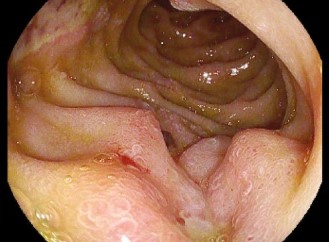
Figure: Figure 2. Exudative colitis seen on the left colon.
Disclosures:
Danielle Jackson indicated no relevant financial relationships.
Eugene Lee indicated no relevant financial relationships.
Bixuan Lin indicated no relevant financial relationships.
Danielle Jackson, DO, Eugene Lee, DO, Bixuan Lin, MD. P5638 - A Rare Case of Hemorrhagic <i>Clostridioides difficile</i> Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
