Tuesday Poster Session
Category: IBD
P5545 - Ileal Tuberculosis Masquerading as Inflammatory Bowel Disease in a Patient With Protein-Losing Enteropathy: A Diagnostic Dilemma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RR
Rubela Ray, MD (she/her/hers)
University of Wyoming
Cheyenne, WY
Presenting Author(s)
Rubela Ray, MD1, Kristina Patel, MD2, Darshankumar Raval, MD3, Syed Ali Uzair Nadeem Bukhari, MD4, Homayoon Lodeen, MD5, Sunny Kumar, MD6
1University of Wyoming, Cheyenne, WY; 2University of Arkansas, Texarkana, AR; 3Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, Youngstown, OH; 4Providence Alaska Medical Center, Anchorage, AK; 5University of California Davis Medical Center, Sacramento, CA; 6Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Ileal tuberculosis (TB) and Crohn’s disease can share overlapping clinical, endoscopic, and histopathological features, posing a diagnostic challenge, particularly in regions endemic to TB. We present a case of a 60-year-old male with ileal ulcers, small bowel obstruction, and protein-losing enteropathy, initially suspected as Crohn’s disease but later diagnosed as intestinal TB.
Case Description/
Methods: A 60-year-old male with type 2 diabetes, hypothyroidism, ischemic heart disease (post-PTCA, post-PPM), and hypertension presented with persistent hiccups, weight loss (~4 kg in 3 weeks), anorexia, abdominal pain, vomiting, and hypoalbuminemia. He had a history of small bowel obstruction involving two ileal segments and post-polypectomy colonic changes.
Labs revealed hypoalbuminemia (2.0–2.6 g/dL), low total protein (4.6 g/dL), and hyponatremia. Imaging showed hepatomegaly. Ileocolonoscopy revealed healed ileal ulcers and cecal scarring. Biopsies showed chronic inflammation with granulomas. GeneXpert for MTB was negative. Based on histology and endemic context, empirical anti-tubercular therapy (AKURIT-T4) was initiated.
He was concurrently treated with mesalamine (Pentasa), albucare powder, and symptom control agents. His symptoms, weight, and albumin levels improved (to 2.6–2.8 g/dL). Protein-losing enteropathy was monitored via urine ACR and 24-hour urinary protein. He remained hemodynamically stable on follow-up.
Discussion: Intestinal TB often mimics Crohn’s disease with ileocecal ulcers and granulomas. However, TB typically presents with transverse ulcers, necrosis, and acute onset. Negative AFB or GeneXpert does not exclude TB, especially in healed disease. Histology and clinical response to therapy guide diagnosis. This patient responded well to ATT within 6–8 weeks.
Protein-losing enteropathy, though uncommon, can arise from chronic ileal inflammation. Persistent hiccups were likely due to diaphragmatic irritation or TB-related motility issues and resolved with treatment.
Conclusion:
In TB-endemic regions, intestinal tuberculosis should remain high on the differential for IBD-like presentations. Empirical ATT may be warranted in equivocal cases with supportive histology and epidemiological context. Accurate differentiation avoids unnecessary immunosuppression.
References:
1. Pulimood AB et al. Intestinal tuberculosis vs Crohn’s disease: Clinical and pathologic overlap. Am J Gastroenterol. 1999;94(2): 369–74.
