Tuesday Poster Session
Category: Infections and Microbiome
P5633 - A Candida Copycat: An Unusual Presentation of HSV Esophagitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samuel Levine, MD
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Samuel Levine, MD1, Zarian Prenatt, DO1, Vishal Patel, MD2
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Health Network, Merion Station, PA
Introduction: Esophageal candidiasis typically presents with dysphagia and odynophagia, predominantly affecting immunocompromised patients, those using inhaled corticosteroids, and individuals with risk factors such as diabetes. Diagnosis is confirmed via esophagogastroduodenoscopy (EGD) showing exudates in the esophagus and histopathological examination. Similarly, Herpes Simplex Virus (HSV) esophagitis presents with odynophagia and dysphagia, primarily in immunocompromised patients. Endoscopic findings often reveal multiple circumscribed, shallow ulcers in the distal esophagus, with diagnosis confirmed histologically. Rarely, HSV and Candida infections can occur in immunocompetent patient or appear similar on EGD, complicating the diagnosis.
Case Description/
Methods: A 66-year-old male with a history of atrial fibrillation, thromboembolic strokes, and right hemiparesis, presented with two weeks of esophageal dysphagia and odynophagia with solids and liquids which began immediately after a recent urologic procedure requiring intubation. Computed tomography (CT) of the chest and abdomen revealed diffuse circumferential thickening of the esophagus. He was admitted and started on intravenous proton pump inhibitor (PPI). On exam, he was noted to have white plaque on his tongue suspicious for candidiasis. He underwent EGD which was significant for diffuse white exudate throughout the esophagus and grade D esophagitis involving the lower esophagus, consistent with Candida esophagitis. As a result, the patient was recommended to start fluconazole for candidiasis and continue PPI for his esophagitis. On the day of discharge, pathology results from esophageal brushings indicated viral cytopathic effect consistent with HSV, and no fungal organisms were identified. The patient was subsequently instructed to begin a course of acyclovir for HSV esophagitis.
Discussion: This case highlights the diagnostic challenge posed by overlapping presentations of esophageal candidiasis and HSV esophagitis. EGD with brushing or biopsy is necessary to differentiate between pathologies. The Infectious Diseases Society of America (IDSA) recommends fungal microscopy, Gram stain, and histopathological examination for diagnosing esophageal candidiasis, while HSV esophagitis is best confirmed through histopathology and nucleic acid amplification tests (NAAT). Therefore, accurate diagnosis requires a combination of endoscopic evaluation and histopathological confirmation to guide appropriate treatment.
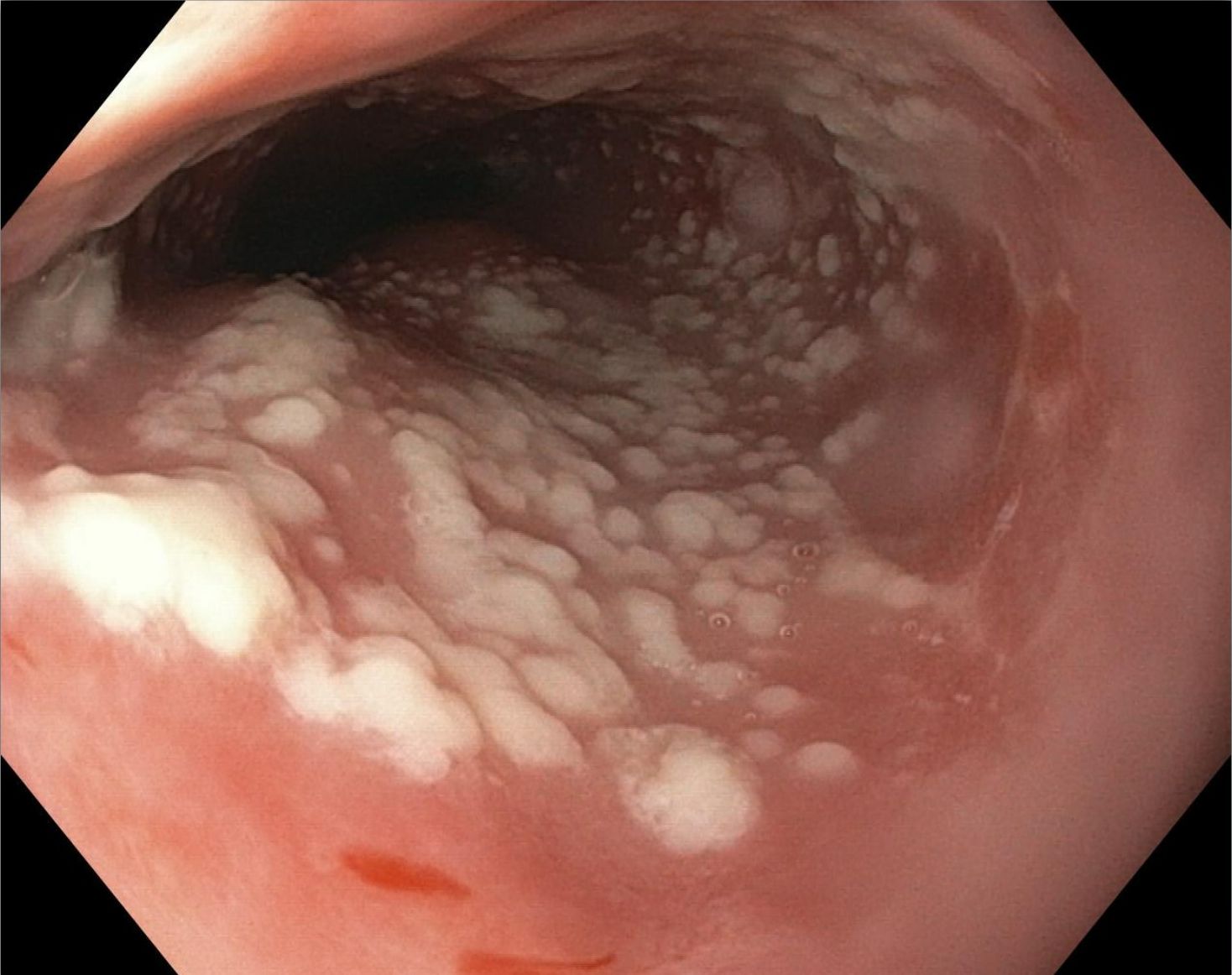
