Tuesday Poster Session
Category: Infections and Microbiome
P5595 - Immunosuppressed and Infected: Pseudomembranous Colitis in a Liver Transplant Patient
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mauricio Jones, DO
Oklahoma State University
Tulsa, OK
Presenting Author(s)
Mauricio Jones, DO1, Maxwell A. Jones, MD2, Dipa Puwar, DO3, Fernando Magana, DO4
1Oklahoma State University, Tulsa, OK; 2University of Arkansas for Medical Sciences, Little Rock, AR; 3Saint Francis Health Systems, Tulsa, OK; 4Oklahoma State University Medical Center, Tulsa, OK
Introduction: We present Clostridioides difficile infection (CDI) in liver transplant recipients, which provides a unique clinical entity given its heightened risk, atypical presentation, and increased morbidity and mortality. Compared to the general hospitalized population, liver transplant patients have a "2.5- to 9-fold increased risk" of CDI due to immunosuppression, prolonged hospital stays, broad-spectrum antibiotic use, and comorbidities. The American College of Gastroenterology identifies liver transplant recipients as having the highest CDI risk among solid organ recipients, with an incidence of approximately 9%. Atypical presentation, including absence of fever or leukocytosis, can delay diagnosis and treatment. Prompt recognition is crucial given the associated risks of recurrence, graft loss, and increased mortality.
Case Description/
Methods: A liver transplant recipient with a history of cryptogenic cirrhosis was admitted for acute-onset back pain. During the hospitalization, he was noted to be anemic. Although he reported only 1–2 loose stools per day without abdominal pain, persistent anemia and mild GI symptoms prompted colonoscopy. Endoscopic evaluation revealed classic pseudomembranous colitis, and stool testing confirmed CDI. He was initiated on oral vancomycin with clinical improvement. Notably, he lacked typical CDI features such as fever or leukocytosis. His immunosuppression regimen, recent hospitalization, and antibiotic exposure were likely contributors to disease onset. The case highlights the importance of maintaining clinical suspicion for CDI even in the absence of traditional symptoms.
Discussion: This case highlights the diagnostic challenge of CDI in liver transplant patients, where symptoms may be mild or atypical. The patient’s anemia prompted further evaluation despite minimal GI complaints, ultimately leading to diagnosis. Immunosuppression may mask classical signs such as diarrhea, fever, or leukocytosis. Risk factors in this population, including high MELD scores, recent antimicrobial use, PPI therapy, and renal impairment, should heighten suspicion for CDI even in the absence of typical symptoms. Early detection and treatment are essential to prevent progression, recurrence, or graft loss.
Generative AI (ChatGPT, OpenAI) was utilized to assist with drafting and refining the language of this abstract. All clinical content was reviewed and verified by the authors.
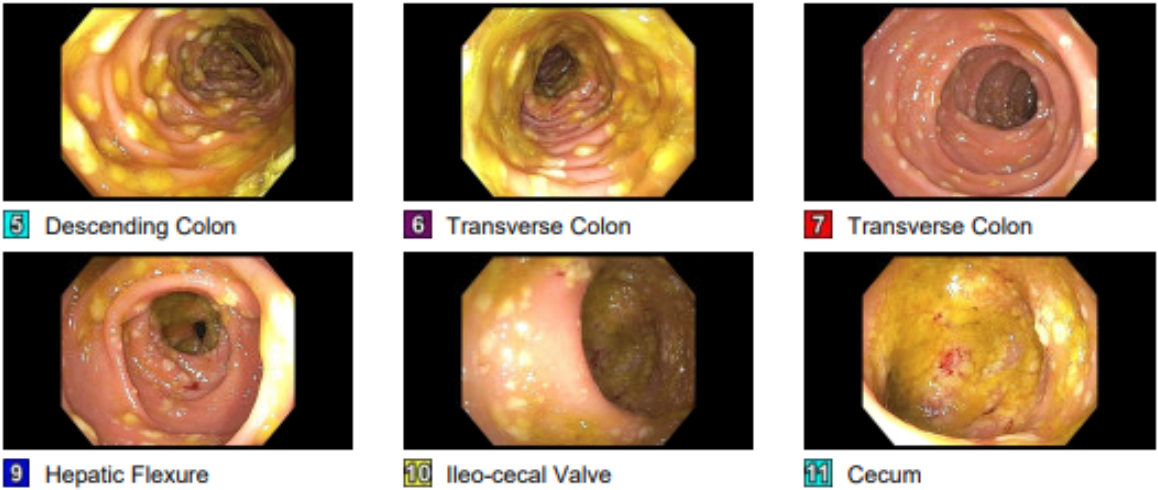
Figure: pseudomembranous colitis

Figure: pseudomembranous colitis
Disclosures:
Mauricio Jones indicated no relevant financial relationships.
Maxwell Jones indicated no relevant financial relationships.
Dipa Puwar indicated no relevant financial relationships.
Fernando Magana indicated no relevant financial relationships.
