Tuesday Poster Session
Category: Infections and Microbiome
P5590 - Black Ulcers and Melena: A Rare Case of Fungal Esophagoduodenitis in an Immunocompetent Host
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aditya Kohli, MD
Trinity Health Oakland Hospital
Pontiac, MI
Presenting Author(s)
Aditya Kohli, MD1, Rakshana Ravichandran, MD1, Ravi Patel, MD1, Yash Shah, MD1, Dina Fakhouri. Bain, MD2
1Trinity Health Oakland Hospital, Pontiac, MI; 2Trinity Health Oakland / Wayne State University School of Medicine, Clarkston, MI
Introduction: Fungal infections of the gastrointestinal (GI) tract are uncommon and typically occur in immunocompromised patients, with Candida species being the most common organism and frequently involving the esophagus. Fungal duodenitis is rare, particularly without classic risk factors including HIV, transplantation, or recent chemotherapy. Melanized fungi produce brown pigmented hyphae and yeasts are usually associated with cutaneous or central nervous system infections. Here, we report a rare case of fungal duodenitis due to pigmented fungi in a diabetic patient without overt immunosuppression.
Case Description/
Methods: A 73-year old man with type 2 diabetes mellitus - well controlled, presented with symptoms of urinary tract infection and was managed with IV antibiotics. During hospitalization, the patient developed septic shock requiring vasopressors. ICU course was complicated with large volume loose watery diarrhea which tested negative for Clostridium difficile and later progressed to dark tarry stools, with a decline in hemoglobin levels from 12.5 g/dl to 8.9 g/dl (baseline 13-14 g/dl). Esophagogastroduodenoscopy (EGD) was performed and revealed complete circumferential ulceration of the esophagus with a dark base. Multiple non-bleeding duodenal ulcers with pigmented material were scattered throughout the duodenum [Image 1]. Duodenal biopsies demonstrated ulcerated tissue with abundant