Tuesday Poster Session
Category: Infections and Microbiome
P5611 - Chronic Unexplained Anemia: The First Clue to Tuberculous Granulomatous Colitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rhett Harmon, MD (he/him/his)
Olive View-UCLA Medical Center
Los Angeles, CA
Presenting Author(s)
Rhett Harmon, MD1, Payman Fathizadeh, MD2, Aidas Mattis, MD2, Lisa Toy, MD2, Daniel Cole, MD, MPH1, Glenn Mathisen, MD2, Sherif Shoucri, MD2, Shaun Chandna, DO2
1Olive View-UCLA Medical Center, Los Angeles, CA; 2Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Gastrointestinal (GI) tuberculosis (TB) is an uncommon form of Mycobacterium tuberculosis infection that frequently presents with symptoms similar to inflammatory bowel disease (IBD) or malignancy. 15% of extrapulmonary TB cases involve the GI tract, predominantly affecting the ileocecal region and ascending colon. GI TB can be difficult to diagnose when presenting with exclusively hematologic abnormalities rather than pulmonary or abdominal symptoms. Anemia is a frequent occurrence in TB patients, with nearly 60% having anemia of chronic disease.
Case Description/
Methods: A 51-year-old woman with diabetes presented for an evaluation of ongoing normocytic anemia. Her hemoglobin (Hb) was stable at 9.4 g/dL for 10 months. She denied respiratory or gastrointestinal symptoms. Despite extensive hematologic evaluation including a bone marrow biopsy, no significant abnormalities were found. A colonoscopy was subsequently pursued, revealing a 2 cm ulcerated cecal lesion with non-necrotizing granulomatous colitis on pathology, with stains negative for acid-fast bacilli (AFB) and fungi. Follow up stool AFB cultures were negative, though QuantiFERON-Gold testing was noted to be positive. Chest imaging showed clear lungs. Repeat colonoscopy with biopsy of cecal ulcer, culture, and specialized testing was performed. MTB PCR returned negative from tissue; however, MTB complex DNA was detected on ls6110 primer set next-generation sequencing (NGS). Growth of MTB from biopsy AFB cultures further confirmed tuberculosis infection. The patient was subsequently started on TB treatment and reported to the local TB control program for outpatient monitoring.
Discussion: Our case of GI TB highlights the importance of considering endoscopic evaluation in anemia of unclear etiology, especially after a negative hematologic work up. Anemia in GI TB can result from chronic inflammation, malabsorption, and occult GI blood loss. TB colitis can be a diagnostic challenge due to its nonspecific, mimicking endoscopic and histologic features for IBD. Although colonic biopsies have low sensitivity for caseating granulomas or AFB detection, GI TB should be considered in the differential of granulomatous colitis on endoscopy. If suspicion is raised (endemicity, immunocompromise, serology or other testing), and initial biopsy and cultures are unrevealing, repeat colonoscopy with biopsy and culture should be performed with the addition of NGS testing that may further facilitate the timely detection of GI TB.
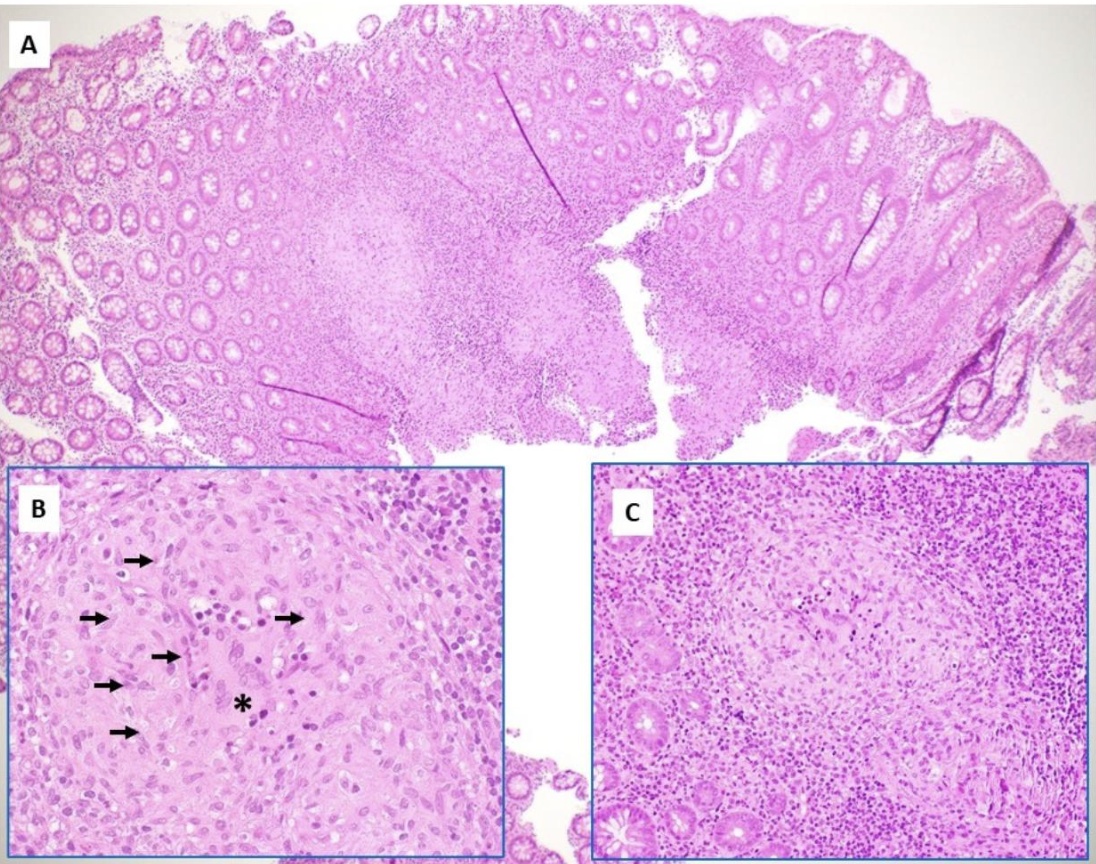
Figure: Colonic biopsies demonstrate mucosa with a non-necrotizing granulomatous inflammatory reaction (A). The granulomatous inflammation is characterized by chronic inflammatory infiltrate composed of epithelioid histiocytes (arrow), multinucleated giant cells (asterisk), and lymphocytes (C) without evidence of necrosis. Special stains for fungal organisms (GMS, PAS-D) and acid-fast bacilli (AFB) failed to identify any infectious microorganisms.

