Tuesday Poster Session
Category: IBD
P5546 - Unpredictable and Unrelenting: A Catastrophic Crohn’s Flare in Mid-Pregnancy Despite Biologic Therapy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mujtaba Moazzam, MD
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Mujtaba Moazzam, MD1, Usman Bin Hameed, MD1, Fady Banno, MD2, Aleena Sharif, MBBS3, Ayesha Sharif, MD4, Saman Amjad, MD1
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Carewell Health William Beaumont Hospital, Royal Oak, MI; 3Sheikh Zayed Medical College Raheem Yar Khan, Bahawalpur, Punjab, Pakistan; 4William Beaumont hospital, Royal Oak, MI
Introduction: Crohn’s disease (CD) frequently affects women of reproductive age. While favorable pregnancy outcomes are achievable, active disease markedly increases the risks of miscarriage, preterm birth, and fetal growth restriction. We present a case of a severe Crohn’s flare in mid-pregnancy complicated by bowel perforation and intrauterine fetal demise (IUFD).
Case Description/
Methods: A 38-year-old gravida 8, para 6 woman with a 10-year history of CD presented at 21 weeks gestation with worsening abdominal pain. Her CD had previously been poorly controlled on adalimumab; colonoscopy two years prior demonstrated significant terminal ileitis. She was steroid-dependent and had been switched to ustekinumab two months prior. Her obstetric history included multiple uncomplicated vaginal deliveries.
Her abdominal pain had been worsening despite oral steroids. CRP was elevated (80.5 mg/dl) and rising. Suspecting a CD flare, intravenous methylprednisolone was initiated while continuing ustekinumab. MRI revealed active terminal ileitis. Her symptoms worsened with increasing pain and decreased bowel movements. Ultimately, she became hemodynamically unstable prompting urgent laparotomy. Surgery revealed perforation of the terminal ileum and cecum; a 30 cm resection was performed. Unfortunately, she experienced intrauterine fetal demise at 22 weeks and underwent medically induced delivery.
Discussion: This case illustrates a catastrophic CD flare in mid-pregnancy leading to perforation and IUFD, despite being on biologic therapy. Although biologics, like ustekinumab, are generally effective and low-risk in pregnancy, 10–20% of patients still flare. Contributing factors in this patient included steroid dependence, recent biologic transition, high disease burden, and likely active disease at the time of conception.
Guidelines strongly recommend that women achieve deep remission prior to conception and continue biologic therapy during pregnancy to prevent flares. Active disease at conception significantly increases the risk of adverse events, including preterm birth, fetal growth restriction, and pregnancy loss. Therefore, women with uncontrolled or moderate-to-severe CD are advised to delay pregnancy until remission is confirmed.
This case reinforces the critical role of preconception counseling, medication adherence, and multidisciplinary care. It also underscores the psychosocial toll of IUFD and critical illness, highlighting the need for compassionate, holistic management in high-risk IBD pregnancies.
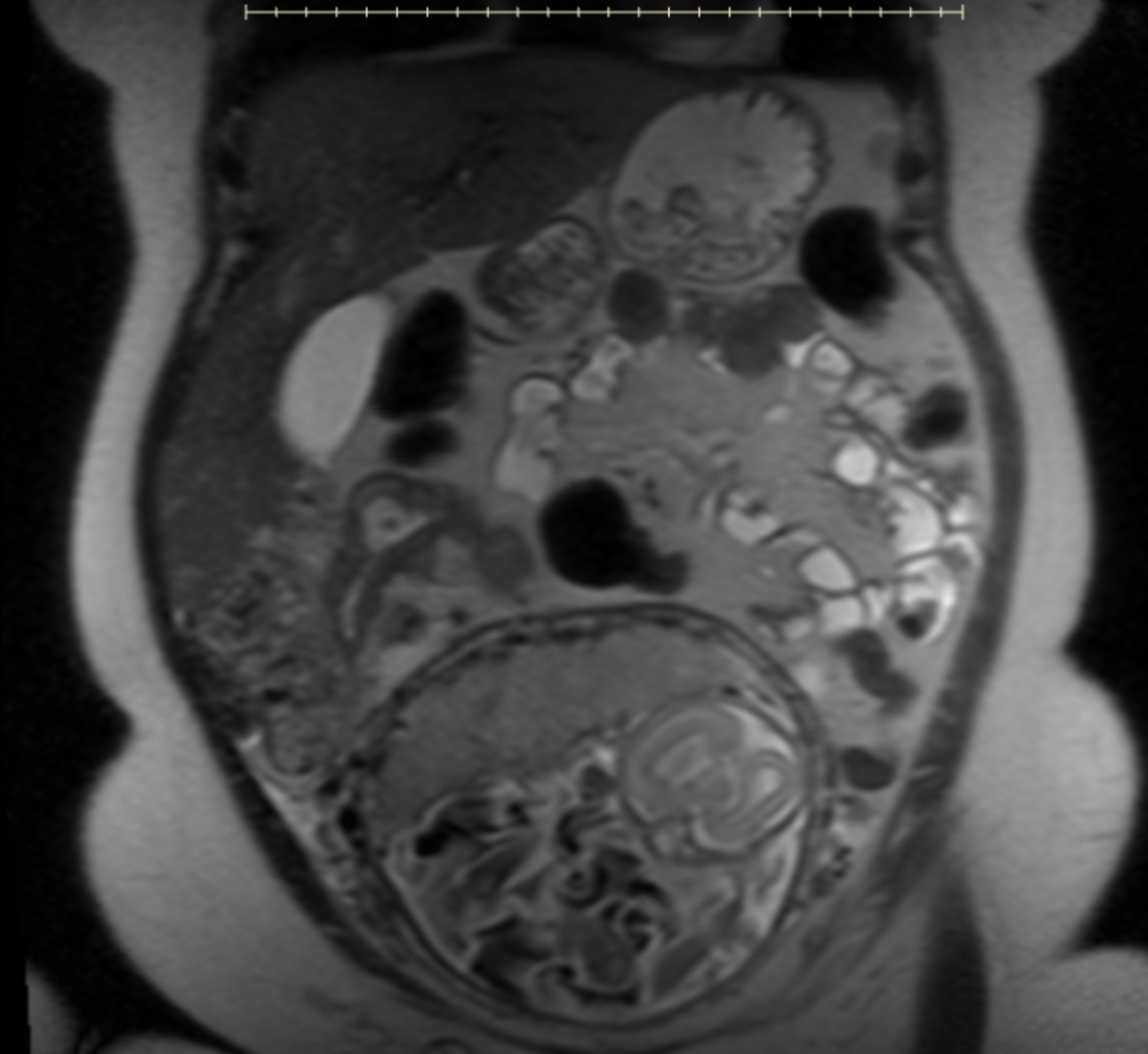