proliferating hyphae and yeast forms with brown pigmentation. Grocott-Gomori methenamine silver (GMS) staining was positive for fungi. Fungal cultures were not obtained due to low initial suspicion. The patient had no history of dysphagia, weight loss and immunosuppressive conditions. Patient was empirically treated with fluconazole, later escalated to micafungin to complete a 14-day course. Subsequently, the symptoms resolved with no further evidence of bleeding and repeat EGD [Image 2] demonstrated mucosal healing with negative Periodic Acid -Schiff (PAS) stain.
Discussion: Duodenal involvement by melanized (dematiaceous) fungi is exceedingly uncommon. These pigmented fungi typically cause cutaneous infections following traumatic implantation - the most common risk factor. Our patient had no typical predisposing conditions, making this an unusual presentation. This case broadens the spectrum of melanized fungal infections, even in immunocompetent patients. Antifungal therapy led to clinical improvement, but follow-up EGD is crucial to guide the duration and intensity of treatment.
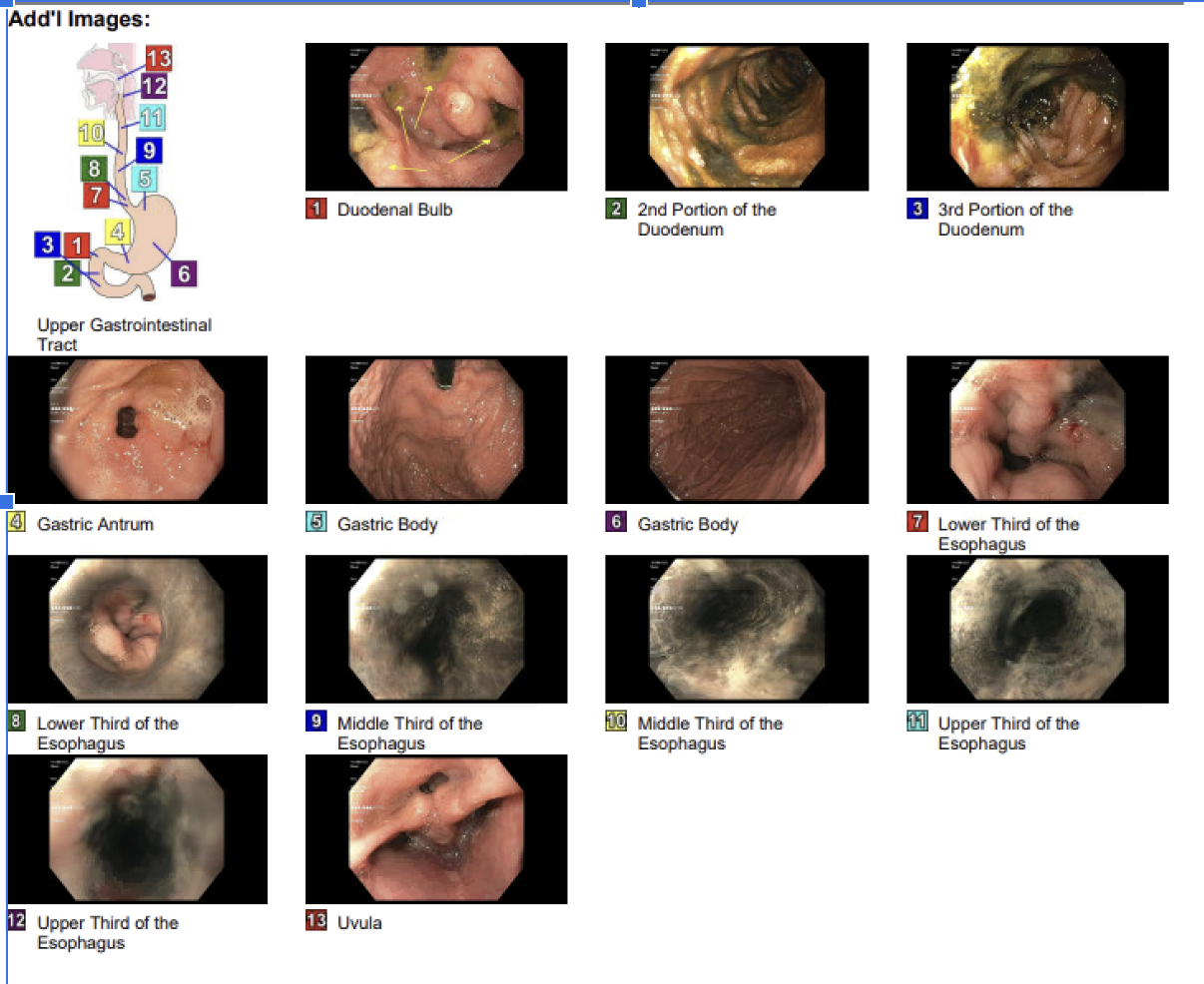
Figure: EGD findings on initial presentation
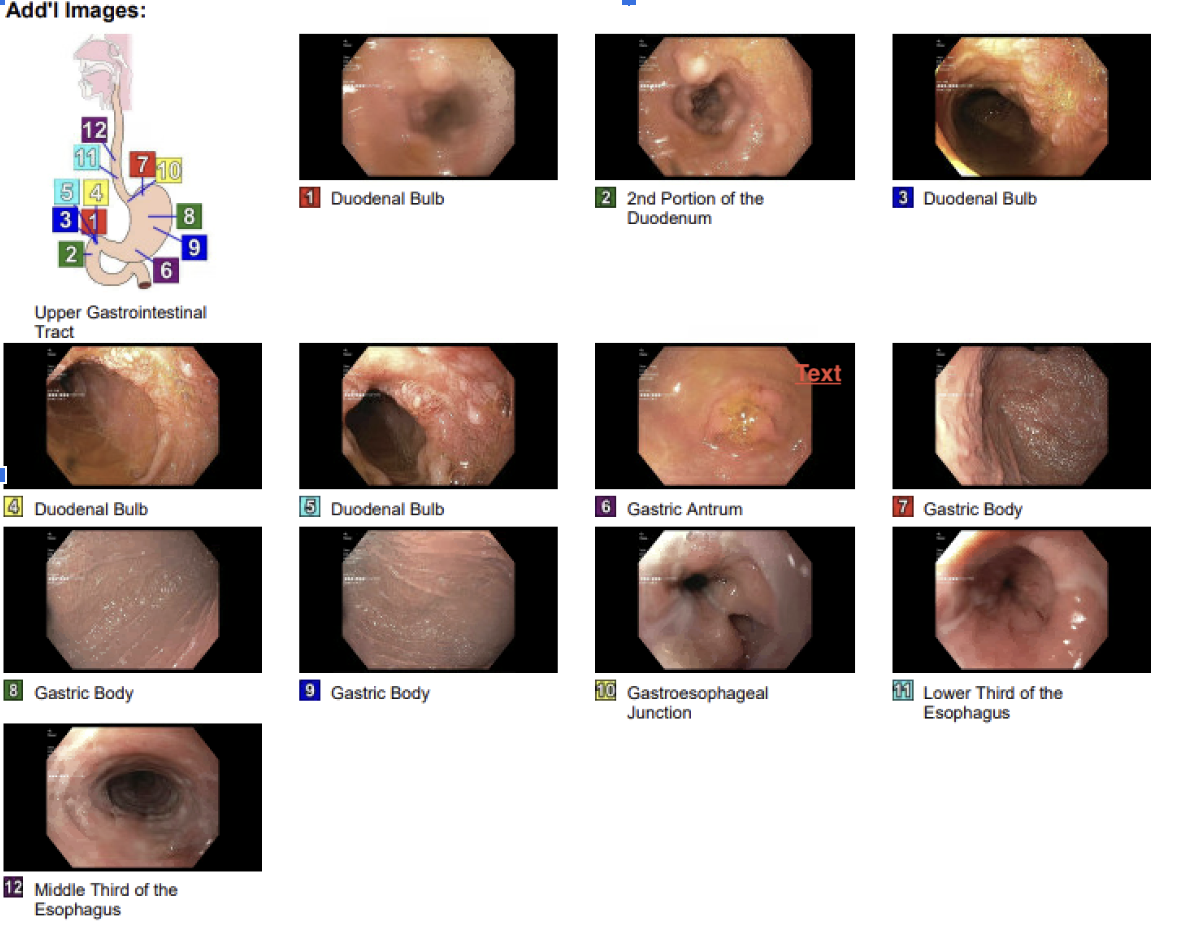
Figure: Follow-up EGD after antifungal treatment
Disclosures:
Aditya Kohli indicated no relevant financial relationships.
Rakshana Ravichandran indicated no relevant financial relationships.
Ravi Patel indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Dina Bain indicated no relevant financial relationships.
Aditya Kohli, MD1, Rakshana Ravichandran, MD1, Ravi Patel, MD1, Yash Shah, MD1, Dina Fakhouri. Bain, MD2. P5590 - Black Ulcers and Melena: A Rare Case of Fungal Esophagoduodenitis in an Immunocompetent Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Trinity Health Oakland Hospital, Pontiac, MI; 2Trinity Health Oakland / Wayne State University School of Medicine, Clarkston, MI
