Tuesday Poster Session
Category: IBD
P5551 - Rapid Evolution to Penetrating Crohn’s Disease Shortly After Vedolizumab Induction in a Newly Diagnosed Crohn’s Patient
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Angsupat Pornchai, MD (she/her/hers)
University of Pittsburgh Medical Center
Harrisburg, PA
Presenting Author(s)
Angsupat Pornchai, MD1, Nicha Wongjarupong, MD2, Adil Mir, MD3
1University of Pittsburgh Medical Center, Harrisburg, PA; 2Cedars-Sinai Medical Center, Los Angeles, CA; 3Augusta Health, Fishersville, VA
Introduction: Vedolizumab is a gut‐selective anti‐integrin approved for induction and maintenance of moderate‐to‐severe Crohn’s disease (CD). Its delayed onset (6–10 weeks) renders it less suitable for penetrating or fistulizing disease. We describe a young man whose disease rapidly evolved to intra‐abdominal abscess and entero‐enteric fistulas shortly after vedolizumab initiation, highlighting the need for guideline-based therapy selection and bridging strategies.
Case Description/
Methods: A 23-year-old man with CD diagnosed three months earlier (after partial small-bowel obstruction) began vedolizumab and prednisone 40 mg daily. Two weeks later, he developed right lower quadrant abdominal pain and non-bloody diarrhea, without fever for 3 days. White blood cell count was 23.9 × 10³/µL and c-reactive protein was 13.6 mg/dL. Computed tomography (CT) abdomen demonstrated severe terminal ileal inflammation and two rim-enhancing air–fluid collections adjacent to the distal ileum and sigmoid colon; Magnetic resonance imaging enterography excluded fistulas. Empiric antibiotics with cefepime, vancomycin, and metronidazole were initiated. Prednisone and the second dose of vedolizumab were deferred due to concern of infection. A percutaneous Jackson-Pratt drain was placed and yielded 20 mL of purulent fluid growing aerobic gram-negative rods. Clinical and biochemical parameters improved rapidly. Antibiotics were de-escalated to ceftriaxone and metronidazole, then transitioned to oral ciprofloxacin/metronidazole to complete a 10-day course. The patient was discharged on day 5 and received vedolizumab the next day. One week later, CT confirmed abscess resolution, but Fluoroscopy fistulogram revealed new small-bowel fistulas, necessitating prolonged drainage and multidisciplinary follow-up.
Discussion: Vedolizumab’s slow onset requires steroid bridging, but steroids were halted once the abscess emerged to limit infection. In penetrating or fistulizing Crohn’s disease, anti-TNF therapy—particularly infliximab—offers superior efficacy and better prevention of complications; early use may have averted abscess formation in our patient. Timely recognition of vedolizumab’s pharmacodynamics and adherence to guideline-based risk stratification are essential to avoid adverse outcomes in newly diagnosed CD and rapid escalation of symptoms—even without fever—should prompt cross-sectional imaging to detect occult penetrating complications before sepsis ensues.
