Tuesday Poster Session
Category: IBD
P5539 - Tracheitis: A Rare Pulmonary Manifestation of Ulcerative Colitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Carter Schulz, MD
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Award: ACG Presidential Poster Award
Carter Schulz, MD, Luis Zuniga, DO, Zach Vinton, DO, Casey Behnke, MD
University of Nebraska Medical Center, Omaha, NE
Introduction: Ulcerative colitis (UC) is an idiopathic, multi-system, inflammatory disease leading to mucosal friability and ulcers. UC commonly affects the distal colon and rectum, but extra-intestinal manifestations (EIMs) can be seen in other organ systems. Pulmonary involvement can involve any part of the respiratory system, but tracheitis is especially uncommon. We present a rare case of UC presenting with tracheitis.
Case Description/
Methods: A 24-year-old male with a history of psoriasis presented to the emergency department with one month of hematochezia, diarrhea with up to 14 stools per day, and 30 pounds of weight loss. Six months prior, he had hematochezia attributed to infectious colitis. He now endorsed a cough, pleuritic chest pain, and night sweats. Labs were notable for leukocytosis, anemia, and elevated inflammatory markers. Chest CT showed tracheal inflammation and ground glass nodules around the right lung. This prompted bronchoscopy, demonstrating friable lesions of the true vocal cords with diffuse friable tracheal tissue. An ulcerated, partially obstructive, polypoid lesion was seen at the level of the carina (Figure 1). Biopsy of the trachea showed fibrin with acute and chronic inflammation. Oncologic workup was negative.
Colonoscopy revealed pancolitis with a decrease in disease past the hepatic flexure (Figure 2). Biopsy showed evidence of active disease with cryptitis and crypt abscess formation as well as chronic mucosal injury with basal lymphoplasma cytosis and crypt distortion. He was diagnosed with UC with associated tracheitis and was started on systemic and inhaled corticosteroids, resulting in rapid improvement. He was discharged on prednisone with a plan for future infliximab therapy.
Discussion: EIM of IBD such as arthritis and uveitis are common. Pulmonary involvement is less common, and tracheitis is incredibly rare, with only a handful of case reports described. Tracheal involvement commonly presents after disease onset, but can happen prior to bowel involvement or years after pancolectomy. Maintaining suspicion for pulmonary EIM is important in anyone with a history of IBD.
Ulcerative colitis associated tracheitis can be suspected based on findings from bronchoscopy, biopsy, and pulmonary function testing. Respiratory disease tends to respond very well to systemic steroids and inhaled corticosteroids. Azathioprine has been used as a steroid-sparing agent, but biologic drugs like infliximab have been reported to be successful for lung involvement in these patients.
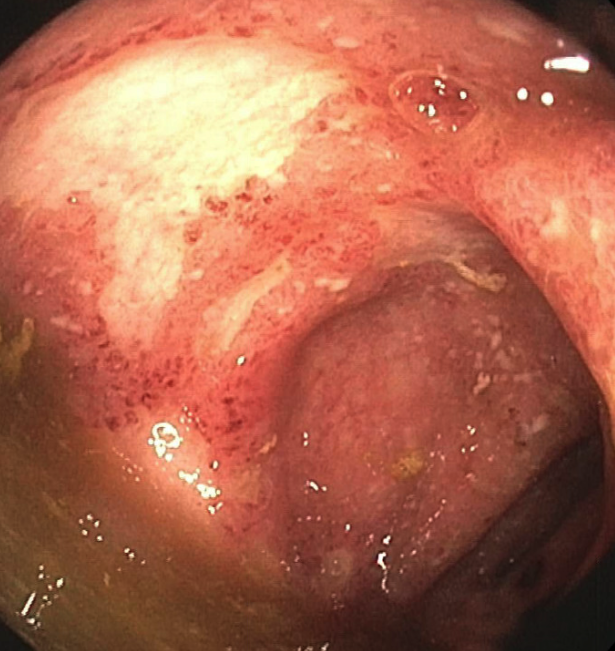
Figure: Figure 1: trachea at the level of the carina. Diffuse erythema and edema were seen in the trachea along with patchy areas of friable granulation tissue. A partially (20%) obstructing, infiltrative, polypoid, submucosal and ulcerated lesion was found in the trachea at the carina.
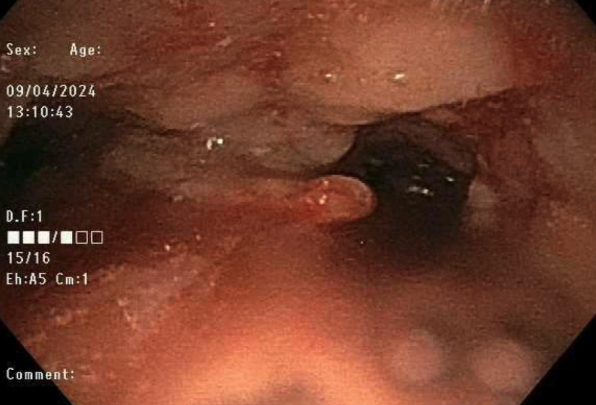
Figure: Figure 2: descending colon. There were diffuse moderate mucosal changes of pancolitis characterized by congestion, erosions, erythema, friability, granularity, loss of vascularity, and shallow ulcerations.
Disclosures:
Carter Schulz indicated no relevant financial relationships.
Luis Zuniga indicated no relevant financial relationships.
Zach Vinton indicated no relevant financial relationships.
Casey Behnke indicated no relevant financial relationships.