Figure: Diffuse white plaque-like lesions throughout the esophagus
Disclosures:
Samuel Levine indicated no relevant financial relationships.
Zarian Prenatt indicated no relevant financial relationships.
Vishal Patel indicated no relevant financial relationships.
Samuel Levine, MD1, Zarian Prenatt, DO1, Vishal Patel, MD2. P5633 - A <i>Candida</i> Copycat: An Unusual Presentation of HSV Esophagitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Health Network, Merion Station, PA
Introduction: Esophageal candidiasis typically presents with dysphagia and odynophagia, predominantly affecting immunocompromised patients, those using inhaled corticosteroids, and individuals with risk factors such as diabetes. Diagnosis is confirmed via esophagogastroduodenoscopy (EGD) showing exudates in the esophagus and histopathological examination. Similarly, Herpes Simplex Virus (HSV) esophagitis presents with odynophagia and dysphagia, primarily in immunocompromised patients. Endoscopic findings often reveal multiple circumscribed, shallow ulcers in the distal esophagus, with diagnosis confirmed histologically. Rarely, HSV and Candida infections can occur in immunocompetent patient or appear similar on EGD, complicating the diagnosis.
Case Description/
Methods: A 66-year-old male with a history of atrial fibrillation, thromboembolic strokes, and right hemiparesis, presented with two weeks of esophageal dysphagia and odynophagia with solids and liquids which began immediately after a recent urologic procedure requiring intubation. Computed tomography (CT) of the chest and abdomen revealed diffuse circumferential thickening of the esophagus. He was admitted and started on intravenous proton pump inhibitor (PPI). On exam, he was noted to have white plaque on his tongue suspicious for candidiasis. He underwent EGD which was significant for diffuse white exudate throughout the esophagus and grade D esophagitis involving the lower esophagus, consistent with Candida esophagitis. As a result, the patient was recommended to start fluconazole for candidiasis and continue PPI for his esophagitis. On the day of discharge, pathology results from esophageal brushings indicated viral cytopathic effect consistent with HSV, and no fungal organisms were identified. The patient was subsequently instructed to begin a course of acyclovir for HSV esophagitis.
Discussion: This case highlights the diagnostic challenge posed by overlapping presentations of esophageal candidiasis and HSV esophagitis. EGD with brushing or biopsy is necessary to differentiate between pathologies. The Infectious Diseases Society of America (IDSA) recommends fungal microscopy, Gram stain, and histopathological examination for diagnosing esophageal candidiasis, while HSV esophagitis is best confirmed through histopathology and nucleic acid amplification tests (NAAT). Therefore, accurate diagnosis requires a combination of endoscopic evaluation and histopathological confirmation to guide appropriate treatment.