Figure: MRI abdomen with active inflammation involving approximately 5 cm segment of terminal ileum
Disclosures:
Mujtaba Moazzam indicated no relevant financial relationships.
Usman Bin Hameed indicated no relevant financial relationships.
Fady Banno indicated no relevant financial relationships.
Aleena Sharif indicated no relevant financial relationships.
Ayesha Sharif indicated no relevant financial relationships.
Saman Amjad indicated no relevant financial relationships.
Mujtaba Moazzam, MD1, Usman Bin Hameed, MD1, Fady Banno, MD2, Aleena Sharif, MBBS3, Ayesha Sharif, MD4, Saman Amjad, MD1. P5546 - Unpredictable and Unrelenting: A Catastrophic Crohn’s Flare in Mid-Pregnancy Despite Biologic Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Carewell Health William Beaumont Hospital, Royal Oak, MI; 3Sheikh Zayed Medical College Raheem Yar Khan, Bahawalpur, Punjab, Pakistan; 4William Beaumont hospital, Royal Oak, MI
Introduction: Crohn’s disease (CD) frequently affects women of reproductive age. While favorable pregnancy outcomes are achievable, active disease markedly increases the risks of miscarriage, preterm birth, and fetal growth restriction. We present a case of a severe Crohn’s flare in mid-pregnancy complicated by bowel perforation and intrauterine fetal demise (IUFD).
Case Description/
Methods: A 38-year-old gravida 8, para 6 woman with a 10-year history of CD presented at 21 weeks gestation with worsening abdominal pain. Her CD had previously been poorly controlled on adalimumab; colonoscopy two years prior demonstrated significant terminal ileitis. She was steroid-dependent and had been switched to ustekinumab two months prior. Her obstetric history included multiple uncomplicated vaginal deliveries.
Her abdominal pain had been worsening despite oral steroids. CRP was elevated (80.5 mg/dl) and rising. Suspecting a CD flare, intravenous methylprednisolone was initiated while continuing ustekinumab. MRI revealed active terminal ileitis. Her symptoms worsened with increasing pain and decreased bowel movements. Ultimately, she became hemodynamically unstable prompting urgent laparotomy. Surgery revealed perforation of the terminal ileum and cecum; a 30 cm resection was performed. Unfortunately, she experienced intrauterine fetal demise at 22 weeks and underwent medically induced delivery.
Discussion: This case illustrates a catastrophic CD flare in mid-pregnancy leading to perforation and IUFD, despite being on biologic therapy. Although biologics, like ustekinumab, are generally effective and low-risk in pregnancy, 10–20% of patients still flare. Contributing factors in this patient included steroid dependence, recent biologic transition, high disease burden, and likely active disease at the time of conception.
Guidelines strongly recommend that women achieve deep remission prior to conception and continue biologic therapy during pregnancy to prevent flares. Active disease at conception significantly increases the risk of adverse events, including preterm birth, fetal growth restriction, and pregnancy loss. Therefore, women with uncontrolled or moderate-to-severe CD are advised to delay pregnancy until remission is confirmed.
