Tuesday Poster Session
Category: IBD
P5524 - Eosinophilic Colitis Following Roux-en-Y Gastric Bypass: A Rare Case of Postoperative Eosinophilic Gastrointestinal Disease in an Atopic Adult
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Isaac Giovannie, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Atsushi Sakuraba, MD, PhD1, Maham Lodhi, MD1, Joseph Frasca, MD1, Veena Nannegari, MD2
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Center, Chicagoii, IL
Introduction: Eosinophilic colitis (EC) is a rare inflammatory condition, with an estimated prevalence of less than 1–2 cases per 100,000 individuals, defined by dense eosinophilic infiltration of the colonic mucosa without secondary causes. It’s most often linked to food allergies, autoimmune conditions, medications, or parasitic infections. EC is particularly uncommon in adults and remains poorly described in the postoperative setting. We present a biopsy-confirmed case of EC developing shortly after Roux-en-Y gastric bypass, suggesting that gastrointestinal surgery may act as a physiological trigger for eosinophilic gastrointestinal disease in predisposed individuals.
Case Description/
Methods: A 30-year-old woman with morbid obesity and multiple allergies (latex, rubber, lidocaine, bee venom) underwent uncomplicated RYGB but developed abdominal pain, nausea, vomiting, and food intolerance within a week, leading to hospitalization for severe constipation; imaging showed fecal stasis and stercoral colitis, and sigmoidoscopy revealed mucosal erythema and ulcers, with biopsies showing mild active colitis without chronicity. She was discharged on Miralax but was lost to follow-up, later returning with a 10-lb weight loss, nausea, and peripheral eosinophilia (26%); colonoscopy showed mild sigmoid