Introduction: Fungal infections of the gastrointestinal (GI) tract are uncommon and typically occur in immunocompromised patients, with Candida species being the most common organism and frequently involving the esophagus. Fungal duodenitis is rare, particularly without classic risk factors including HIV, transplantation, or recent chemotherapy. Melanized fungi produce brown pigmented hyphae and yeasts are usually associated with cutaneous or central nervous system infections. Here, we report a rare case of fungal duodenitis due to pigmented fungi in a diabetic patient without overt immunosuppression.
Case Description/
Methods: A 73-year old man with type 2 diabetes mellitus - well controlled, presented with symptoms of urinary tract infection and was managed with IV antibiotics. During hospitalization, the patient developed septic shock requiring vasopressors. ICU course was complicated with large volume loose watery diarrhea which tested negative for Clostridium difficile and later progressed to dark tarry stools, with a decline in hemoglobin levels from 12.5 g/dl to 8.9 g/dl (baseline 13-14 g/dl). Esophagogastroduodenoscopy (EGD) was performed and revealed complete circumferential ulceration of the esophagus with a dark base. Multiple non-bleeding duodenal ulcers with pigmented material were scattered throughout the duodenum [Image 1]. Duodenal biopsies demonstrated ulcerated tissue with abundant proliferating hyphae and yeast forms with brown pigmentation. Grocott-Gomori methenamine silver (GMS) staining was positive for fungi. Fungal cultures were not obtained due to low initial suspicion. The patient had no history of dysphagia, weight loss and immunosuppressive conditions. Patient was empirically treated with fluconazole, later escalated to micafungin to complete a 14-day course. Subsequently, the symptoms resolved with no further evidence of bleeding and repeat EGD [Image 2] demonstrated mucosal healing with negative Periodic Acid -Schiff (PAS) stain.