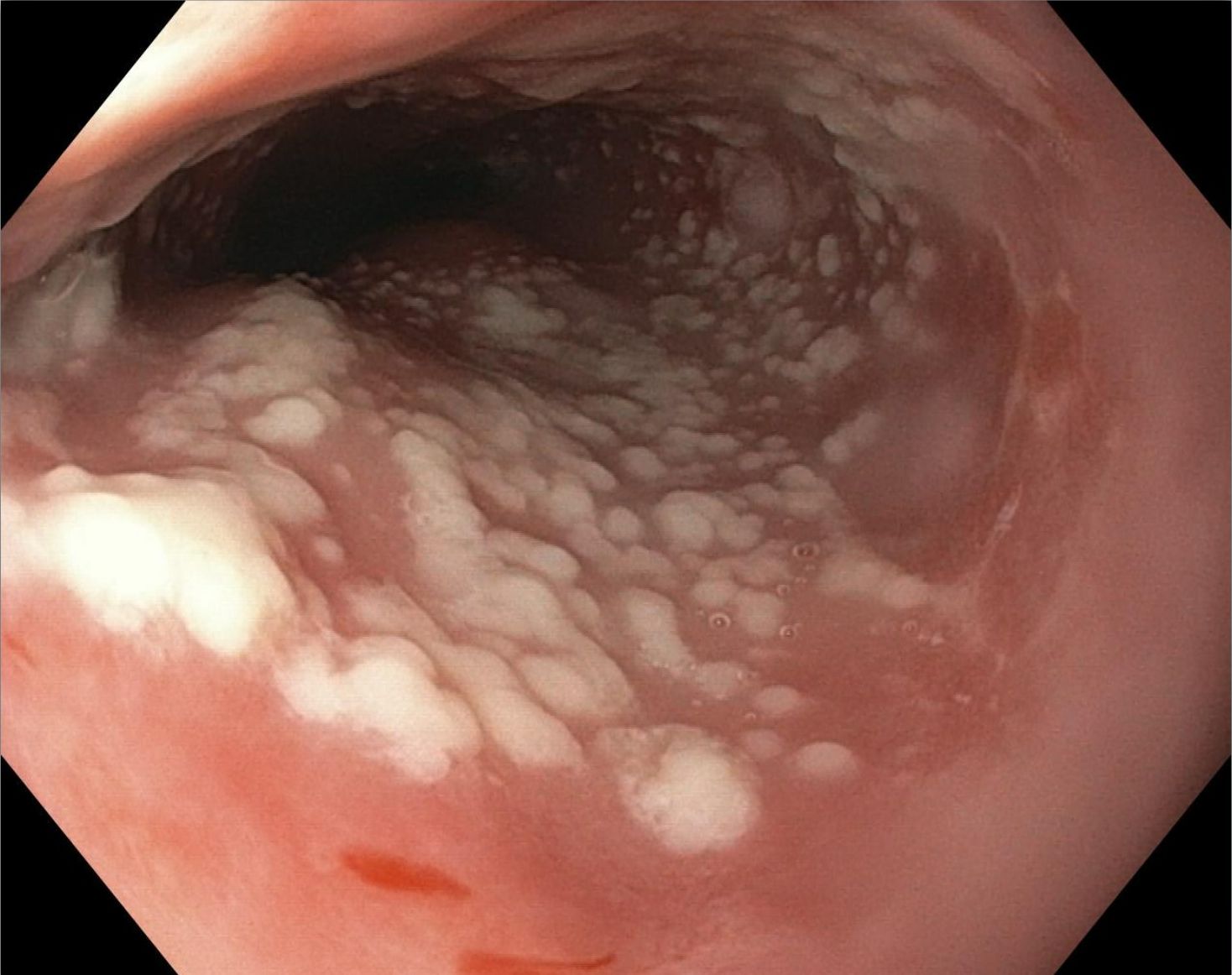
Figure: Diffuse white plaque-like lesions throughout the esophagus
Disclosures:
Samuel Levine indicated no relevant financial relationships.
Zarian Prenatt indicated no relevant financial relationships.
Vishal Patel indicated no relevant financial relationships.
Samuel Levine, MD1, Zarian Prenatt, DO1, Vishal Patel, MD2. P5633 - A <i>Candida</i> Copycat: An Unusual Presentation of HSV Esophagitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