Carter Schulz, MD, Luis Zuniga, DO, Zach Vinton, DO, Casey Behnke, MD. P5539 - Tracheitis: A Rare Pulmonary Manifestation of Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Carter Schulz, MD, Luis Zuniga, DO, Zach Vinton, DO, Casey Behnke, MD
University of Nebraska Medical Center, Omaha, NE
Introduction: Ulcerative colitis (UC) is an idiopathic, multi-system, inflammatory disease leading to mucosal friability and ulcers. UC commonly affects the distal colon and rectum, but extra-intestinal manifestations (EIMs) can be seen in other organ systems. Pulmonary involvement can involve any part of the respiratory system, but tracheitis is especially uncommon. We present a rare case of UC presenting with tracheitis.
Case Description/
Methods: A 24-year-old male with a history of psoriasis presented to the emergency department with one month of hematochezia, diarrhea with up to 14 stools per day, and 30 pounds of weight loss. Six months prior, he had hematochezia attributed to infectious colitis. He now endorsed a cough, pleuritic chest pain, and night sweats. Labs were notable for leukocytosis, anemia, and elevated inflammatory markers. Chest CT showed tracheal inflammation and ground glass nodules around the right lung. This prompted bronchoscopy, demonstrating friable lesions of the true vocal cords with diffuse friable tracheal tissue. An ulcerated, partially obstructive, polypoid lesion was seen at the level of the carina (Figure 1). Biopsy of the trachea showed fibrin with acute and chronic inflammation. Oncologic workup was negative.
Colonoscopy revealed pancolitis with a decrease in disease past the hepatic flexure (Figure 2). Biopsy showed evidence of active disease with cryptitis and crypt abscess formation as well as chronic mucosal injury with basal lymphoplasma cytosis and crypt distortion. He was diagnosed with UC with associated tracheitis and was started on systemic and inhaled corticosteroids, resulting in rapid improvement. He was discharged on prednisone with a plan for future infliximab therapy.
Discussion: EIM of IBD such as arthritis and uveitis are common. Pulmonary involvement is less common, and tracheitis is incredibly rare, with only a handful of case reports described. Tracheal involvement commonly presents after disease onset, but can happen prior to bowel involvement or years after pancolectomy. Maintaining suspicion for pulmonary EIM is important in anyone with a history of IBD.
Ulcerative colitis associated tracheitis can be suspected based on findings from bronchoscopy, biopsy, and pulmonary function testing. Respiratory disease tends to respond very well to systemic steroids and inhaled corticosteroids. Azathioprine has been used as a steroid-sparing agent, but biologic drugs like infliximab have been reported to be successful for lung involvement in these patients.
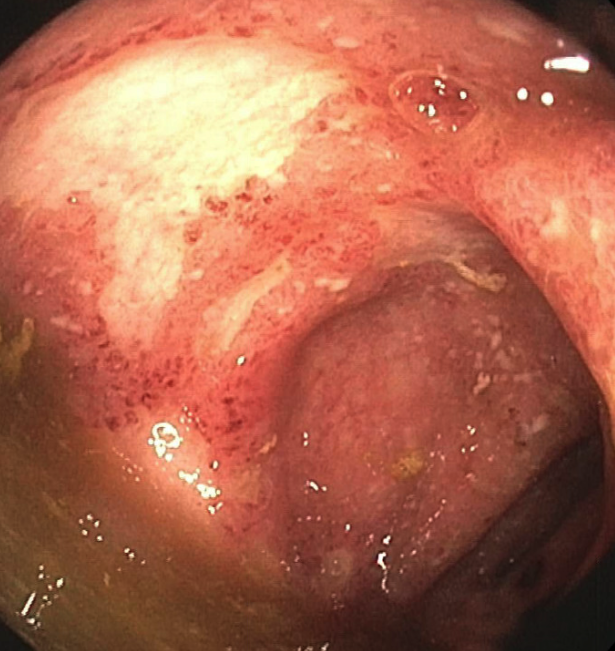
Figure: Figure 1: trachea at the level of the carina. Diffuse erythema and edema were seen in the trachea along with patchy areas of friable granulation tissue. A partially (20%) obstructing, infiltrative, polypoid, submucosal and ulcerated lesion was found in the trachea at the carina.
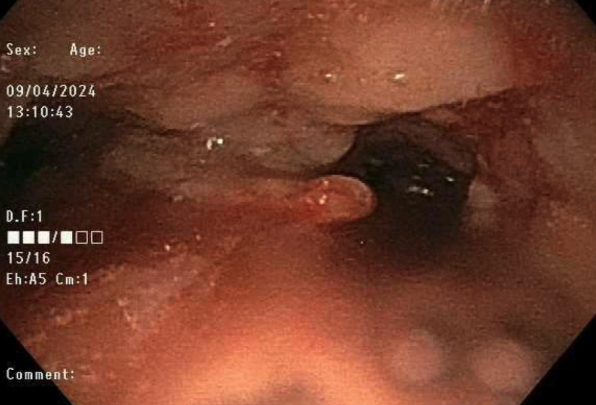
Figure: Figure 2: descending colon. There were diffuse moderate mucosal changes of pancolitis characterized by congestion, erosions, erythema, friability, granularity, loss of vascularity, and shallow ulcerations.
Disclosures:
Carter Schulz indicated no relevant financial relationships.
Luis Zuniga indicated no relevant financial relationships.
Zach Vinton indicated no relevant financial relationships.
Casey Behnke indicated no relevant financial relationships.
Carter Schulz, MD, Luis Zuniga, DO, Zach Vinton, DO, Casey Behnke, MD. P5539 - Tracheitis: A Rare Pulmonary Manifestation of Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

