Tuesday Poster Session
Category: Infections and Microbiome
P5598 - When Histoplasma Hides: Dissemination Histoplasmosis With Gastric Involvement in an Immunocompetent Patient After 8 Years of Latency
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sharifeh Almasaid, MD, MPH (she/her/hers)
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Sharifeh Almasaid, MD, MPH1, Abdelkader Chaar, MD1, Oleksandr Kravtsov, MD2, Idan Goren, MD1, Ganesh Aswath, MD2
1SUNY Upstate Medical University, Syracuse, NY; 2SUNY Upstate Medical University Hospital, Syracuse, NY
Introduction: Histoplasmosis is a fungal infection endemic to the Ohio and Mississippi River valleys, primarily affecting the lungs via inhaled spores. It’s often mild or asymptomatic in immunocompetent individuals but can be life-threatening. When disseminated, it frequently involves the GI tract, especially the ileum and colon, due to lymphoid tissue abundance. Gastric involvement is rare but can mimic ulcers or cancer, delaying diagnosis. We report a case of recurrent disseminated histoplasmosis with gastric involvement in a patient with odynophagia in a non-endemic area
Case Description/
Methods: A 71-year-old man with prior tonsillar histoplasmosis treated 8 years ago with 12 weeks of itraconazole and confirmed resolution presented with 2 weeks of progressive odynophagia (worse with solids), oral ulcers, abdominal pain, and 30-pound weight loss over 6 months. He denied dysphagia, nausea, vomiting, and melena. No history of malignancy, autoimmune diseases, steroids use or recent travel. Vitals were stable. Labs showed normocytic anemia (Hb 6.7 g/dL, MCV 92.7) without leukocytosis or thrombocytopenia. Kidney and liver functions were normal. Infectious workup, including HIV and tick-borne diseases, was negative. Computerized tomography of the chest showed tree-in-bud centrilobular nodules with upper lobe predominance. Abdominal imaging was unremarkable. Esophagogastroduodenoscopy (EGD) done to evaluate his odynophagia, revealing multiple gastric ulcers with overlying eschar, the