Tuesday Poster Session
Category: Infections and Microbiome
Entamoeba Histolytica Predisposing Factor for Superimposed Invasive <i>Klebsiella</i> Liver Abscess
P5616 - Entamoeba Histolytica Predisposing Factor for Superimposed Invasive Klebsiella Liver Abscess
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chris Pace, DO (he/him/his)
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
Christopher Pace, DO, Masuma Syed, MD, Christina Joya, DO, Vishvinder Sharma, MD
Valley Hospital Medical Center, Las Vegas, NV
Introduction: Pyogenic liver abscesses (PLAs) are bacterial, commonly caused by Klebsiella pneumoniae in Asian populations, especially in diabetics. Amebic liver abscesses (ALAs), due to Entamoeba histolytica, are endemic in South Asia and usually result from ingesting contaminated food or water. Co-infection is rare, particularly in immunocompetent individuals. We present a rare case of a Klebsiella liver abscess with positive E. histolytica serology.
Case Description/
Methods: 54-year-old man reported two months of poor appetite, night sweats, and 25 kg unintentional weight loss. He had immigrated to the U.S. from India six years earlier, with no subsequent international travel. On admission, resting HR was 104; other vitals were normal. Weight was 55 kg, BMI 20. Labs showed WBC 14.13 × 10⁹/L, Hb 8.3 g/dL, platelets 585 × 10⁹/L, HbA1c 5.9, HIV negative and AFP < 2.2 ng/mL
CT demonstrated gas-containing, ill-defined hypodense liver lesions extending toward the dome. MRI confirmed multiloculated, peripherally enhancing abscesses
Serology was positive for E. histolytica. Aspiration yielded purulent fluid that cultured Klebsiella pneumoniae. He was treated with metronidazole and ceftriaxone for 10 days, then ciprofloxacin for four weeks, with clinical improvement.
Discussion: Concurrent Klebsiella and positive E. histolytica serology suggests either an amebic abscess secondarily infected by bacteria or a PLA with prior amebic exposure. It’s possible parasitic infection alters hepatic defenses, allowing bacterial invasion even in immunocompetent hosts. This patient had no other risk factors for a PLA such diabetes or immunodeficiency. Though the positive serology may have been an incidental finding, the absence of other risk factors makes E. histolytica a plausible contributor.
Treatment of PLA involves Percutaneous drainage which is both diagnostic and therapeutic with concurrent appropriate antibiotic administration. Treatment is typically for 4 - 6 weeks.
Amebic abscesses typically respond to metronidazole, followed by a luminal agent to eradicate intraluminal cysts—even if stool tests are negative. With early diagnosis and appropriate interventions and antibiotics, outcomes for both PLA and ALA are favorable.
This case emphasizes the need to consider both bacterial and parasitic causes of liver abscesses, even with distant exposure and in non-endemic settings.
*Generative AI was used for assistance in editing this case report.*
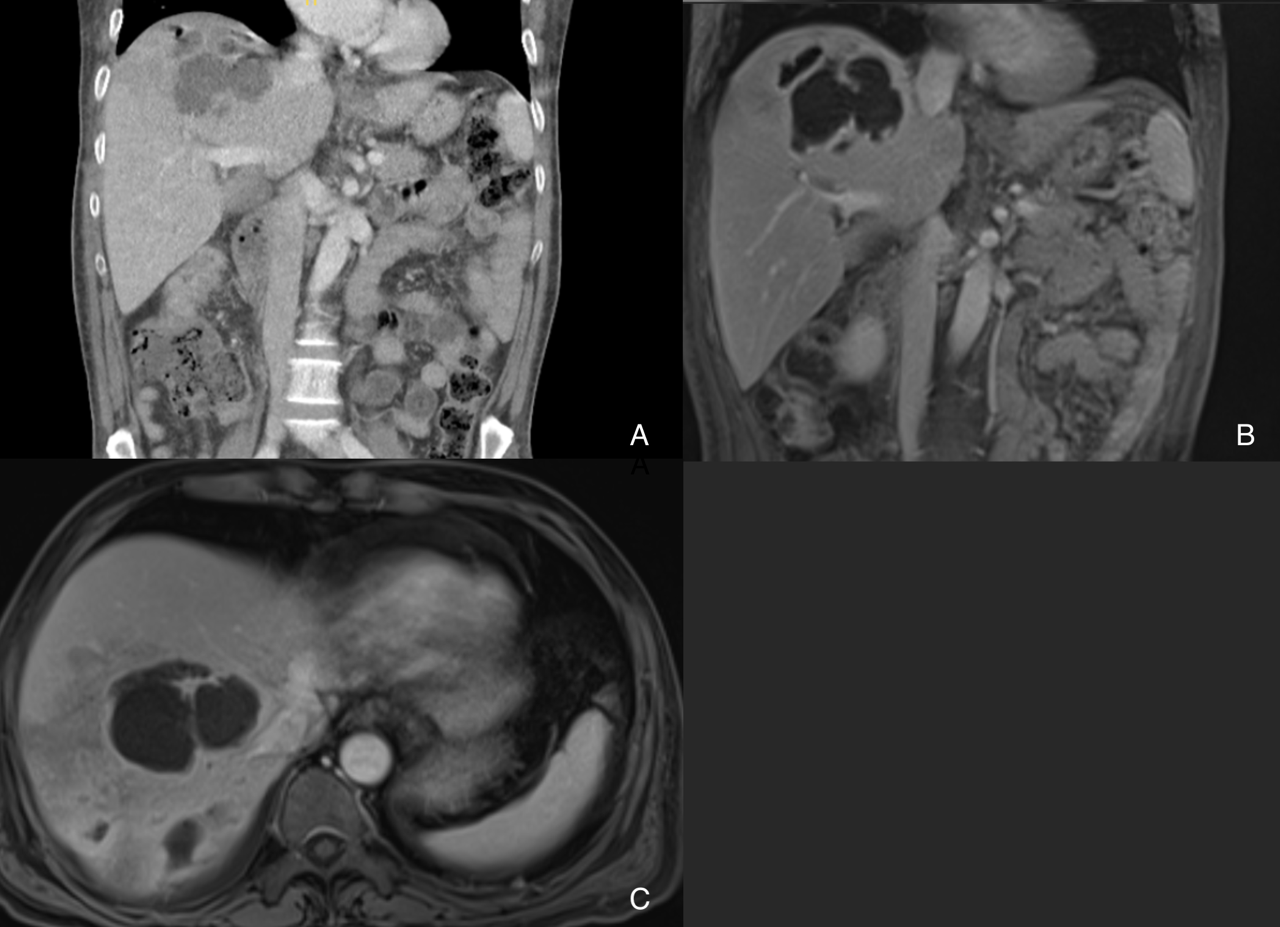
