Tuesday Poster Session
Category: IBD
P5538 - Mood Dysregulation in a Middle-Aged Woman With Longstanding IBS: A Case Reflecting Gut-Brain-Microbiome Axis Disruption
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Fahmida Shaik, MBBS (she/her/hers)
Gandhi Medical College & Hospital
San Jose, CA
Presenting Author(s)
Tanishq Kesani, MD1, Deepthi Chintala, MBB2, Fahmida Shaik, MBBSS3, Usman Saif Mohammed, MBBS4, Sai Prashanthi Varakala, 5, Deekshithreddy Challa, MBBS6, Riya Varughese Raju, MBBS7
1Yuma Regional Medical Center, Yuma, AZ; 2NRI medical college, Mangalagiri, Guntur, Andhra Pradesh, India; 3Gandhi Medical College & Hospital, San Jose, CA; 4Dr. YSR University of Health Sciences, Chirala, Andhra Pradesh, India; 5Osmania Medical College, Dallas, TX; 6Nimra institute of medical sciences, Hanamkonda, Warangal, Telangana, India; 7Maharajah's Institute of Medical Sciences, Springfield, IL
Introduction: Irritable Bowel Syndrome (IBS) is a prevalent functional gastrointestinal disorder often associated with mood disturbances such as depression, anxiety, and fatigue. This overlap can significantly impair quality of life and increase healthcare use. Recent insights into the gut-brain-microbiome axis have identified it as a key mediator in this bidirectional relationship. Dysbiosis—altered gut microbial composition—has been linked to visceral hypersensitivity, immune activation, and neuroinflammation. Additionally, microbial by-products like short-chain fatty acids (SCFAs) and gut-derived serotonin influence both enteric and central nervous systems, impacting mood and stress regulation. We present a case that highlights the need for integrated care in managing IBS with psychological comorbidity.
Case Description/
Methods: A 45-year-old woman with a 10-year history of IBS-M presented with worsening bloating, alternating bowel habits, and new-onset mood symptoms including irritability, fatigue, low mood, and social withdrawal. She reported a clear link between emotional distress and GI flares. She had no psychiatric history. Physical exam and routine labs were normal. Mental health screening showed PHQ-9 = 13 (moderate depression) and GAD-7 = 9 (mild anxiety). Stool microbiome testing revealed reduced alpha-diversity, decreased Bifidobacterium and Lactobacillus, and elevated Ruminococcus gnavus, a species associated with mucosal inflammation. Treatment included sertraline 50 mg daily, a low FODMAP diet, targeted probiotics, and gut-directed cognitive behavioral therapy (CBT). At 12 weeks, her PHQ-9 dropped to 6, with improved GI stability and emotional well-being.
Discussion: This case demonstrates how gut microbial imbalance may contribute to mood symptoms in IBS through disrupted SCFA signaling, vagal dysfunction, and immune activation. The patient’s improvement with combined psychotropic, dietary, and microbiome-targeted interventions supports a growing body of evidence favoring multidisciplinary care in IBS. A personalized, mechanism-driven approach can lead to more effective management of both GI and psychological symptoms in functional bowel disorders.