largest being 40 mm in diameter. Biopsies showed chronic gastritis with ulceration and fungal yeasts consistent with Histoplasma, confirmed by Grocott's methenamine silver stain. Similarly, oral ulcer biopsy showed non-necrotizing granulomas with fungal forms. He was started on itraconazole and was discharged in stable condition. Follow-up EGD one month later showed healing ulcers.
Discussion: Disseminated histoplasmosis involving the GI tract is common, typically seen in immunocompromised patients. Recurrence may occur due to fungus' ability to persist within macrophages but is extremely rare in immunocompetent individuals. To our knowledge, this is the first reported case of recurrent gastric involvement in an immunocompetent patient from a non-endemic area. This case underscores the need for high clinical suspicion and prompt histopathological evaluation when ulcers are found on endoscopy, even in immunocompetent individuals, to ensure timely diagnosis and optimal outcomes.
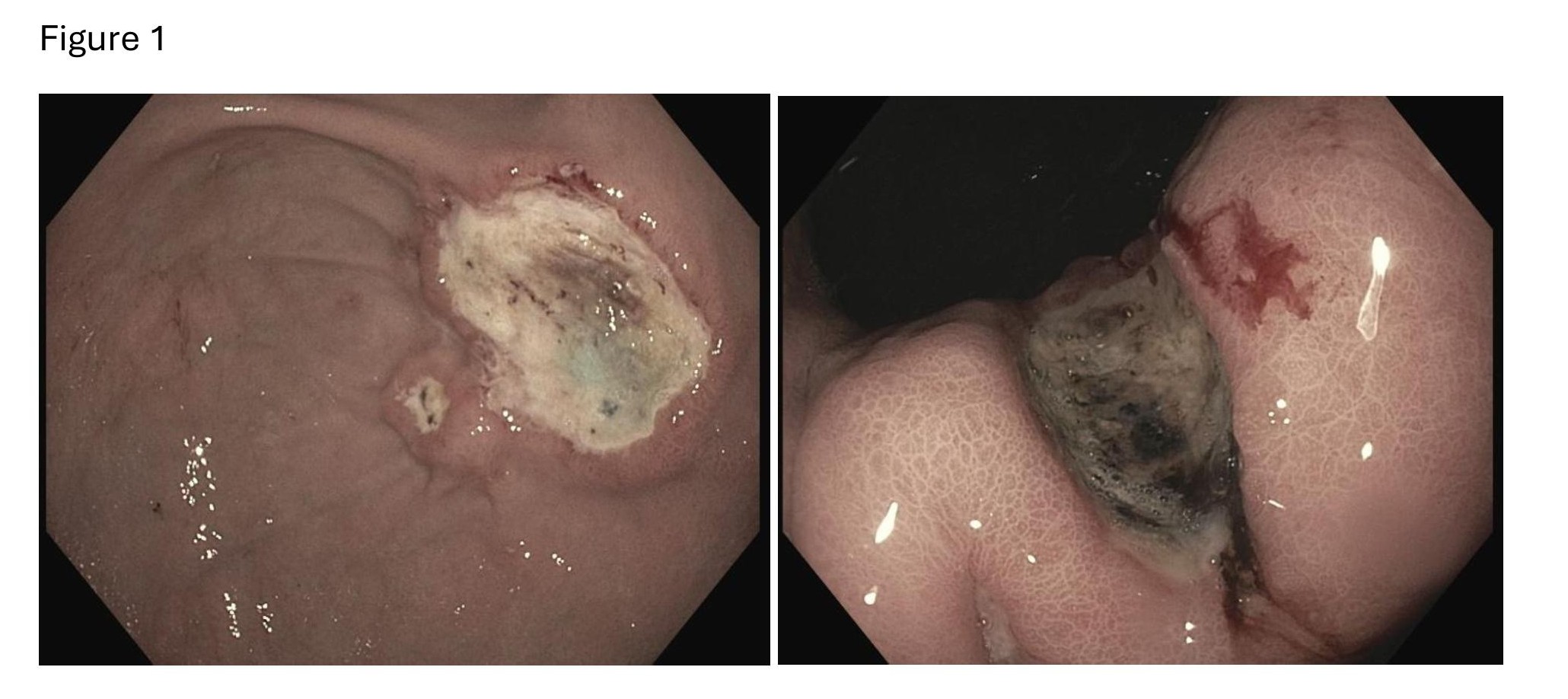
Figure: Gastric ulcers seen on endoscopy
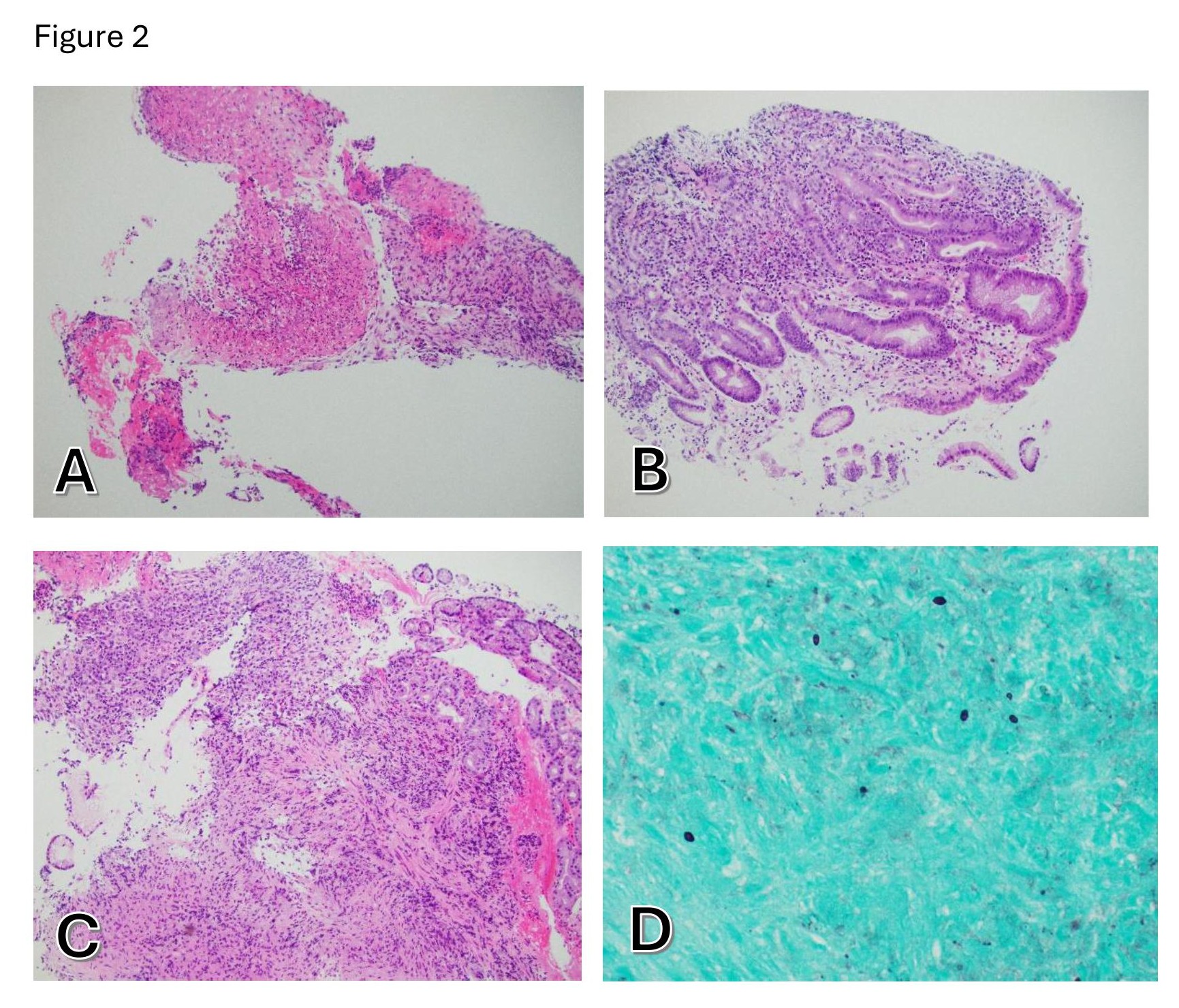
Figure: A: Granulation tissue and fibrin with polymorphonuclear inflammatory infiltration, H&E stain, 100x magnification.
B: Gastric mucosa with active chronic inflammation and regenerative epithelial changes, H&E stain, 100x magnification.
C: Gastric mucosa and granulation tissue with active chronic inflammation, H&E stain, 100x magnification.
D: 2-4 μm in size ovoid yeast with thin non-refractive cell walls and narrow bases, GMS stain, 600x magnification.
Disclosures:
Sharifeh Almasaid indicated no relevant financial relationships.
Abdelkader Chaar indicated no relevant financial relationships.
Oleksandr Kravtsov indicated no relevant financial relationships.
Idan Goren indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Sharifeh Almasaid, MD, MPH1, Abdelkader Chaar, MD1, Oleksandr Kravtsov, MD2, Idan Goren, MD1, Ganesh Aswath, MD2. P5598 - When Histoplasma Hides: Dissemination Histoplasmosis With Gastric Involvement in an Immunocompetent Patient After 8 Years of Latency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University, Syracuse, NY; 2SUNY Upstate Medical University Hospital, Syracuse, NY