erythema, and biopsies from the right, left, and sigmoid colon demonstrated marked eosinophilic infiltration of the lamina propria—124, 141, and 115 eosinophils per HPF, respectively. Diagnosed with EC, she was started on prednisone but couldn’t tolerate oral steroids due to nausea, requiring hospitalization and IV corticosteroids, which led to clinical improvement, resolution of eosinophilia, and normal follow-up colonoscopy.
Discussion: Post-RYGB EC is rare but clinically important. Rather than a direct surgical complication, it may reflect immune dysregulation triggered by postoperative stress, altered antigen exposure, or microbiota shifts. Diagnosis is challenging due to patchy disease and nonspecific or absent endoscopic findings. Diagnostic criteria include GI symptoms, exclusion of secondary causes, and histologic eosinophil counts >100/HPF (right colon), >84/HPF (transverse), or >64/HPF (left). False negatives on initial biopsy are common, highlighting the need for repeat sampling. While most cases respond to corticosteroids, TNF-α inhibitors may help in refractory disease. This case highlights the importance of considering EGIDs in post-bariatric patients with persistent GI symptoms and eosinophilia.
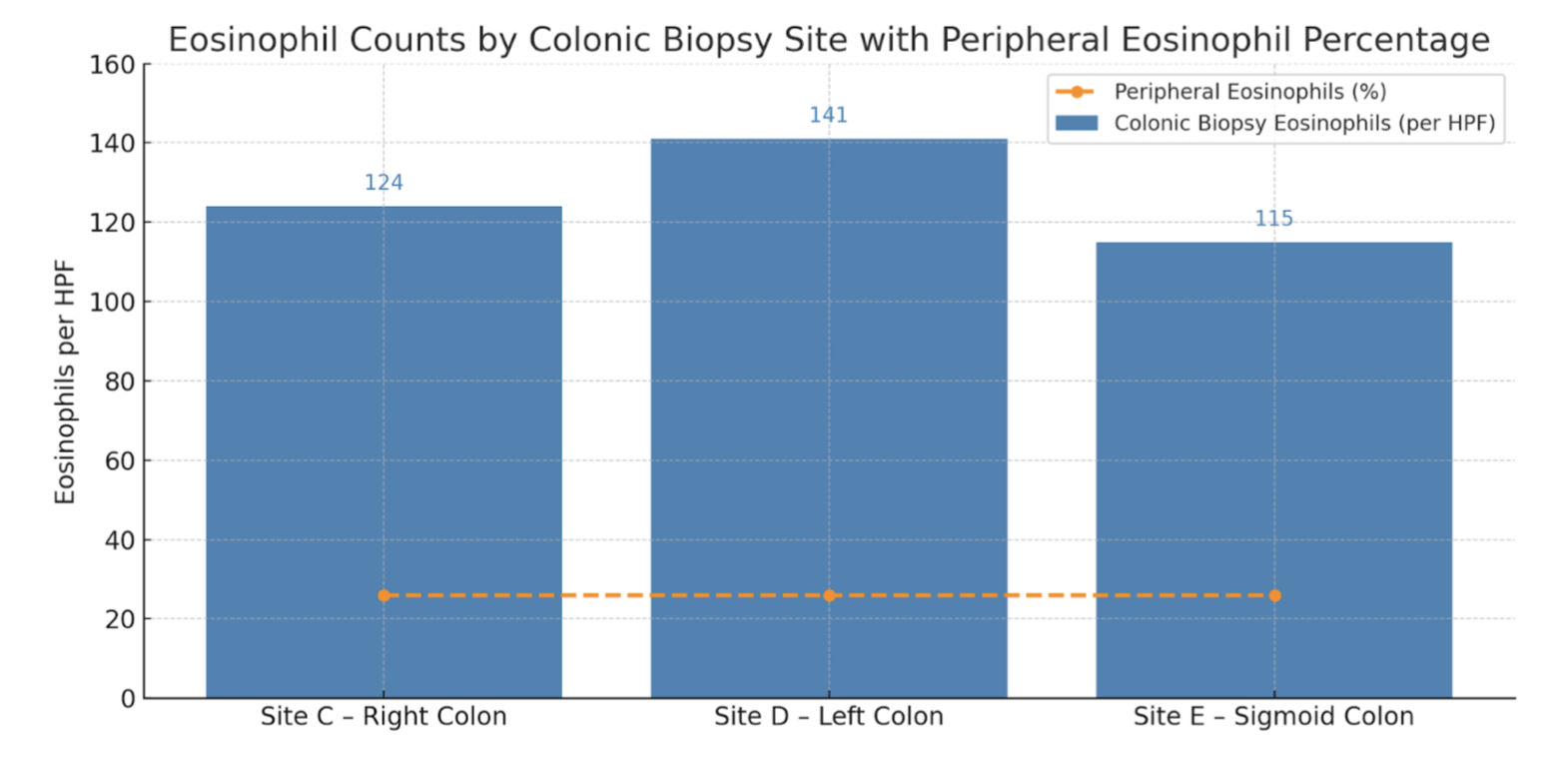
Figure: Table 1: Eosinophil counts from colonic biopsy sites and peripheral blood: Colonic biopsies revealed marked eosinophilic infiltration in the lamina propria: Site C – Right Colon (124 eosinophils/HPF), Site D – Left Colon (141 eosinophils/HPF), and Site E – Sigmoid Colon (115 eosinophils/HPF). A horizontal dashed line represents peripheral eosinophilia (26%), highlighting the coexistence of systemic and tissue-level eosinophilic inflammation. These findings supported the diagnosis of eosinophilic colitis.