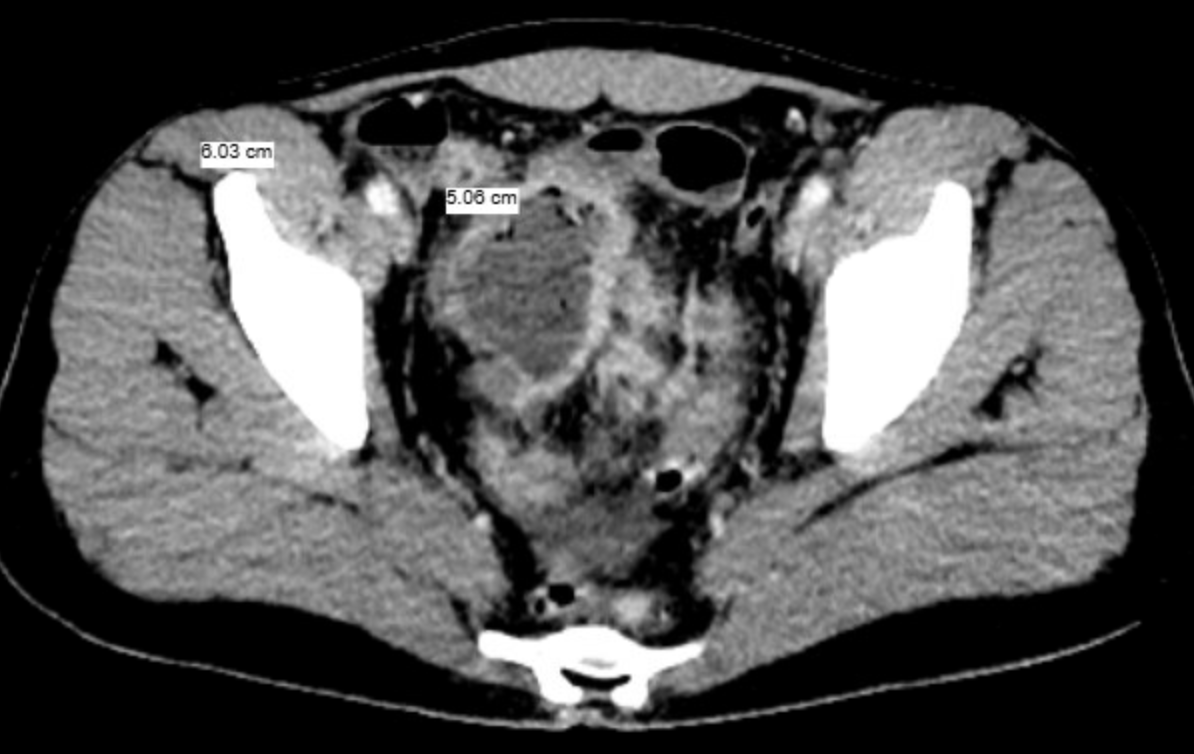
Figure: Contrast-enhanced CT of the abdomen and pelvis demonstrates a 5.2 × 6.0 × 5.1 cm rim-enhancing mixed air–fluid collection adjacent to the inflamed distal ileum, with additional smaller abscesses next to it, contiguous with the sigmoid colon.
Disclosures:
Angsupat Pornchai indicated no relevant financial relationships.
Nicha Wongjarupong indicated no relevant financial relationships.
Adil Mir indicated no relevant financial relationships.
Angsupat Pornchai, MD1, Nicha Wongjarupong, MD2, Adil Mir, MD3. P5551 - Rapid Evolution to Penetrating Crohn’s Disease Shortly After Vedolizumab Induction in a Newly Diagnosed Crohn’s Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pittsburgh Medical Center, Harrisburg, PA; 2Cedars-Sinai Medical Center, Los Angeles, CA; 3Augusta Health, Fishersville, VA
Introduction: Vedolizumab is a gut‐selective anti‐integrin approved for induction and maintenance of moderate‐to‐severe Crohn’s disease (CD). Its delayed onset (6–10 weeks) renders it less suitable for penetrating or fistulizing disease. We describe a young man whose disease rapidly evolved to intra‐abdominal abscess and entero‐enteric fistulas shortly after vedolizumab initiation, highlighting the need for guideline-based therapy selection and bridging strategies.
Case Description/
Methods: A 23-year-old man with CD diagnosed three months earlier (after partial small-bowel obstruction) began vedolizumab and prednisone 40 mg daily. Two weeks later, he developed right lower quadrant abdominal pain and non-bloody diarrhea, without fever for 3 days. White blood cell count was 23.9 × 10³/µL and c-reactive protein was 13.6 mg/dL. Computed tomography (CT) abdomen demonstrated severe terminal ileal inflammation and two rim-enhancing air–fluid collections adjacent to the distal ileum and sigmoid colon; Magnetic resonance imaging enterography excluded fistulas. Empiric antibiotics with cefepime, vancomycin, and metronidazole were initiated. Prednisone and the second dose of vedolizumab were deferred due to concern of infection. A percutaneous Jackson-Pratt drain was placed and yielded 20 mL of purulent fluid growing aerobic gram-negative rods. Clinical and biochemical parameters improved rapidly. Antibiotics were de-escalated to ceftriaxone and metronidazole, then transitioned to oral ciprofloxacin/metronidazole to complete a 10-day course. The patient was discharged on day 5 and received vedolizumab the next day. One week later, CT confirmed abscess resolution, but Fluoroscopy fistulogram revealed new small-bowel fistulas, necessitating prolonged drainage and multidisciplinary follow-up.