Introduction: Histoplasmosis is a fungal infection endemic to the Ohio and Mississippi River valleys, primarily affecting the lungs via inhaled spores. It’s often mild or asymptomatic in immunocompetent individuals but can be life-threatening. When disseminated, it frequently involves the GI tract, especially the ileum and colon, due to lymphoid tissue abundance. Gastric involvement is rare but can mimic ulcers or cancer, delaying diagnosis. We report a case of recurrent disseminated histoplasmosis with gastric involvement in a patient with odynophagia in a non-endemic area
Case Description/
Methods: A 71-year-old man with prior tonsillar histoplasmosis treated 8 years ago with 12 weeks of itraconazole and confirmed resolution presented with 2 weeks of progressive odynophagia (worse with solids), oral ulcers, abdominal pain, and 30-pound weight loss over 6 months. He denied dysphagia, nausea, vomiting, and melena. No history of malignancy, autoimmune diseases, steroids use or recent travel. Vitals were stable. Labs showed normocytic anemia (Hb 6.7 g/dL, MCV 92.7) without leukocytosis or thrombocytopenia. Kidney and liver functions were normal. Infectious workup, including HIV and tick-borne diseases, was negative. Computerized tomography of the chest showed tree-in-bud centrilobular nodules with upper lobe predominance. Abdominal imaging was unremarkable. Esophagogastroduodenoscopy (EGD) done to evaluate his odynophagia, revealing multiple gastric ulcers with overlying eschar, the largest being 40 mm in diameter. Biopsies showed chronic gastritis with ulceration and fungal yeasts consistent with Histoplasma, confirmed by Grocott's methenamine silver stain. Similarly, oral ulcer biopsy showed non-necrotizing granulomas with fungal forms. He was started on itraconazole and was discharged in stable condition. Follow-up EGD one month later showed healing ulcers.
