Tuesday Poster Session
Category: IBD
P5533 - Rectal Lymphoma in an Ulcerative Colitis Patient on Anti-Tumor Necrosis Factor Therapy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Claire Beamish, MD
Dartmouth Hitchcock Medical Center
Lebanon, NH
Presenting Author(s)
Claire Beamish, MD, Michael Winter, MD
Dartmouth Hitchcock Medical Center, Lebanon, NH
Introduction: The absolute risk of IBD and lymphoma is unclear. Some data suggests that IBD portends an increased risk for lymphoma, whereas other research proposes that IBD treatment itself is the primary driver of increased lymphoma risk. The association between lymphomas and immunomodulators has been well established for several decades. However, the association between lymphomas and anti-tumor necrosis factor (anti-TNF) therapy is uncertain. Research into the relationship between lymphomas and anti-TNF agents is limited as many patients on anti-TNF medications are on concurrent or prior immunomodulators. We present a case of a 47-year-old male with a history of ulcerative proctitis who developed rectal diffuse large B-cell lymphoma (DLBCL) six months after initiation of anti-TNF therapy without any prior history of immunomodulator exposure.
Case Description/
Methods: A 47-year-old man diagnosed with ulcerative proctitis two years prior on mesalamine presented to clinic for worsening tenesmus, urgency, and hematochezia. A flexible sigmoidoscopy was obtained and biopsies showed chronic colitis in the distal rectum. Patient was transitioned to adalimumab for suboptimal response to current therapy. Four months later, patient re-presented to clinic for refractory abdominal cramping necessitating a repeat colonoscopy for restaging of his IBD (Figure 1). Rectal biopsies showed lymphoplasmacytic infiltrates consistent with DLBCL. Patient’s adalimumab was immediately stopped. Patient completed a four week course of rituximab. Following completion of chemotherapy, repeat colonoscopy was performed with rectal biopsies showing no evidence of disease. Repeat PET scan also confirmed resolution of previously active lymphoma
Discussion: This case is unique in that it highlights an apparent anti-TNF induced lymphoma in the absence of any confounding immunomodulator therapy. Further, the location of the lymphoma and time course are both highly unusual. Given that the lymphoma was localized to the same area affected by the patient’s underlying ulcerative proctitis, it is unclear what degree recurrent inflammation from IBD played in the pathogenesis. Ultimately, this case highlights the need for ongoing research into assessing the lymphoma risk in IBD patients with prior or concomitant usage of anti-TNF therapy while minimizing confounding variables and potential bias.
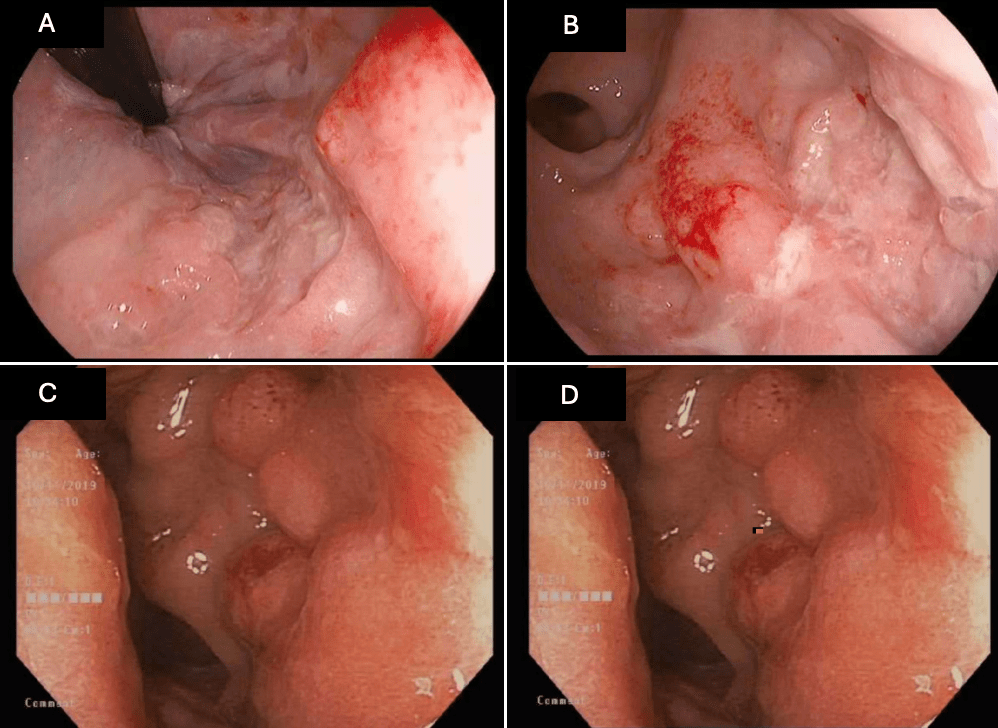
Figure: Figure 1. Slides A and B demonstrate rectum prior to anti-TNF induction; slides C and D demonstrate rectum after anti-TNF therapy.
Disclosures:
Claire Beamish indicated no relevant financial relationships.
Michael Winter indicated no relevant financial relationships.