Figure: 2 cm cecal ulcer 1 cm proximal to ileocecal valve
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Payman Fathizadeh indicated no relevant financial relationships.
Aidas Mattis indicated no relevant financial relationships.
Lisa Toy indicated no relevant financial relationships.
Daniel Cole indicated no relevant financial relationships.
Glenn Mathisen indicated no relevant financial relationships.
Sherif Shoucri indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Rhett Harmon, MD1, Payman Fathizadeh, MD2, Aidas Mattis, MD2, Lisa Toy, MD2, Daniel Cole, MD, MPH1, Glenn Mathisen, MD2, Sherif Shoucri, MD2, Shaun Chandna, DO2. P5611 - Chronic Unexplained Anemia: The First Clue to Tuberculous Granulomatous Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Olive View-UCLA Medical Center, Los Angeles, CA; 2Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Gastrointestinal (GI) tuberculosis (TB) is an uncommon form of Mycobacterium tuberculosis infection that frequently presents with symptoms similar to inflammatory bowel disease (IBD) or malignancy. 15% of extrapulmonary TB cases involve the GI tract, predominantly affecting the ileocecal region and ascending colon. GI TB can be difficult to diagnose when presenting with exclusively hematologic abnormalities rather than pulmonary or abdominal symptoms. Anemia is a frequent occurrence in TB patients, with nearly 60% having anemia of chronic disease.
Case Description/
Methods: A 51-year-old woman with diabetes presented for an evaluation of ongoing normocytic anemia. Her hemoglobin (Hb) was stable at 9.4 g/dL for 10 months. She denied respiratory or gastrointestinal symptoms. Despite extensive hematologic evaluation including a bone marrow biopsy, no significant abnormalities were found. A colonoscopy was subsequently pursued, revealing a 2 cm ulcerated cecal lesion with non-necrotizing granulomatous colitis on pathology, with stains negative for acid-fast bacilli (AFB) and fungi. Follow up stool AFB cultures were negative, though QuantiFERON-Gold testing was noted to be positive. Chest imaging showed clear lungs. Repeat colonoscopy with biopsy of cecal ulcer, culture, and specialized testing was performed. MTB PCR returned negative from tissue; however, MTB complex DNA was detected on ls6110 primer set next-generation sequencing (NGS). Growth of MTB from biopsy AFB cultures further confirmed tuberculosis infection. The patient was subsequently started on TB treatment and reported to the local TB control program for outpatient monitoring.
Discussion: Our case of GI TB highlights the importance of considering endoscopic evaluation in anemia of unclear etiology, especially after a negative hematologic work up. Anemia in GI TB can result from chronic inflammation, malabsorption, and occult GI blood loss. TB colitis can be a diagnostic challenge due to its nonspecific, mimicking endoscopic and histologic features for IBD. Although colonic biopsies have low sensitivity for caseating granulomas or AFB detection, GI TB should be considered in the differential of granulomatous colitis on endoscopy. If suspicion is raised (endemicity, immunocompromise, serology or other testing), and initial biopsy and cultures are unrevealing, repeat colonoscopy with biopsy and culture should be performed with the addition of NGS testing that may further facilitate the timely detection of GI TB.
