Tuesday Poster Session
Category: Infections and Microbiome
P5605 - A Wormy Surprise: Unmasking Strongyloides in Eosinophilic Colitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
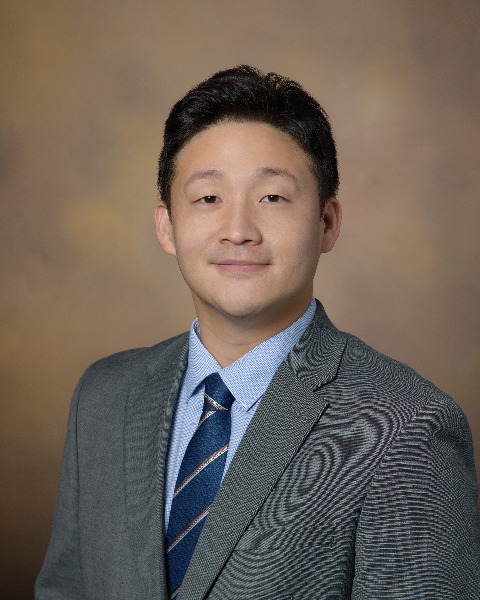
Samuel Cheong, DO
University of Arizona College of Medicine
Tucson, AZ
Presenting Author(s)
Samuel Cheong, DO1, Mohamad Omar Diab, MD2, Sabrina Ho, MD1, Brandon Witten, MD1, Natasha Khona, DO1, Shivanand Bomman, MD1
1Banner - University of Arizona Tucson, Tucson, AZ; 2Canyon Vista Medical Center, Sierra Vista, AZ
Introduction: Eosinophilic Colitis (EoC) is defined as abnormal infiltration of eosinophilic polymorphonuclear cells in the colonic mucosa. Although common in children under two years old, it is rare in adults. EoC is classified as primary and secondary, which is crucial for guiding management. We present a rare case of secondary EoC.
Case Description/
Methods: A 61-year-old male with a history of severe allergies, GERD, and eosinophilic esophagitis was referred by an allergist for oral irritation triggered by various foods.
EGD revealed Barrett’s esophagus, as well as erythematous mucosa in the gastric body, antrum, and duodenum. Biopsies confirmed eosinophilic esophagitis ( >15 eosinophils per high-power field) and were negative for CD117 immunostaining for clustering mast cells. Colonoscopy revealed multiple 1 mm white lesions in the cecum, ascending, and transverse colon (TC), 11 tubular adenomas (< 5 mm), and one sessile serrated lesion with a necrotizing granuloma in the TC. Biopsies throughout the colon revealed background mucosa with marked, patchy mucosal eosinophilia ranging between 150 and >400 eosinophils per HPF. CD117 immunostaining was negative for clustering mast cells. Biopsies of the terminal ileum showed increased lamina propria inflammation. MRI enterography was negative for acute or chronic gastroenteritis.
An infectious workup was positive for Strongyloides IgG antibody, likely the primary culprit of his colonoscopy findings and peripheral eosinophilia. The patient was started on omeprazole 40 mg BID indefinitely and ivermectin. Repeat procedures showed resolution of his infectious colitis.
Discussion: Although not standardized, one proposed criterion for EoC is >40 eosinophils/HPF in at least two colonic segments. Primary EoC is a diagnosis of exclusion, whereas secondary EoC has many etiologies (Table 1). Parasitic infections account for 5 to 10% of cases, most commonly including Strongyloides, pinworms, toxocariasis, schistosomiasis, etc. The diagnostic sensitivity of parasitic infections is poor, hence the need for repeated stool and serological tests. The most common findings on colonoscopy are minute, raised lesions, which are collections of eosinophils surrounding a dead Strongyloides larva (Splendore-Hoeppli phenomenon). These lesions may enlarge and become necrotic (possibly explaining the TC polyp), resulting in ulcerations. Treatment involves anti-helminthic agents rather than immunosuppressants for primary EoC. This case highlights a rare form of EoC due to Strongyloides.