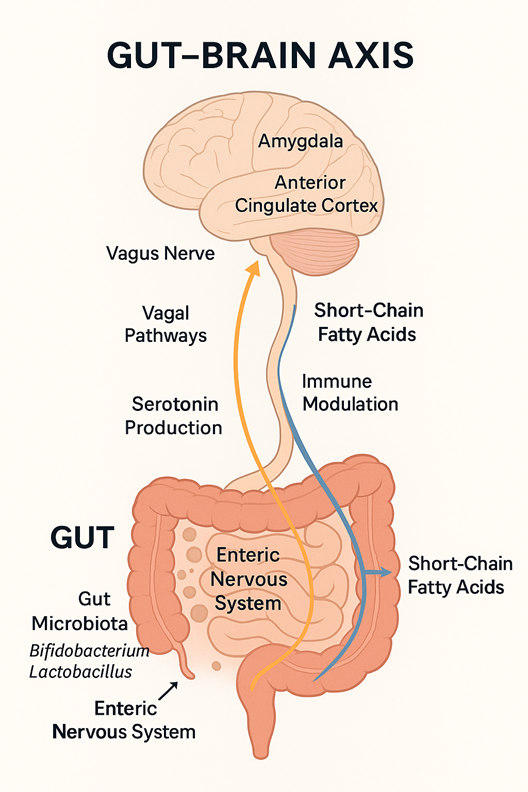
Figure: Figure 1: Stool Microbiome Composition (Pre vs. Post-Intervention)
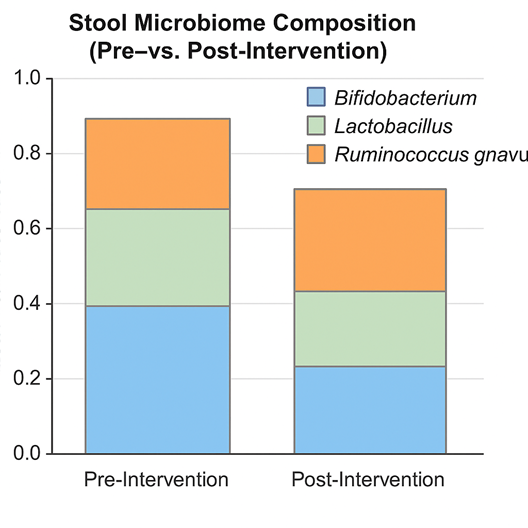
Figure: Figure 2: Gut-Brain Axis Illustration
Disclosures:
Tanishq Kesani indicated no relevant financial relationships.
Deepthi Chintala indicated no relevant financial relationships.
Fahmida Shaik indicated no relevant financial relationships.
Usman Saif Mohammed indicated no relevant financial relationships.
Sai Prashanthi Varakala indicated no relevant financial relationships.
Deekshithreddy Challa indicated no relevant financial relationships.
Riya Varughese Raju indicated no relevant financial relationships.
Tanishq Kesani, MD1, Deepthi Chintala, MBBS2, Fahmida Shaik, MBBS3, Usman Saif Mohammed, MBBS4, Sai Prashanthi Varakala, 5, Deekshithreddy Challa, MBBS6, Riya Varughese Raju, MBBS7. P5538 - Mood Dysregulation in a Middle-Aged Woman With Longstanding IBS: A Case Reflecting Gut-Brain-Microbiome Axis Disruption, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yuma Regional Medical Center, Yuma, AZ; 2NRI medical college, Mangalagiri, Guntur, Andhra Pradesh, India; 3Gandhi Medical College & Hospital, San Jose, CA; 4Dr. YSR University of Health Sciences, Chirala, Andhra Pradesh, India; 5Osmania Medical College, Dallas, TX; 6Nimra institute of medical sciences, Hanamkonda, Warangal, Telangana, India; 7Maharajah's Institute of Medical Sciences, Springfield, IL
Introduction: Irritable Bowel Syndrome (IBS) is a prevalent functional gastrointestinal disorder often associated with mood disturbances such as depression, anxiety, and fatigue. This overlap can significantly impair quality of life and increase healthcare use. Recent insights into the gut-brain-microbiome axis have identified it as a key mediator in this bidirectional relationship. Dysbiosis—altered gut microbial composition—has been linked to visceral hypersensitivity, immune activation, and neuroinflammation. Additionally, microbial by-products like short-chain fatty acids (SCFAs) and gut-derived serotonin influence both enteric and central nervous systems, impacting mood and stress regulation. We present a case that highlights the need for integrated care in managing IBS with psychological comorbidity.
Case Description/
Methods: A 45-year-old woman with a 10-year history of IBS-M presented with worsening bloating, alternating bowel habits, and new-onset mood symptoms including irritability, fatigue, low mood, and social withdrawal. She reported a clear link between emotional distress and GI flares. She had no psychiatric history. Physical exam and routine labs were normal. Mental health screening showed PHQ-9 = 13 (moderate depression) and GAD-7 = 9 (mild anxiety). Stool microbiome testing revealed reduced alpha-diversity, decreased Bifidobacterium and Lactobacillus, and elevated Ruminococcus gnavus, a species associated with mucosal inflammation. Treatment included sertraline 50 mg daily, a low FODMAP diet, targeted probiotics, and gut-directed cognitive behavioral therapy (CBT). At 12 weeks, her PHQ-9 dropped to 6, with improved GI stability and emotional well-being.