Discussion: Disseminated histoplasmosis involving the GI tract is common, typically seen in immunocompromised patients. Recurrence may occur due to fungus' ability to persist within macrophages but is extremely rare in immunocompetent individuals. To our knowledge, this is the first reported case of recurrent gastric involvement in an immunocompetent patient from a non-endemic area. This case underscores the need for high clinical suspicion and prompt histopathological evaluation when ulcers are found on endoscopy, even in immunocompetent individuals, to ensure timely diagnosis and optimal outcomes.
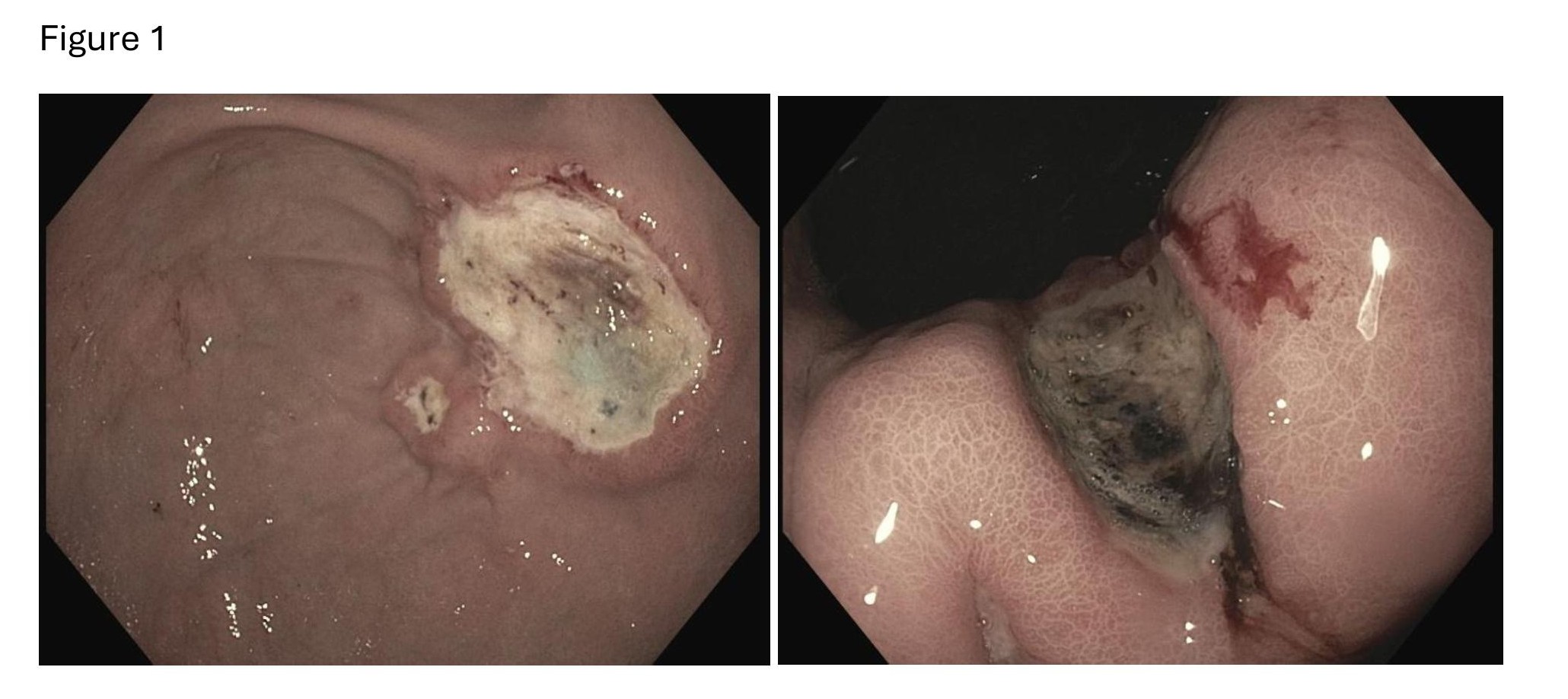
Figure: Gastric ulcers seen on endoscopy
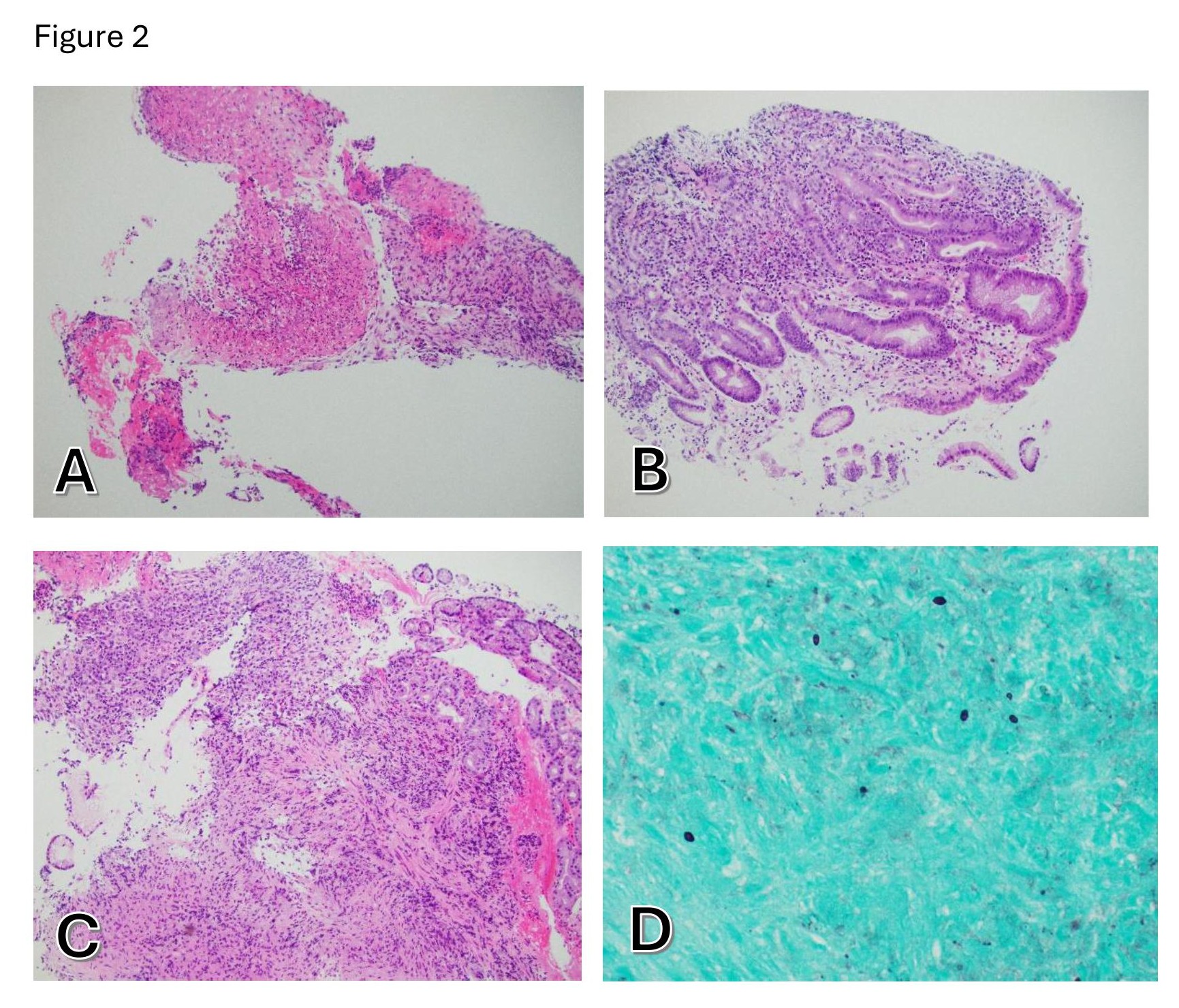
Figure: A: Granulation tissue and fibrin with polymorphonuclear inflammatory infiltration, H&E stain, 100x magnification.
B: Gastric mucosa with active chronic inflammation and regenerative epithelial changes, H&E stain, 100x magnification.
C: Gastric mucosa and granulation tissue with active chronic inflammation, H&E stain, 100x magnification.
D: 2-4 μm in size ovoid yeast with thin non-refractive cell walls and narrow bases, GMS stain, 600x magnification.
Disclosures:
Sharifeh Almasaid indicated no relevant financial relationships.
Abdelkader Chaar indicated no relevant financial relationships.
Oleksandr Kravtsov indicated no relevant financial relationships.
Idan Goren indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Sharifeh Almasaid, MD, MPH1, Abdelkader Chaar, MD1, Oleksandr Kravtsov, MD2, Idan Goren, MD1, Ganesh Aswath, MD2. P5598 - When Histoplasma Hides: Dissemination Histoplasmosis With Gastric Involvement in an Immunocompetent Patient After 8 Years of Latency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