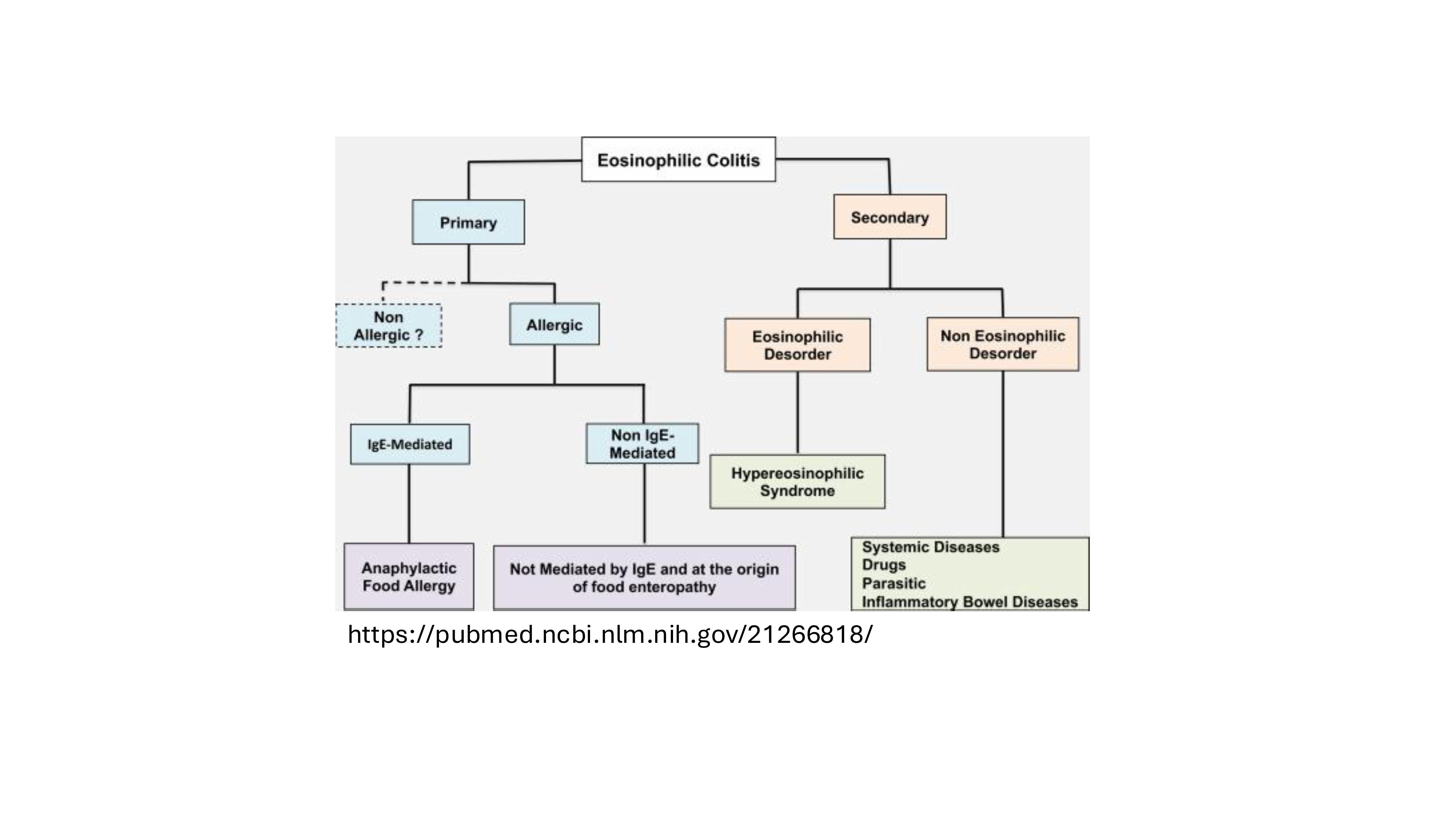
Figure: Figure 1. Classification of eosinophilic colitis into primary and secondary subtypes highlighting associated mechanisms and etiologies.