Figure: A: Coronal view CT Abdomen/Pelvis depicting hypodense lesions with gas extending towards the dome of the liver.
B: Coronal view MRI Abdomen showing multiloculated peripherally enhancing structure.
C: Axial View MRI Abdomen again showing multiloculated peripherally enhancing structure.
Disclosures:
Christopher Pace indicated no relevant financial relationships.
Masuma Syed indicated no relevant financial relationships.
Christina Joya indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Christopher Pace, DO, Masuma Syed, MD, Christina Joya, DO, Vishvinder Sharma, MD. P5616 - Entamoeba Histolytica Predisposing Factor for Superimposed Invasive <i>Klebsiella</i> Liver Abscess, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Valley Hospital Medical Center, Las Vegas, NV
Introduction: Pyogenic liver abscesses (PLAs) are bacterial, commonly caused by Klebsiella pneumoniae in Asian populations, especially in diabetics. Amebic liver abscesses (ALAs), due to Entamoeba histolytica, are endemic in South Asia and usually result from ingesting contaminated food or water. Co-infection is rare, particularly in immunocompetent individuals. We present a rare case of a Klebsiella liver abscess with positive E. histolytica serology.
Case Description/
Methods: 54-year-old man reported two months of poor appetite, night sweats, and 25 kg unintentional weight loss. He had immigrated to the U.S. from India six years earlier, with no subsequent international travel. On admission, resting HR was 104; other vitals were normal. Weight was 55 kg, BMI 20. Labs showed WBC 14.13 × 10⁹/L, Hb 8.3 g/dL, platelets 585 × 10⁹/L, HbA1c 5.9, HIV negative and AFP < 2.2 ng/mL
CT demonstrated gas-containing, ill-defined hypodense liver lesions extending toward the dome. MRI confirmed multiloculated, peripherally enhancing abscesses
Serology was positive for E. histolytica. Aspiration yielded purulent fluid that cultured Klebsiella pneumoniae. He was treated with metronidazole and ceftriaxone for 10 days, then ciprofloxacin for four weeks, with clinical improvement.
Discussion: Concurrent Klebsiella and positive E. histolytica serology suggests either an amebic abscess secondarily infected by bacteria or a PLA with prior amebic exposure. It’s possible parasitic infection alters hepatic defenses, allowing bacterial invasion even in immunocompetent hosts. This patient had no other risk factors for a PLA such diabetes or immunodeficiency. Though the positive serology may have been an incidental finding, the absence of other risk factors makes E. histolytica a plausible contributor.
Treatment of PLA involves Percutaneous drainage which is both diagnostic and therapeutic with concurrent appropriate antibiotic administration. Treatment is typically for 4 - 6 weeks.
Amebic abscesses typically respond to metronidazole, followed by a luminal agent to eradicate intraluminal cysts—even if stool tests are negative. With early diagnosis and appropriate interventions and antibiotics, outcomes for both PLA and ALA are favorable.