Claire Beamish, MD, Michael Winter, MD. P5533 - Rectal Lymphoma in an Ulcerative Colitis Patient on Anti-Tumor Necrosis Factor Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Dartmouth Hitchcock Medical Center, Lebanon, NH
Introduction: The absolute risk of IBD and lymphoma is unclear. Some data suggests that IBD portends an increased risk for lymphoma, whereas other research proposes that IBD treatment itself is the primary driver of increased lymphoma risk. The association between lymphomas and immunomodulators has been well established for several decades. However, the association between lymphomas and anti-tumor necrosis factor (anti-TNF) therapy is uncertain. Research into the relationship between lymphomas and anti-TNF agents is limited as many patients on anti-TNF medications are on concurrent or prior immunomodulators. We present a case of a 47-year-old male with a history of ulcerative proctitis who developed rectal diffuse large B-cell lymphoma (DLBCL) six months after initiation of anti-TNF therapy without any prior history of immunomodulator exposure.
Case Description/
Methods: A 47-year-old man diagnosed with ulcerative proctitis two years prior on mesalamine presented to clinic for worsening tenesmus, urgency, and hematochezia. A flexible sigmoidoscopy was obtained and biopsies showed chronic colitis in the distal rectum. Patient was transitioned to adalimumab for suboptimal response to current therapy. Four months later, patient re-presented to clinic for refractory abdominal cramping necessitating a repeat colonoscopy for restaging of his IBD (Figure 1). Rectal biopsies showed lymphoplasmacytic infiltrates consistent with DLBCL. Patient’s adalimumab was immediately stopped. Patient completed a four week course of rituximab. Following completion of chemotherapy, repeat colonoscopy was performed with rectal biopsies showing no evidence of disease. Repeat PET scan also confirmed resolution of previously active lymphoma
Discussion: This case is unique in that it highlights an apparent anti-TNF induced lymphoma in the absence of any confounding immunomodulator therapy. Further, the location of the lymphoma and time course are both highly unusual. Given that the lymphoma was localized to the same area affected by the patient’s underlying ulcerative proctitis, it is unclear what degree recurrent inflammation from IBD played in the pathogenesis. Ultimately, this case highlights the need for ongoing research into assessing the lymphoma risk in IBD patients with prior or concomitant usage of anti-TNF therapy while minimizing confounding variables and potential bias.
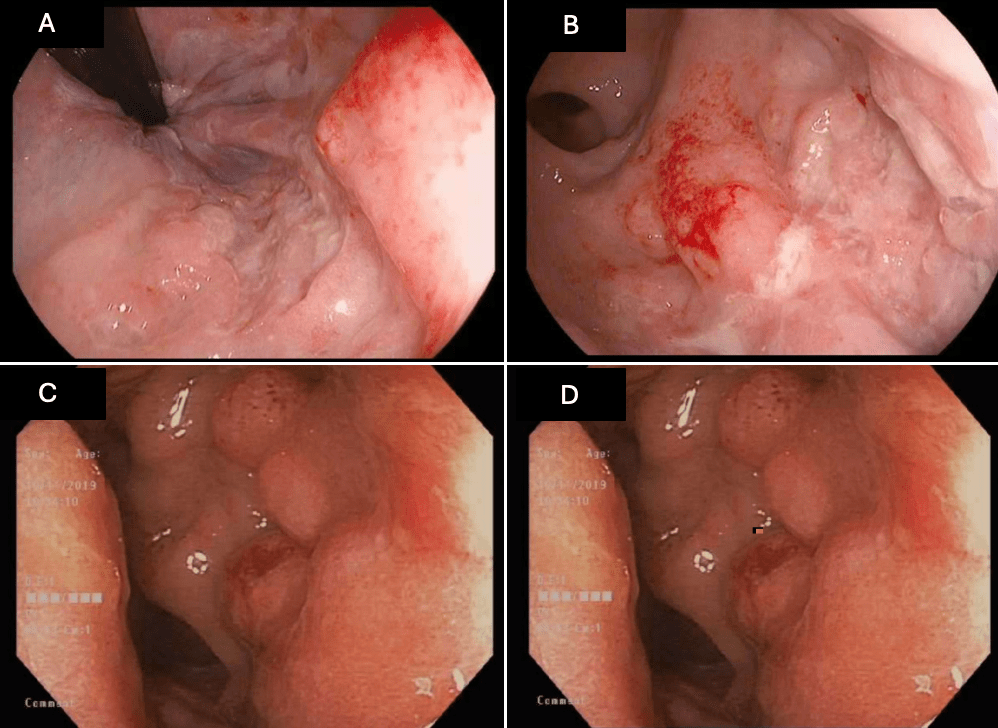
Figure: Figure 1. Slides A and B demonstrate rectum prior to anti-TNF induction; slides C and D demonstrate rectum after anti-TNF therapy.
Disclosures:
Claire Beamish indicated no relevant financial relationships.
Michael Winter indicated no relevant financial relationships.
Claire Beamish, MD, Michael Winter, MD. P5533 - Rectal Lymphoma in an Ulcerative Colitis Patient on Anti-Tumor Necrosis Factor Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