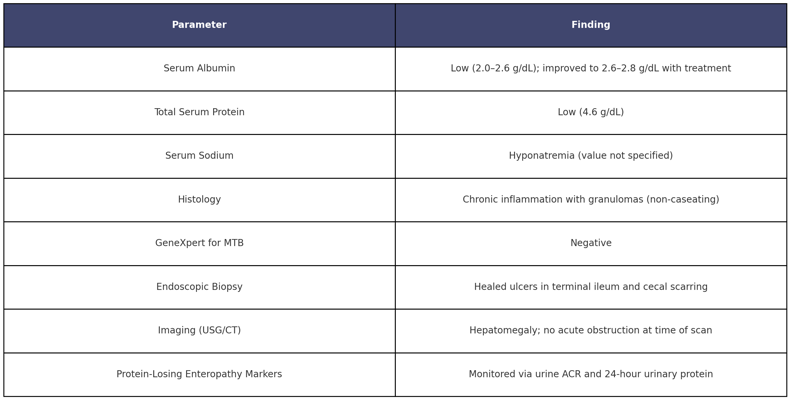
Figure: Case Summary Of Ileal Tuberculosis Mimicking Crohn's Disease
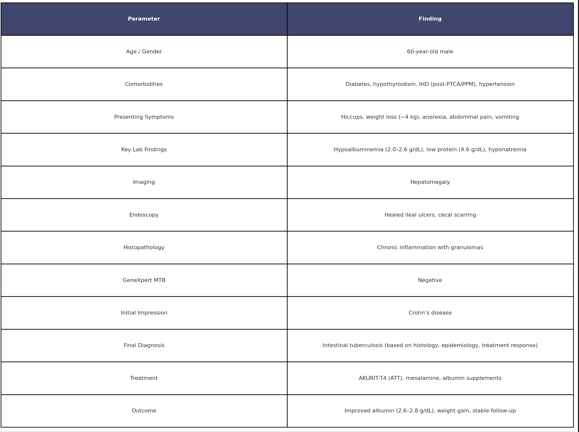
Figure: Laboratory and Pathological Findings of the Patient
Disclosures:
Rubela Ray indicated no relevant financial relationships.
Kristina Patel indicated no relevant financial relationships.
Darshankumar Raval indicated no relevant financial relationships.
Syed Ali Uzair Nadeem Bukhari indicated no relevant financial relationships.
Homayoon Lodeen indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Rubela Ray, MD1, Kristina Patel, MD2, Darshankumar Raval, MD3, Syed Ali Uzair Nadeem Bukhari, MD4, Homayoon Lodeen, MD5, Sunny Kumar, MD6. P5545 - Ileal Tuberculosis Masquerading as Inflammatory Bowel Disease in a Patient With Protein-Losing Enteropathy: A Diagnostic Dilemma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Wyoming, Cheyenne, WY; 2University of Arkansas, Texarkana, AR; 3Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, Youngstown, OH; 4Providence Alaska Medical Center, Anchorage, AK; 5University of California Davis Medical Center, Sacramento, CA; 6Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Ileal tuberculosis (TB) and Crohn’s disease can share overlapping clinical, endoscopic, and histopathological features, posing a diagnostic challenge, particularly in regions endemic to TB. We present a case of a 60-year-old male with ileal ulcers, small bowel obstruction, and protein-losing enteropathy, initially suspected as Crohn’s disease but later diagnosed as intestinal TB.
Case Description/
Methods: A 60-year-old male with type 2 diabetes, hypothyroidism, ischemic heart disease (post-PTCA, post-PPM), and hypertension presented with persistent hiccups, weight loss (~4 kg in 3 weeks), anorexia, abdominal pain, vomiting, and hypoalbuminemia. He had a history of small bowel obstruction involving two ileal segments and post-polypectomy colonic changes.
Labs revealed hypoalbuminemia (2.0–2.6 g/dL), low total protein (4.6 g/dL), and hyponatremia. Imaging showed hepatomegaly. Ileocolonoscopy revealed healed ileal ulcers and cecal scarring. Biopsies showed chronic inflammation with granulomas. GeneXpert for MTB was negative. Based on histology and endemic context, empirical anti-tubercular therapy (AKURIT-T4) was initiated.
He was concurrently treated with mesalamine (Pentasa), albucare powder, and symptom control agents. His symptoms, weight, and albumin levels improved (to 2.6–2.8 g/dL). Protein-losing enteropathy was monitored via urine ACR and 24-hour urinary protein. He remained hemodynamically stable on follow-up.