Discussion: This case demonstrates how gut microbial imbalance may contribute to mood symptoms in IBS through disrupted SCFA signaling, vagal dysfunction, and immune activation. The patient’s improvement with combined psychotropic, dietary, and microbiome-targeted interventions supports a growing body of evidence favoring multidisciplinary care in IBS. A personalized, mechanism-driven approach can lead to more effective management of both GI and psychological symptoms in functional bowel disorders.
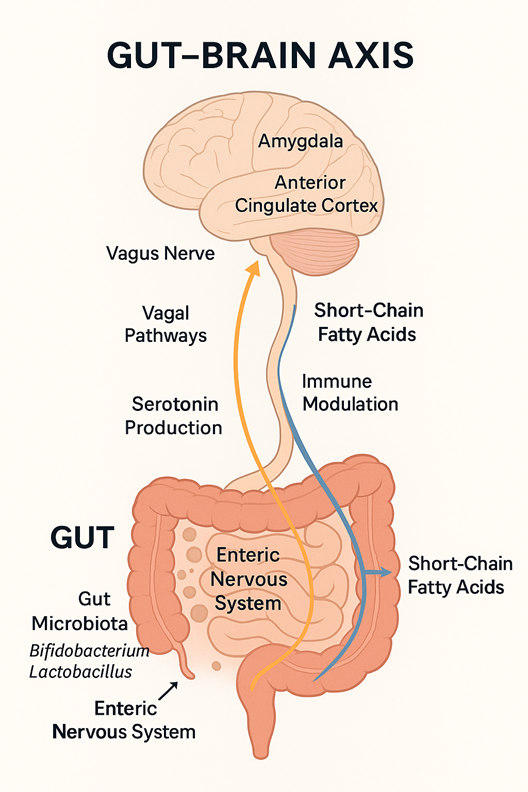
Figure: Figure 1: Stool Microbiome Composition (Pre vs. Post-Intervention)
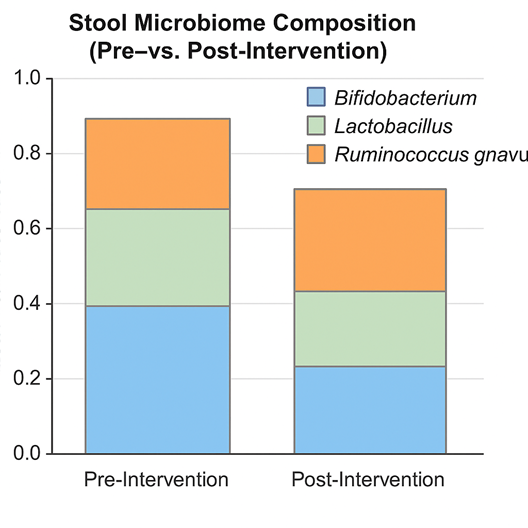
Figure: Figure 2: Gut-Brain Axis Illustration
Disclosures:
Tanishq Kesani indicated no relevant financial relationships.
Deepthi Chintala indicated no relevant financial relationships.
Fahmida Shaik indicated no relevant financial relationships.
Usman Saif Mohammed indicated no relevant financial relationships.
Sai Prashanthi Varakala indicated no relevant financial relationships.
Deekshithreddy Challa indicated no relevant financial relationships.
Riya Varughese Raju indicated no relevant financial relationships.
Tanishq Kesani, MD1, Deepthi Chintala, MBBS2, Fahmida Shaik, MBBS3, Usman Saif Mohammed, MBBS4, Sai Prashanthi Varakala, 5, Deekshithreddy Challa, MBBS6, Riya Varughese Raju, MBBS7. P5538 - Mood Dysregulation in a Middle-Aged Woman With Longstanding IBS: A Case Reflecting Gut-Brain-Microbiome Axis Disruption, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