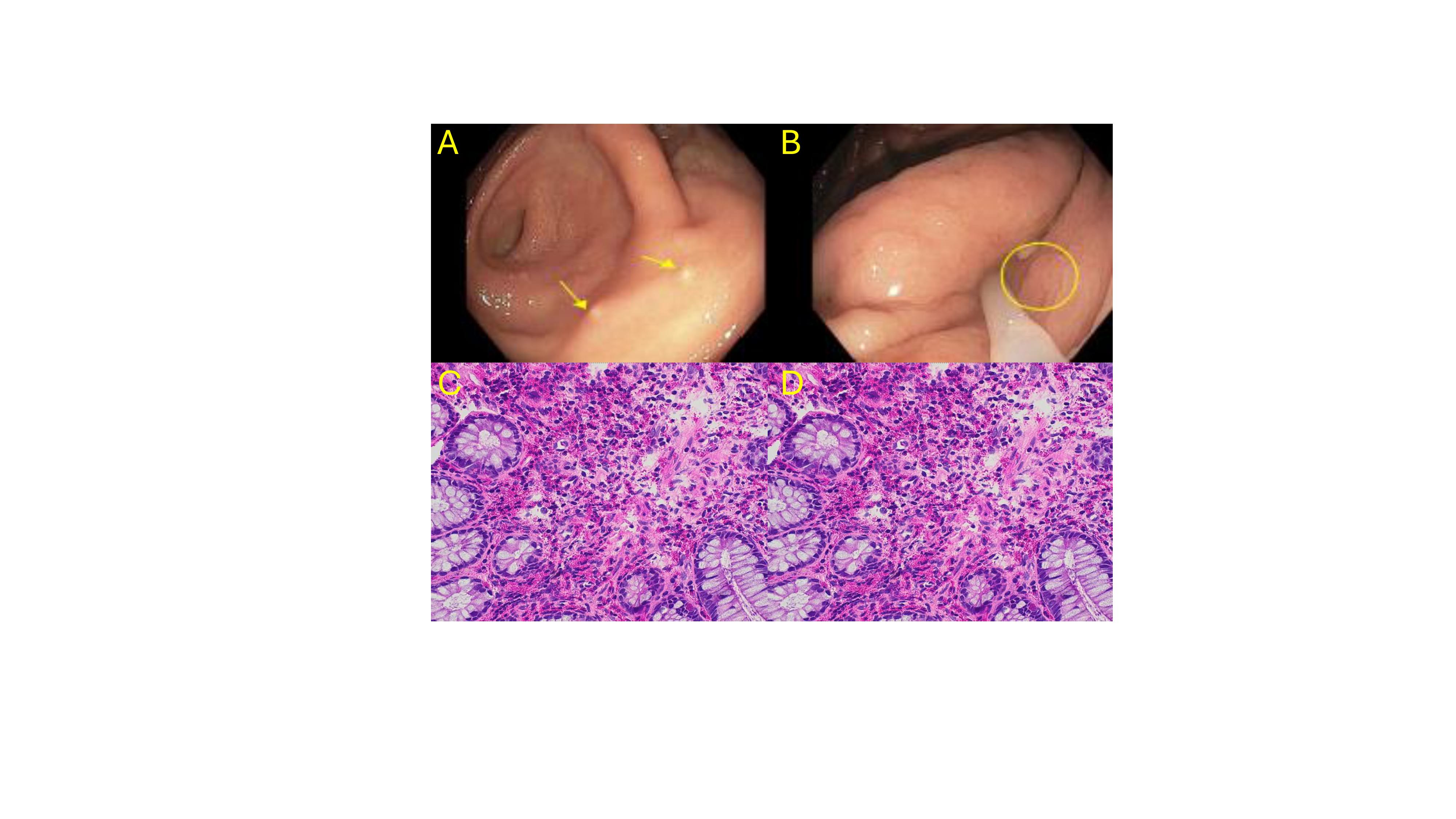
Figure: A, B. Multiple 1 mm white spots noted in the cecum and ascending colon, respectively. C, D. H&E sections of colon biopsies show benign colonic mucosa with a marked lamina propria infiltrate of eosinophils [H&E x200].
