Tuesday Poster Session
Category: Infections and Microbiome
P5559 - H. pylori in Sickle Cell Disease: A Single Center Retrospective Study of Prevalence, Risk, and Outcomes
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

John Pueringer, DO
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
John Pueringer, DO1, Jessica E. McClain, MD2, Cierra Jarmon, MD1, Emily Muscat, MD1, Myles Bosompem, MD1, Deene Mohandas, MD1, Evan Garrad, MD1, Yousif Esho, MD1, Michael Fayad, DO2, Marwah Farooqui, DO1, Wadih Chacra, MD1, Robert Molokie, MD1
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois Chicago, Chicago, IL
Introduction: Research is limited regarding the association between Helicobacter pylori (H. pylori) infection and sickle cell disease (SCD). Further characterization of the SCD population’s H. pylori infection prevalence and susceptibility would be beneficial to our understanding of their risk and potential complications. This study aims to investigate the relationship between SCD and H. pylori infection in the adult population.
Methods: We conducted a retrospective chart review of adult patients with SCD who presented to UIC between 1/1/2020 and 3/31/2024. The primary outcome was a diagnosis of H. pylori. Data collected includes variables such as demographics, genotype, regimen of H. pylori treatment, number of times treated, testing for cure, complications of SCD prior to diagnosis of H. pylori, medications prior to diagnosis of H. pylori, and complications related to infection. Statistical analysis was performed with Pearson Chi-Square, Fischer’s Exact Test, and Odds Ratio to compare categorical variables and risk.
Results: Of 1,484 patients, 828 had sickle cell disease (SCD), with 85 (10%) testing positive for Helicobacter pylori (HP+) (Table 1). HP+ SCD patients were older (46.1 vs. 38.9 years) and more often female (72%) compared to the overall SCD group (Table 1). HP testing occurred in 30% of SCD patients, with a 5% positivity rate (Table 2). Most HP+ SCD patients had HbSS (74%) (Table 1). Vaso-occlusive crises (VOC) were significantly more frequent in HP+ vs. HP− patients (64% vs. 42%, p=0.015, OR 2.59) (Table 3). Other SCD complications did not differ significantly. Risk factor usage, including NSAIDs and hydroxyurea, showed no statistical differences, though glucocorticoid use trended higher in HP+ patients (p=0.086) (Table 4). Most SCD patients received one HP treatment, with triple therapy being most common (33%), followed by bismuth quadruple therapy (21%) (Table 5). GERD was significantly more prevalent in non-SCD HP+ patients (50% vs. 28%, p=0.020), while other GI complications were similar (Table 6).
Discussion: Our findings suggest a notable association between H. pylori infection and vaso-occlusive crises in adults with sickle cell disease. Although overall H. pylori prevalence was low, infected individuals were older and predominantly female. The higher VOC rate highlights a potential clinical impact warranting further investigation. Routine screening for H. pylori in SCD patients with GI symptoms may be beneficial in reducing complications.
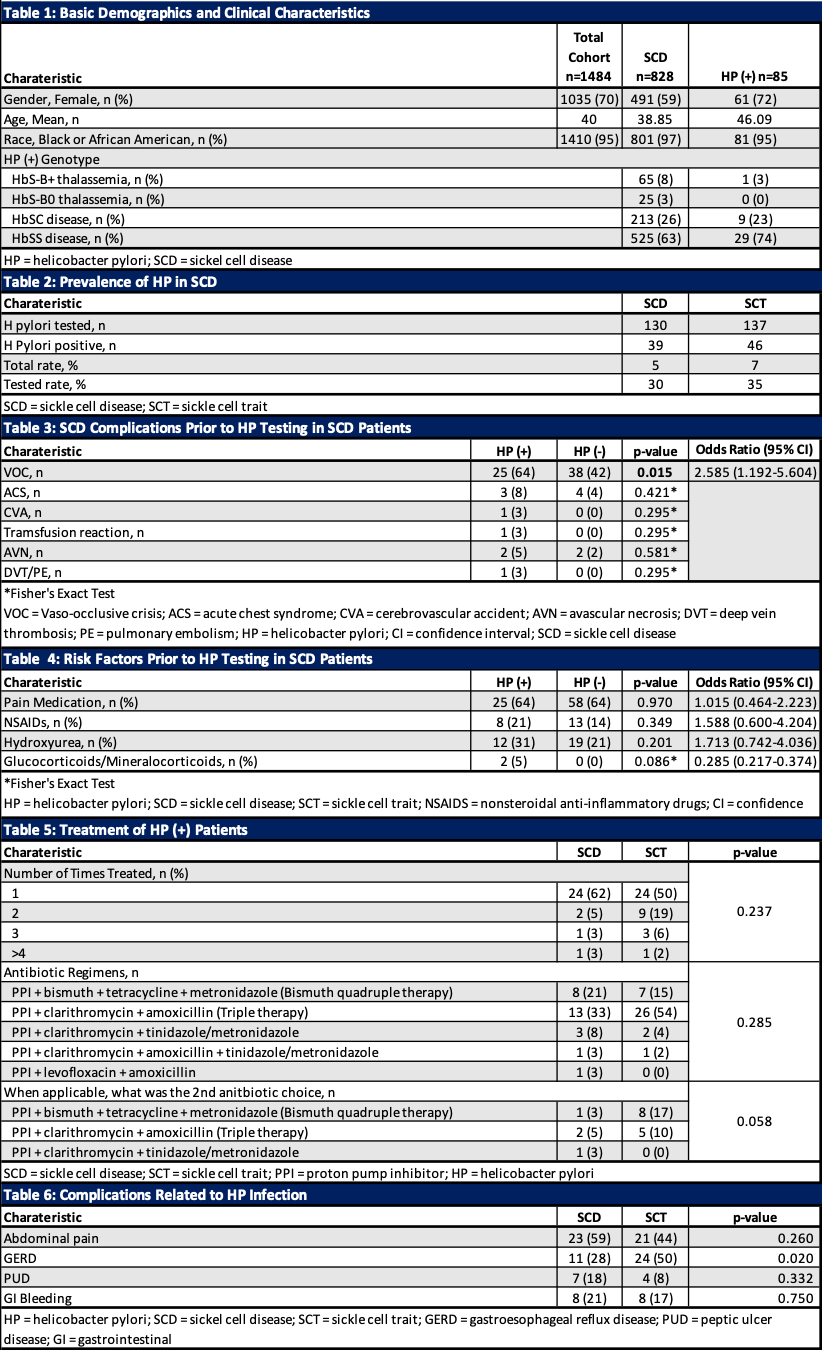
Figure: Table 1–6. Demographics, Clinical Characteristics, Risk Factors, and Treatment Outcomes Related to Helicobacter pylori in Patients with Sickle Cell Disease (SCD).
Disclosures:
John Pueringer indicated no relevant financial relationships.
Jessica McClain indicated no relevant financial relationships.
Cierra Jarmon indicated no relevant financial relationships.