Discussion: Duodenal involvement by melanized (dematiaceous) fungi is exceedingly uncommon. These pigmented fungi typically cause cutaneous infections following traumatic implantation - the most common risk factor. Our patient had no typical predisposing conditions, making this an unusual presentation. This case broadens the spectrum of melanized fungal infections, even in immunocompetent patients. Antifungal therapy led to clinical improvement, but follow-up EGD is crucial to guide the duration and intensity of treatment.
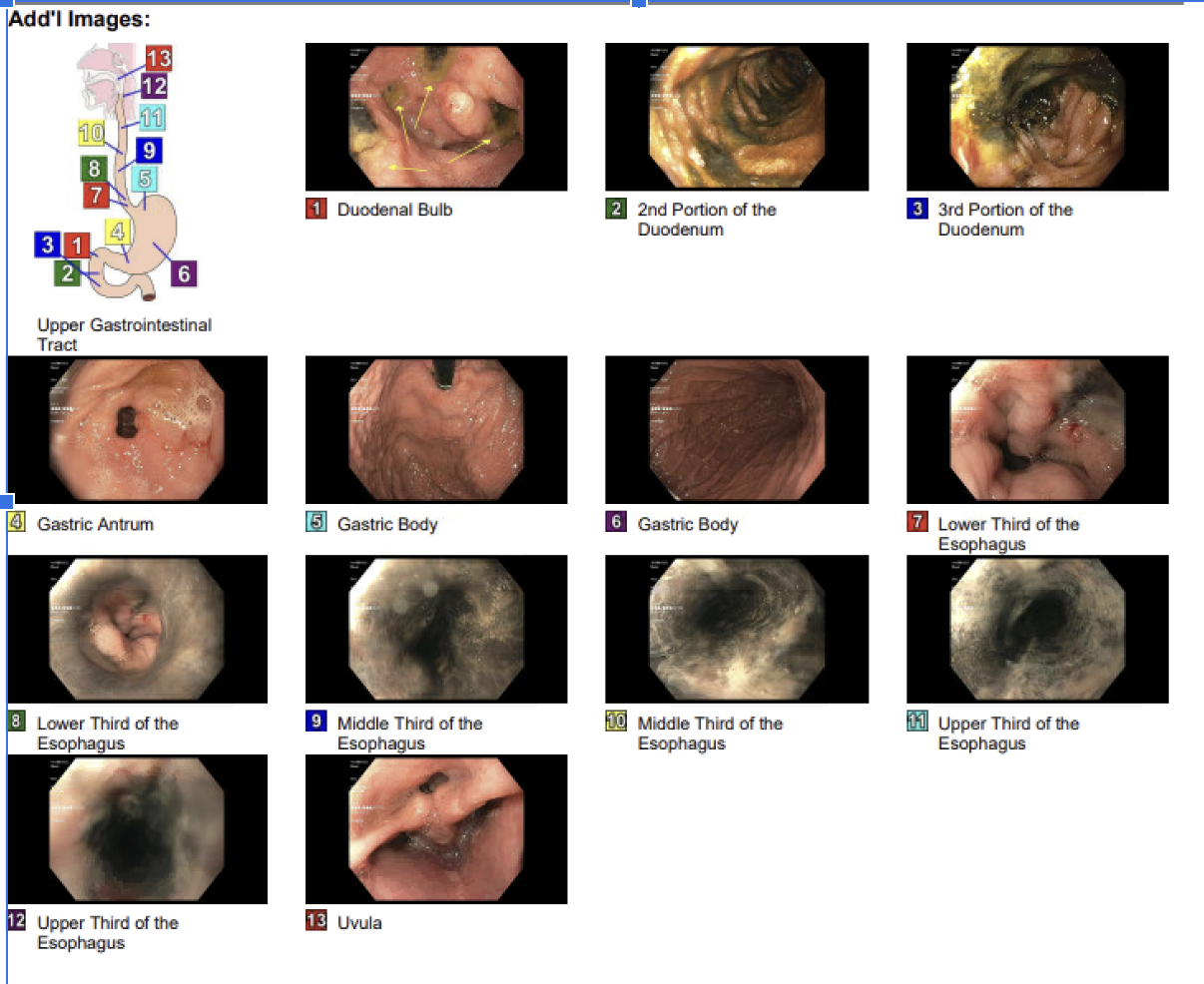
Figure: EGD findings on initial presentation