Disclosures:
Samuel Cheong indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Sabrina Ho indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Natasha Khona indicated no relevant financial relationships.
Shivanand Bomman indicated no relevant financial relationships.
Samuel Cheong, DO1, Mohamad Omar Diab, MD2, Sabrina Ho, MD1, Brandon Witten, MD1, Natasha Khona, DO1, Shivanand Bomman, MD1. P5605 - A Wormy Surprise: Unmasking Strongyloides in Eosinophilic Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Banner - University of Arizona Tucson, Tucson, AZ; 2Canyon Vista Medical Center, Sierra Vista, AZ
Introduction: Eosinophilic Colitis (EoC) is defined as abnormal infiltration of eosinophilic polymorphonuclear cells in the colonic mucosa. Although common in children under two years old, it is rare in adults. EoC is classified as primary and secondary, which is crucial for guiding management. We present a rare case of secondary EoC.
Case Description/
Methods: A 61-year-old male with a history of severe allergies, GERD, and eosinophilic esophagitis was referred by an allergist for oral irritation triggered by various foods.
EGD revealed Barrett’s esophagus, as well as erythematous mucosa in the gastric body, antrum, and duodenum. Biopsies confirmed eosinophilic esophagitis ( >15 eosinophils per high-power field) and were negative for CD117 immunostaining for clustering mast cells. Colonoscopy revealed multiple 1 mm white lesions in the cecum, ascending, and transverse colon (TC), 11 tubular adenomas (< 5 mm), and one sessile serrated lesion with a necrotizing granuloma in the TC. Biopsies throughout the colon revealed background mucosa with marked, patchy mucosal eosinophilia ranging between 150 and >400 eosinophils per HPF. CD117 immunostaining was negative for clustering mast cells. Biopsies of the terminal ileum showed increased lamina propria inflammation. MRI enterography was negative for acute or chronic gastroenteritis.
An infectious workup was positive for Strongyloides IgG antibody, likely the primary culprit of his colonoscopy findings and peripheral eosinophilia. The patient was started on omeprazole 40 mg BID indefinitely and ivermectin. Repeat procedures showed resolution of his infectious colitis.
Discussion: Although not standardized, one proposed criterion for EoC is >40 eosinophils/HPF in at least two colonic segments. Primary EoC is a diagnosis of exclusion, whereas secondary EoC has many etiologies (Table 1). Parasitic infections account for 5 to 10% of cases, most commonly including Strongyloides, pinworms, toxocariasis, schistosomiasis, etc. The diagnostic sensitivity of parasitic infections is poor, hence the need for repeated stool and serological tests. The most common findings on colonoscopy are minute, raised lesions, which are collections of eosinophils surrounding a dead Strongyloides larva (Splendore-Hoeppli phenomenon). These lesions may enlarge and become necrotic (possibly explaining the TC polyp), resulting in ulcerations. Treatment involves anti-helminthic agents rather than immunosuppressants for primary EoC. This case highlights a rare form of EoC due to Strongyloides.