Emily Muscat indicated no relevant financial relationships.
Myles Bosompem indicated no relevant financial relationships.
Deene Mohandas indicated no relevant financial relationships.
Evan Garrad indicated no relevant financial relationships.
Yousif Esho indicated no relevant financial relationships.
Michael Fayad indicated no relevant financial relationships.
Marwah Farooqui indicated no relevant financial relationships.
Wadih Chacra indicated no relevant financial relationships.
Robert Molokie indicated no relevant financial relationships.
John Pueringer, DO1, Jessica E. McClain, MD2, Cierra Jarmon, MD1, Emily Muscat, MD1, Myles Bosompem, MD1, Deene Mohandas, MD1, Evan Garrad, MD1, Yousif Esho, MD1, Michael Fayad, DO2, Marwah Farooqui, DO1, Wadih Chacra, MD1, Robert Molokie, MD1. P5559 - <i>H. pylori</i> in Sickle Cell Disease: A Single Center Retrospective Study of Prevalence, Risk, and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois Chicago, Chicago, IL
Introduction: Research is limited regarding the association between Helicobacter pylori (H. pylori) infection and sickle cell disease (SCD). Further characterization of the SCD population’s H. pylori infection prevalence and susceptibility would be beneficial to our understanding of their risk and potential complications. This study aims to investigate the relationship between SCD and H. pylori infection in the adult population.
Methods: We conducted a retrospective chart review of adult patients with SCD who presented to UIC between 1/1/2020 and 3/31/2024. The primary outcome was a diagnosis of H. pylori. Data collected includes variables such as demographics, genotype, regimen of H. pylori treatment, number of times treated, testing for cure, complications of SCD prior to diagnosis of H. pylori, medications prior to diagnosis of H. pylori, and complications related to infection. Statistical analysis was performed with Pearson Chi-Square, Fischer’s Exact Test, and Odds Ratio to compare categorical variables and risk.
Results: Of 1,484 patients, 828 had sickle cell disease (SCD), with 85 (10%) testing positive for Helicobacter pylori (HP+) (Table 1). HP+ SCD patients were older (46.1 vs. 38.9 years) and more often female (72%) compared to the overall SCD group (Table 1). HP testing occurred in 30% of SCD patients, with a 5% positivity rate (Table 2). Most HP+ SCD patients had HbSS (74%) (Table 1). Vaso-occlusive crises (VOC) were significantly more frequent in HP+ vs. HP− patients (64% vs. 42%, p=0.015, OR 2.59) (Table 3). Other SCD complications did not differ significantly. Risk factor usage, including NSAIDs and hydroxyurea, showed no statistical differences, though glucocorticoid use trended higher in HP+ patients (p=0.086) (Table 4). Most SCD patients received one HP treatment, with triple therapy being most common (33%), followed by bismuth quadruple therapy (21%) (Table 5). GERD was significantly more prevalent in non-SCD HP+ patients (50% vs. 28%, p=0.020), while other GI complications were similar (Table 6).
Discussion: Our findings suggest a notable association between H. pylori infection and vaso-occlusive crises in adults with sickle cell disease. Although overall H. pylori prevalence was low, infected individuals were older and predominantly female. The higher VOC rate highlights a potential clinical impact warranting further investigation. Routine screening for H. pylori in SCD patients with GI symptoms may be beneficial in reducing complications.