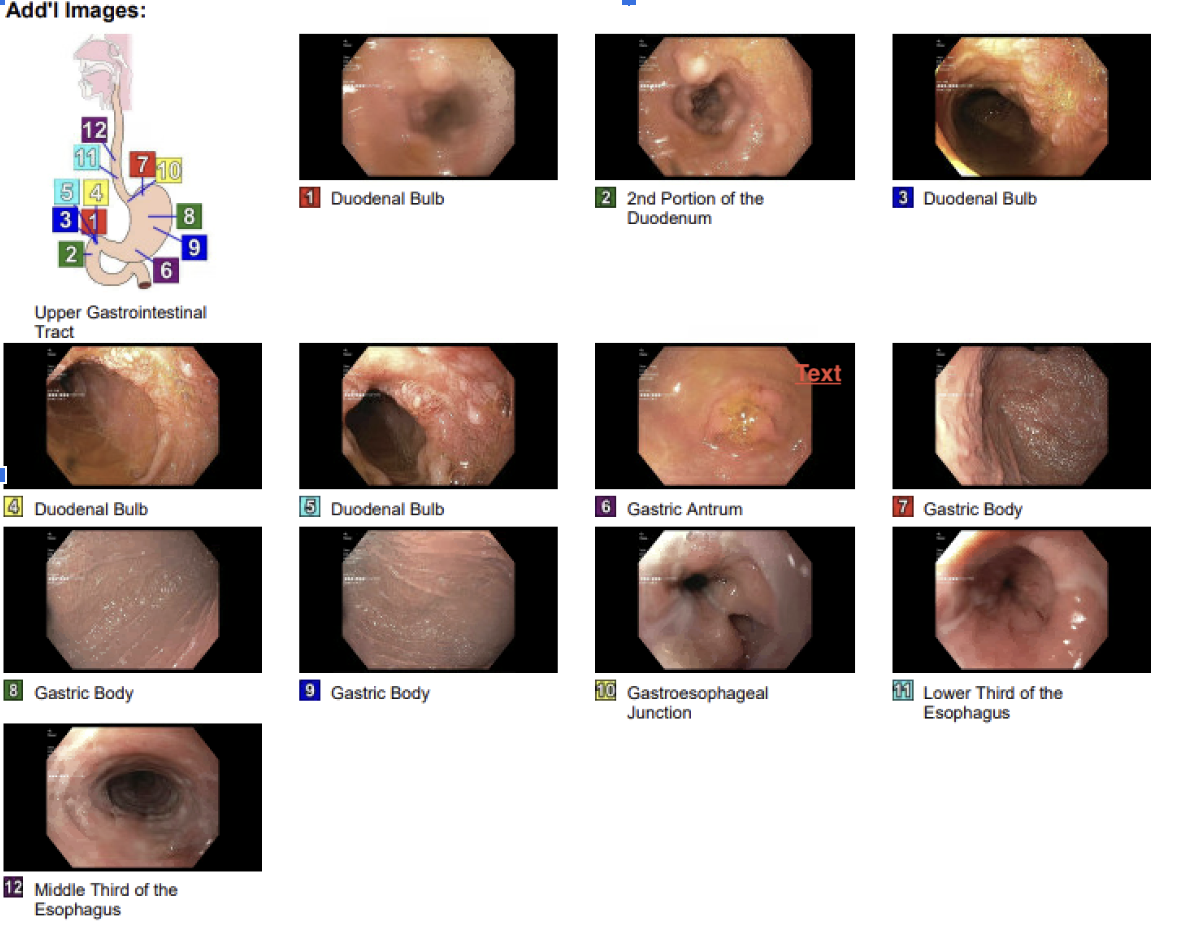
Figure: Follow-up EGD after antifungal treatment
Disclosures:
Aditya Kohli indicated no relevant financial relationships.
Rakshana Ravichandran indicated no relevant financial relationships.
Ravi Patel indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Dina Bain indicated no relevant financial relationships.
Aditya Kohli, MD1, Rakshana Ravichandran, MD1, Ravi Patel, MD1, Yash Shah, MD1, Dina Fakhouri. Bain, MD2. P5590 - Black Ulcers and Melena: A Rare Case of Fungal Esophagoduodenitis in an Immunocompetent Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