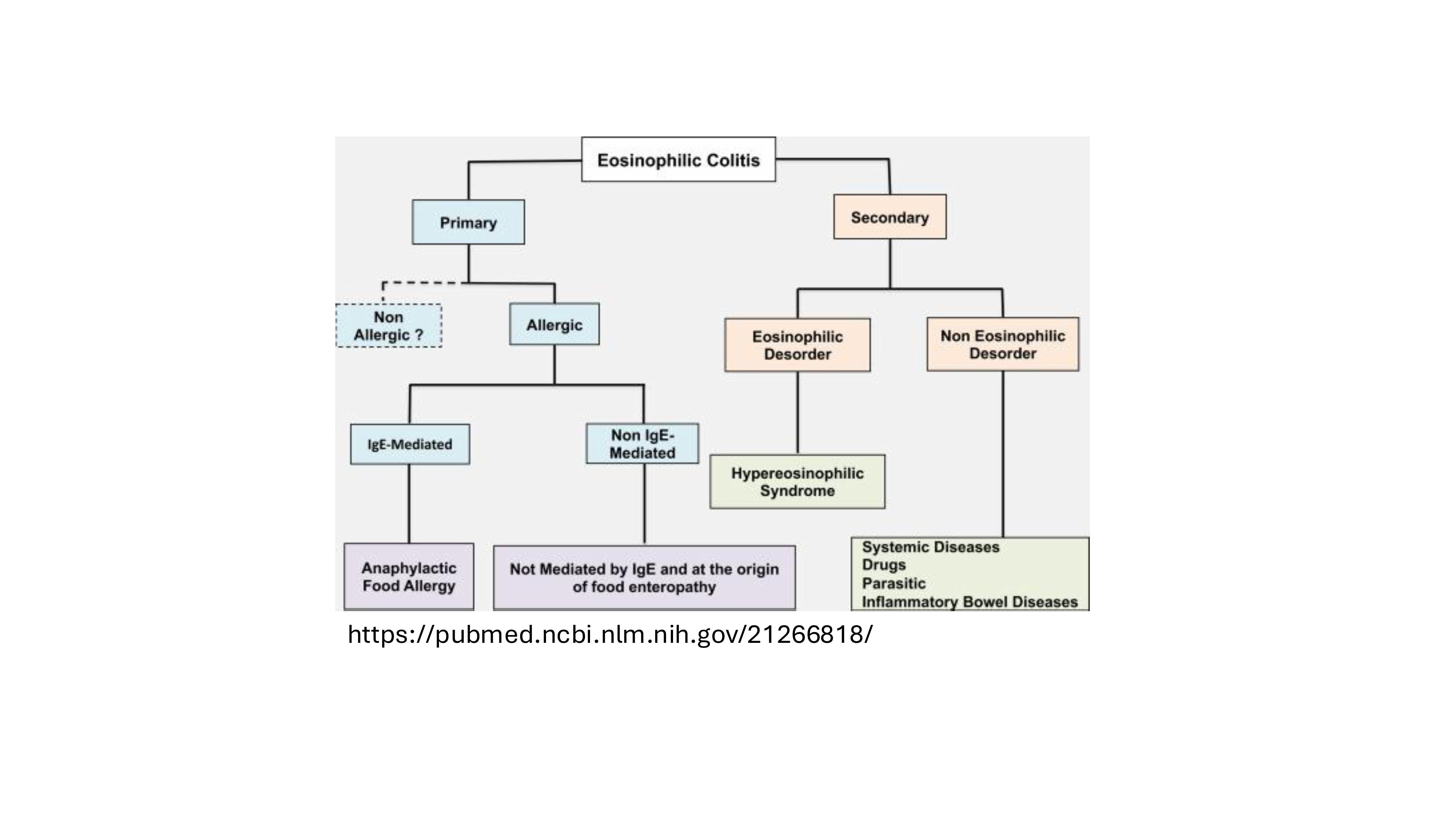
Figure: Figure 1. Classification of eosinophilic colitis into primary and secondary subtypes highlighting associated mechanisms and etiologies.