This case reinforces the critical role of preconception counseling, medication adherence, and multidisciplinary care. It also underscores the psychosocial toll of IUFD and critical illness, highlighting the need for compassionate, holistic management in high-risk IBD pregnancies.
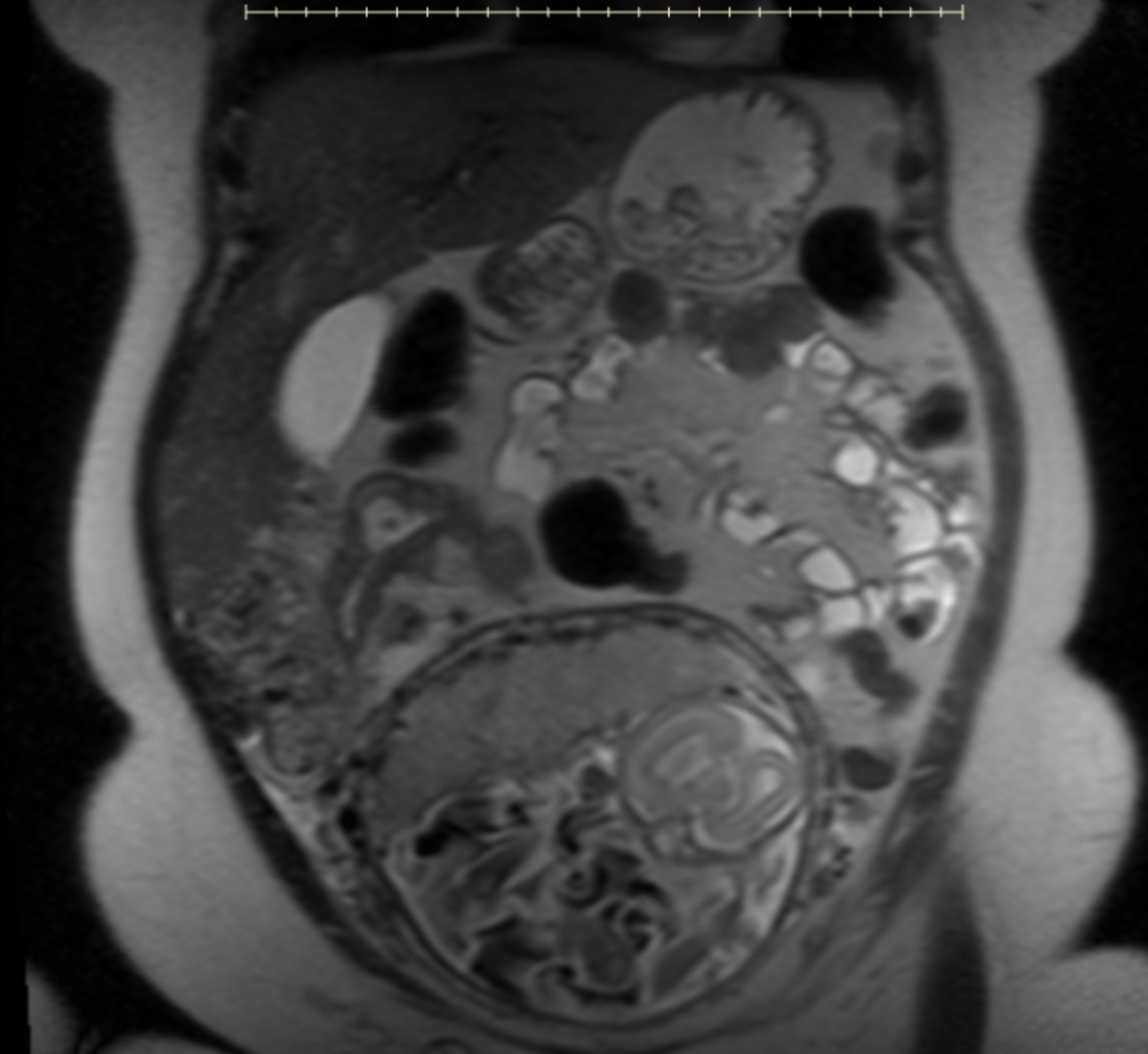
Figure: MRI abdomen with active inflammation involving approximately 5 cm segment of terminal ileum
Disclosures:
Mujtaba Moazzam indicated no relevant financial relationships.
Usman Bin Hameed indicated no relevant financial relationships.
Fady Banno indicated no relevant financial relationships.
Aleena Sharif indicated no relevant financial relationships.
Ayesha Sharif indicated no relevant financial relationships.
Saman Amjad indicated no relevant financial relationships.
Mujtaba Moazzam, MD1, Usman Bin Hameed, MD1, Fady Banno, MD2, Aleena Sharif, MBBS3, Ayesha Sharif, MD4, Saman Amjad, MD1. P5546 - Unpredictable and Unrelenting: A Catastrophic Crohn’s Flare in Mid-Pregnancy Despite Biologic Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