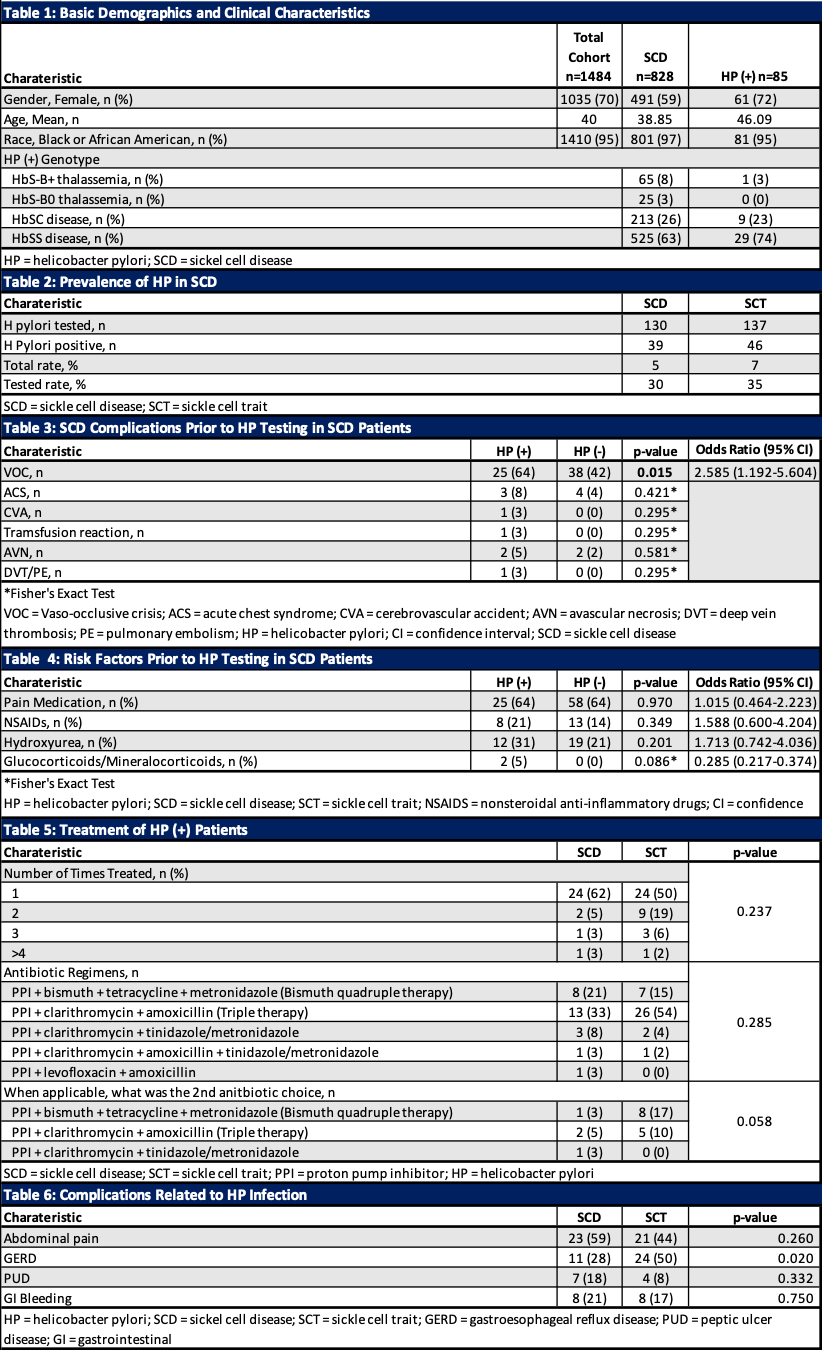
Figure: Table 1–6. Demographics, Clinical Characteristics, Risk Factors, and Treatment Outcomes Related to Helicobacter pylori in Patients with Sickle Cell Disease (SCD).
Disclosures:
John Pueringer indicated no relevant financial relationships.
Jessica McClain indicated no relevant financial relationships.
Cierra Jarmon indicated no relevant financial relationships.
Emily Muscat indicated no relevant financial relationships.
Myles Bosompem indicated no relevant financial relationships.
Deene Mohandas indicated no relevant financial relationships.
Evan Garrad indicated no relevant financial relationships.
Yousif Esho indicated no relevant financial relationships.
Michael Fayad indicated no relevant financial relationships.
Marwah Farooqui indicated no relevant financial relationships.
Wadih Chacra indicated no relevant financial relationships.
Robert Molokie indicated no relevant financial relationships.
John Pueringer, DO1, Jessica E. McClain, MD2, Cierra Jarmon, MD1, Emily Muscat, MD1, Myles Bosompem, MD1, Deene Mohandas, MD1, Evan Garrad, MD1, Yousif Esho, MD1, Michael Fayad, DO2, Marwah Farooqui, DO1, Wadih Chacra, MD1, Robert Molokie, MD1. P5559 - <i>H. pylori</i> in Sickle Cell Disease: A Single Center Retrospective Study of Prevalence, Risk, and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