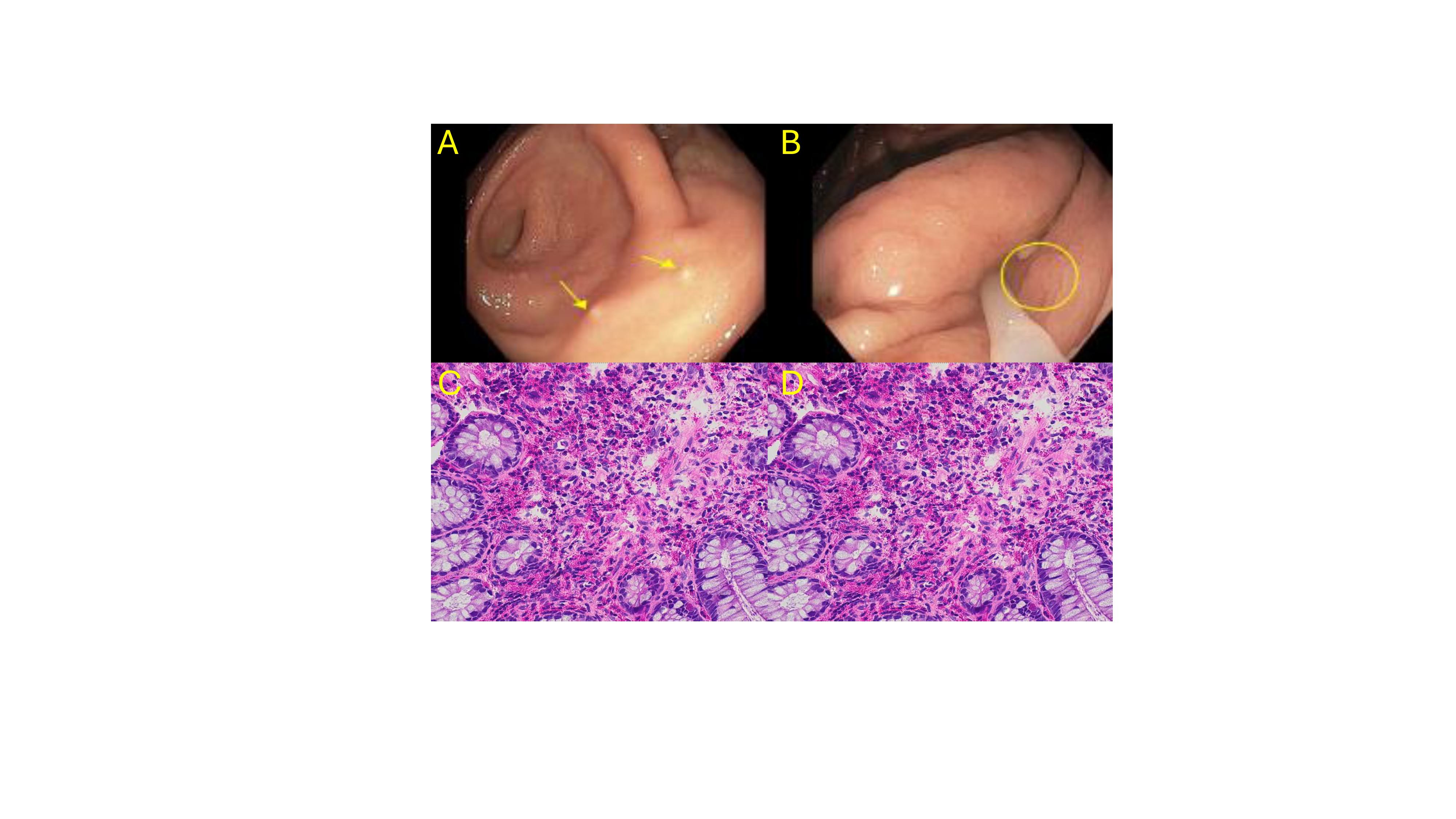
Figure: A, B. Multiple 1 mm white spots noted in the cecum and ascending colon, respectively. C, D. H&E sections of colon biopsies show benign colonic mucosa with a marked lamina propria infiltrate of eosinophils [H&E x200].
Disclosures:
Samuel Cheong indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Sabrina Ho indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Natasha Khona indicated no relevant financial relationships.
Shivanand Bomman indicated no relevant financial relationships.
Samuel Cheong, DO1, Mohamad Omar Diab, MD2, Sabrina Ho, MD1, Brandon Witten, MD1, Natasha Khona, DO1, Shivanand Bomman, MD1. P5605 - A Wormy Surprise: Unmasking Strongyloides in Eosinophilic Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