This case emphasizes the need to consider both bacterial and parasitic causes of liver abscesses, even with distant exposure and in non-endemic settings.
*Generative AI was used for assistance in editing this case report.*
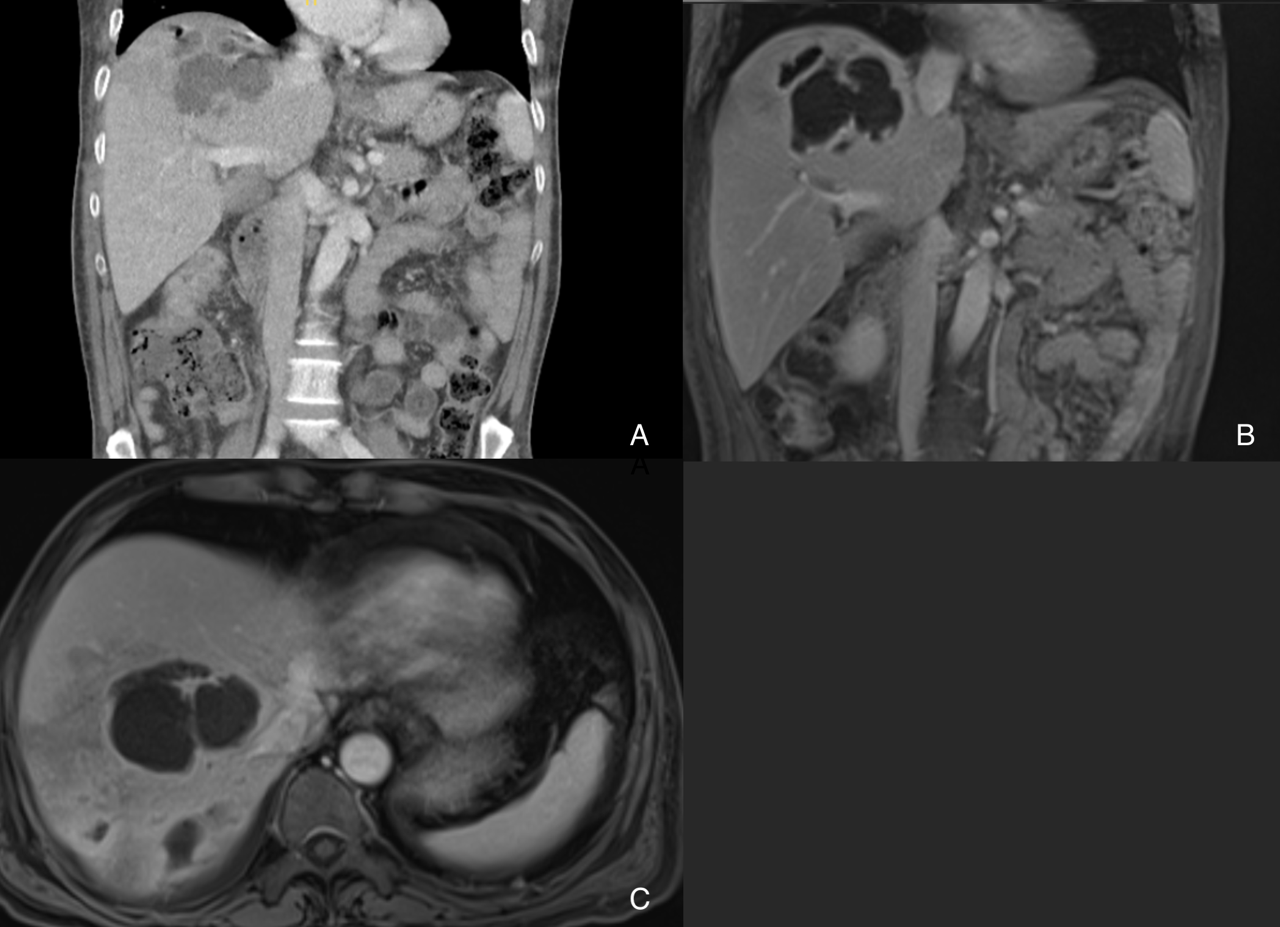
Figure: A: Coronal view CT Abdomen/Pelvis depicting hypodense lesions with gas extending towards the dome of the liver.
B: Coronal view MRI Abdomen showing multiloculated peripherally enhancing structure.
C: Axial View MRI Abdomen again showing multiloculated peripherally enhancing structure.
Disclosures:
Christopher Pace indicated no relevant financial relationships.
Masuma Syed indicated no relevant financial relationships.
Christina Joya indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Christopher Pace, DO, Masuma Syed, MD, Christina Joya, DO, Vishvinder Sharma, MD. P5616 - Entamoeba Histolytica Predisposing Factor for Superimposed Invasive <i>Klebsiella</i> Liver Abscess, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