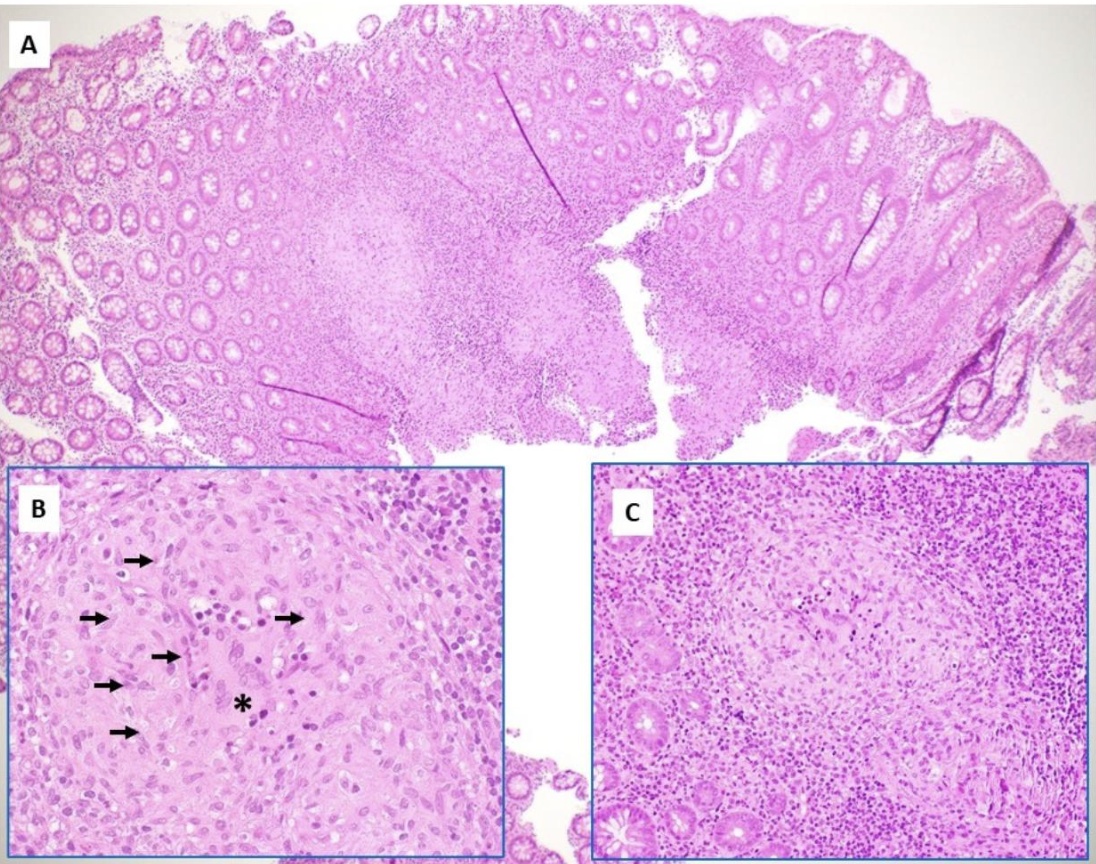
Figure: Colonic biopsies demonstrate mucosa with a non-necrotizing granulomatous inflammatory reaction (A). The granulomatous inflammation is characterized by chronic inflammatory infiltrate composed of epithelioid histiocytes (arrow), multinucleated giant cells (asterisk), and lymphocytes (C) without evidence of necrosis. Special stains for fungal organisms (GMS, PAS-D) and acid-fast bacilli (AFB) failed to identify any infectious microorganisms.

Figure: 2 cm cecal ulcer 1 cm proximal to ileocecal valve
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Payman Fathizadeh indicated no relevant financial relationships.
Aidas Mattis indicated no relevant financial relationships.
Lisa Toy indicated no relevant financial relationships.
Daniel Cole indicated no relevant financial relationships.
Glenn Mathisen indicated no relevant financial relationships.
Sherif Shoucri indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Rhett Harmon, MD1, Payman Fathizadeh, MD2, Aidas Mattis, MD2, Lisa Toy, MD2, Daniel Cole, MD, MPH1, Glenn Mathisen, MD2, Sherif Shoucri, MD2, Shaun Chandna, DO2. P5611 - Chronic Unexplained Anemia: The First Clue to Tuberculous Granulomatous Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