Mauricio Jones, DO1, Maxwell A. Jones, MD2, Dipa Puwar, DO3, Fernando Magana, DO4. P5595 - Immunosuppressed and Infected: Pseudomembranous Colitis in a Liver Transplant Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Oklahoma State University, Tulsa, OK; 2University of Arkansas for Medical Sciences, Little Rock, AR; 3Saint Francis Health Systems, Tulsa, OK; 4Oklahoma State University Medical Center, Tulsa, OK
Introduction: We present Clostridioides difficile infection (CDI) in liver transplant recipients, which provides a unique clinical entity given its heightened risk, atypical presentation, and increased morbidity and mortality. Compared to the general hospitalized population, liver transplant patients have a "2.5- to 9-fold increased risk" of CDI due to immunosuppression, prolonged hospital stays, broad-spectrum antibiotic use, and comorbidities. The American College of Gastroenterology identifies liver transplant recipients as having the highest CDI risk among solid organ recipients, with an incidence of approximately 9%. Atypical presentation, including absence of fever or leukocytosis, can delay diagnosis and treatment. Prompt recognition is crucial given the associated risks of recurrence, graft loss, and increased mortality.
Case Description/
Methods: A liver transplant recipient with a history of cryptogenic cirrhosis was admitted for acute-onset back pain. During the hospitalization, he was noted to be anemic. Although he reported only 1–2 loose stools per day without abdominal pain, persistent anemia and mild GI symptoms prompted colonoscopy. Endoscopic evaluation revealed classic pseudomembranous colitis, and stool testing confirmed CDI. He was initiated on oral vancomycin with clinical improvement. Notably, he lacked typical CDI features such as fever or leukocytosis. His immunosuppression regimen, recent hospitalization, and antibiotic exposure were likely contributors to disease onset. The case highlights the importance of maintaining clinical suspicion for CDI even in the absence of traditional symptoms.
Discussion: This case highlights the diagnostic challenge of CDI in liver transplant patients, where symptoms may be mild or atypical. The patient’s anemia prompted further evaluation despite minimal GI complaints, ultimately leading to diagnosis. Immunosuppression may mask classical signs such as diarrhea, fever, or leukocytosis. Risk factors in this population, including high MELD scores, recent antimicrobial use, PPI therapy, and renal impairment, should heighten suspicion for CDI even in the absence of typical symptoms. Early detection and treatment are essential to prevent progression, recurrence, or graft loss.
Generative AI (ChatGPT, OpenAI) was utilized to assist with drafting and refining the language of this abstract. All clinical content was reviewed and verified by the authors.
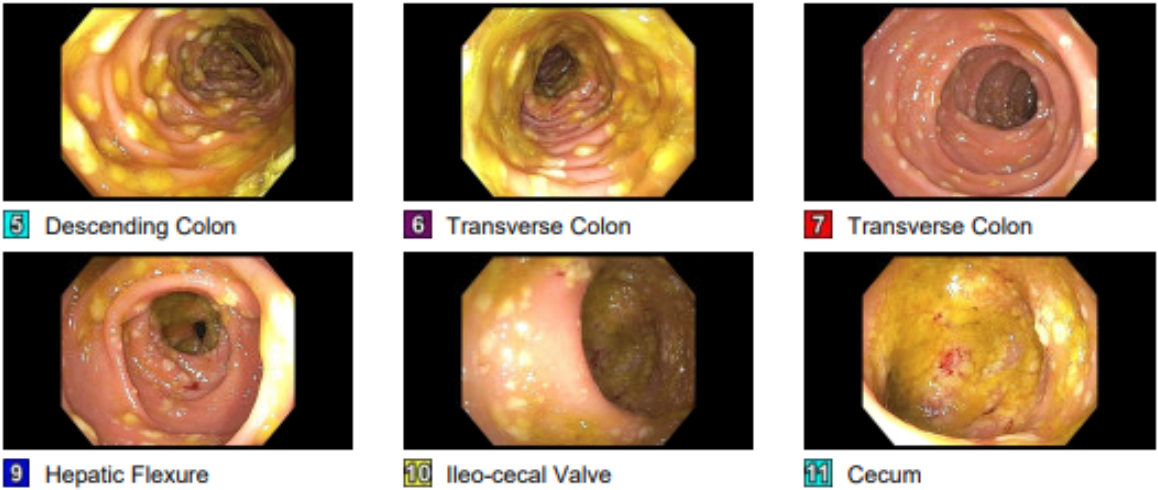
Figure: pseudomembranous colitis

Figure: pseudomembranous colitis
Disclosures:
Mauricio Jones indicated no relevant financial relationships.
Maxwell Jones indicated no relevant financial relationships.
Dipa Puwar indicated no relevant financial relationships.
Fernando Magana indicated no relevant financial relationships.
Mauricio Jones, DO1, Maxwell A. Jones, MD2, Dipa Puwar, DO3, Fernando Magana, DO4. P5595 - Immunosuppressed and Infected: Pseudomembranous Colitis in a Liver Transplant Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