Discussion: Vedolizumab’s slow onset requires steroid bridging, but steroids were halted once the abscess emerged to limit infection. In penetrating or fistulizing Crohn’s disease, anti-TNF therapy—particularly infliximab—offers superior efficacy and better prevention of complications; early use may have averted abscess formation in our patient. Timely recognition of vedolizumab’s pharmacodynamics and adherence to guideline-based risk stratification are essential to avoid adverse outcomes in newly diagnosed CD and rapid escalation of symptoms—even without fever—should prompt cross-sectional imaging to detect occult penetrating complications before sepsis ensues.
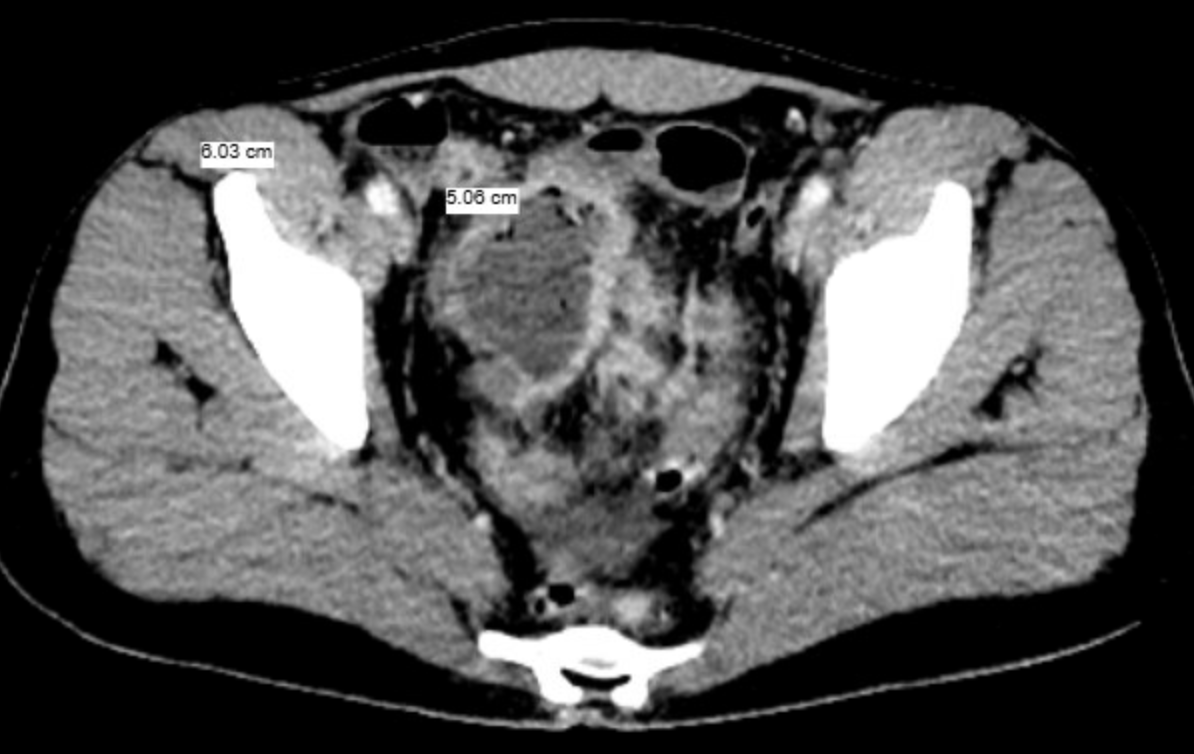
Figure: Contrast-enhanced CT of the abdomen and pelvis demonstrates a 5.2 × 6.0 × 5.1 cm rim-enhancing mixed air–fluid collection adjacent to the inflamed distal ileum, with additional smaller abscesses next to it, contiguous with the sigmoid colon.
Disclosures:
Angsupat Pornchai indicated no relevant financial relationships.
Nicha Wongjarupong indicated no relevant financial relationships.
Adil Mir indicated no relevant financial relationships.
Angsupat Pornchai, MD1, Nicha Wongjarupong, MD2, Adil Mir, MD3. P5551 - Rapid Evolution to Penetrating Crohn’s Disease Shortly After Vedolizumab Induction in a Newly Diagnosed Crohn’s Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