Discussion: Intestinal TB often mimics Crohn’s disease with ileocecal ulcers and granulomas. However, TB typically presents with transverse ulcers, necrosis, and acute onset. Negative AFB or GeneXpert does not exclude TB, especially in healed disease. Histology and clinical response to therapy guide diagnosis. This patient responded well to ATT within 6–8 weeks.
Protein-losing enteropathy, though uncommon, can arise from chronic ileal inflammation. Persistent hiccups were likely due to diaphragmatic irritation or TB-related motility issues and resolved with treatment.
Conclusion:
In TB-endemic regions, intestinal tuberculosis should remain high on the differential for IBD-like presentations. Empirical ATT may be warranted in equivocal cases with supportive histology and epidemiological context. Accurate differentiation avoids unnecessary immunosuppression.
References:
1. Pulimood AB et al. Intestinal tuberculosis vs Crohn’s disease: Clinical and pathologic overlap. Am J Gastroenterol. 1999;94(2): 369–74.
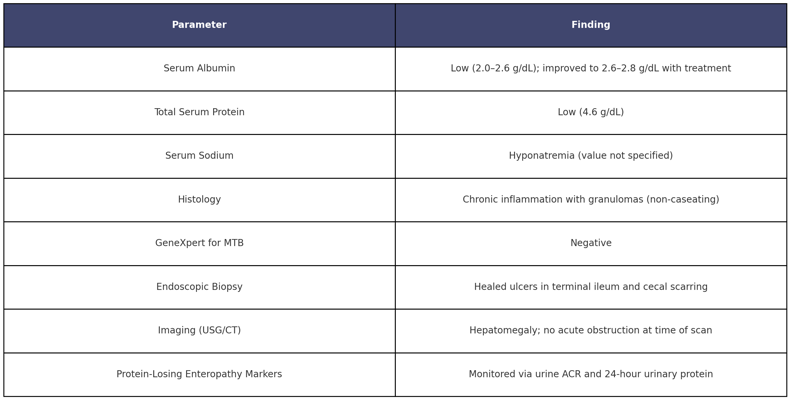
Figure: Case Summary Of Ileal Tuberculosis Mimicking Crohn's Disease
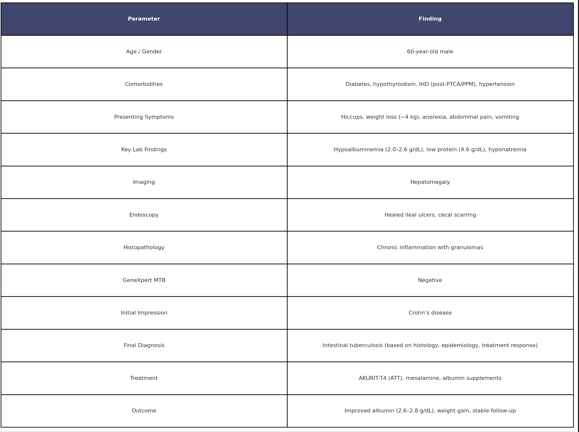
Figure: Laboratory and Pathological Findings of the Patient
Disclosures:
Rubela Ray indicated no relevant financial relationships.
Kristina Patel indicated no relevant financial relationships.
Darshankumar Raval indicated no relevant financial relationships.
Syed Ali Uzair Nadeem Bukhari indicated no relevant financial relationships.
Homayoon Lodeen indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Rubela Ray, MD1, Kristina Patel, MD2, Darshankumar Raval, MD3, Syed Ali Uzair Nadeem Bukhari, MD4, Homayoon Lodeen, MD5, Sunny Kumar, MD6. P5545 - Ileal Tuberculosis Masquerading as Inflammatory Bowel Disease in a Patient With Protein-Losing Enteropathy: A Diagnostic Dilemma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