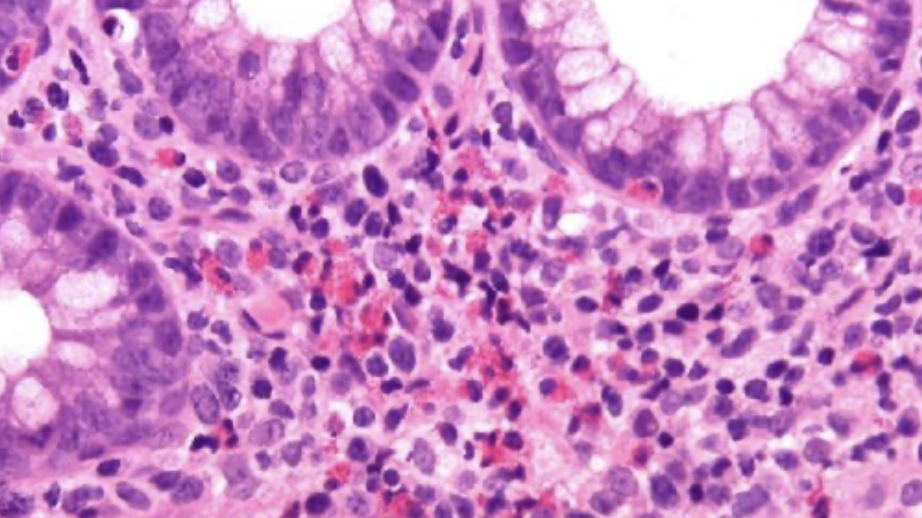
Figure: Image 1: Eosinophilic colitis. Presence of numerous eosinophils, in aggregate and sheets in the lamina propria and infiltrating the crypt epithelium. H&E magnification 40x.
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Zoe Post indicated no relevant financial relationships.
Atsushi Sakuraba indicated no relevant financial relationships.
Maham Lodhi indicated no relevant financial relationships.
Joseph Frasca indicated no relevant financial relationships.
Veena Nannegari indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Atsushi Sakuraba, MD, PhD1, Maham Lodhi, MD1, Joseph Frasca, MD1, Veena Nannegari, MD2. P5524 - Eosinophilic Colitis Following Roux-en-Y Gastric Bypass: A Rare Case of Postoperative Eosinophilic Gastrointestinal Disease in an Atopic Adult, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Center, Chicagoii, IL
Introduction: Eosinophilic colitis (EC) is a rare inflammatory condition, with an estimated prevalence of less than 1–2 cases per 100,000 individuals, defined by dense eosinophilic infiltration of the colonic mucosa without secondary causes. It’s most often linked to food allergies, autoimmune conditions, medications, or parasitic infections. EC is particularly uncommon in adults and remains poorly described in the postoperative setting. We present a biopsy-confirmed case of EC developing shortly after Roux-en-Y gastric bypass, suggesting that gastrointestinal surgery may act as a physiological trigger for eosinophilic gastrointestinal disease in predisposed individuals.
Case Description/
Methods: A 30-year-old woman with morbid obesity and multiple allergies (latex, rubber, lidocaine, bee venom) underwent uncomplicated RYGB but developed abdominal pain, nausea, vomiting, and food intolerance within a week, leading to hospitalization for severe constipation; imaging showed fecal stasis and stercoral colitis, and sigmoidoscopy revealed mucosal erythema and ulcers, with biopsies showing mild active colitis without chronicity. She was discharged on Miralax but was lost to follow-up, later returning with a 10-lb weight loss, nausea, and peripheral eosinophilia (26%); colonoscopy showed mild sigmoid erythema, and biopsies from the right, left, and sigmoid colon demonstrated marked eosinophilic infiltration of the lamina propria—124, 141, and 115 eosinophils per HPF, respectively. Diagnosed with EC, she was started on prednisone but couldn’t tolerate oral steroids due to nausea, requiring hospitalization and IV corticosteroids, which led to clinical improvement, resolution of eosinophilia, and normal follow-up colonoscopy.
Discussion: Post-RYGB EC is rare but clinically important. Rather than a direct surgical complication, it may reflect immune dysregulation triggered by postoperative stress, altered antigen exposure, or microbiota shifts. Diagnosis is challenging due to patchy disease and nonspecific or absent endoscopic findings. Diagnostic criteria include GI symptoms, exclusion of secondary causes, and histologic eosinophil counts >100/HPF (right colon), >84/HPF (transverse), or >64/HPF (left). False negatives on initial biopsy are common, highlighting the need for repeat sampling. While most cases respond to corticosteroids, TNF-α inhibitors may help in refractory disease. This case highlights the importance of considering EGIDs in post-bariatric patients with persistent GI symptoms and eosinophilia.
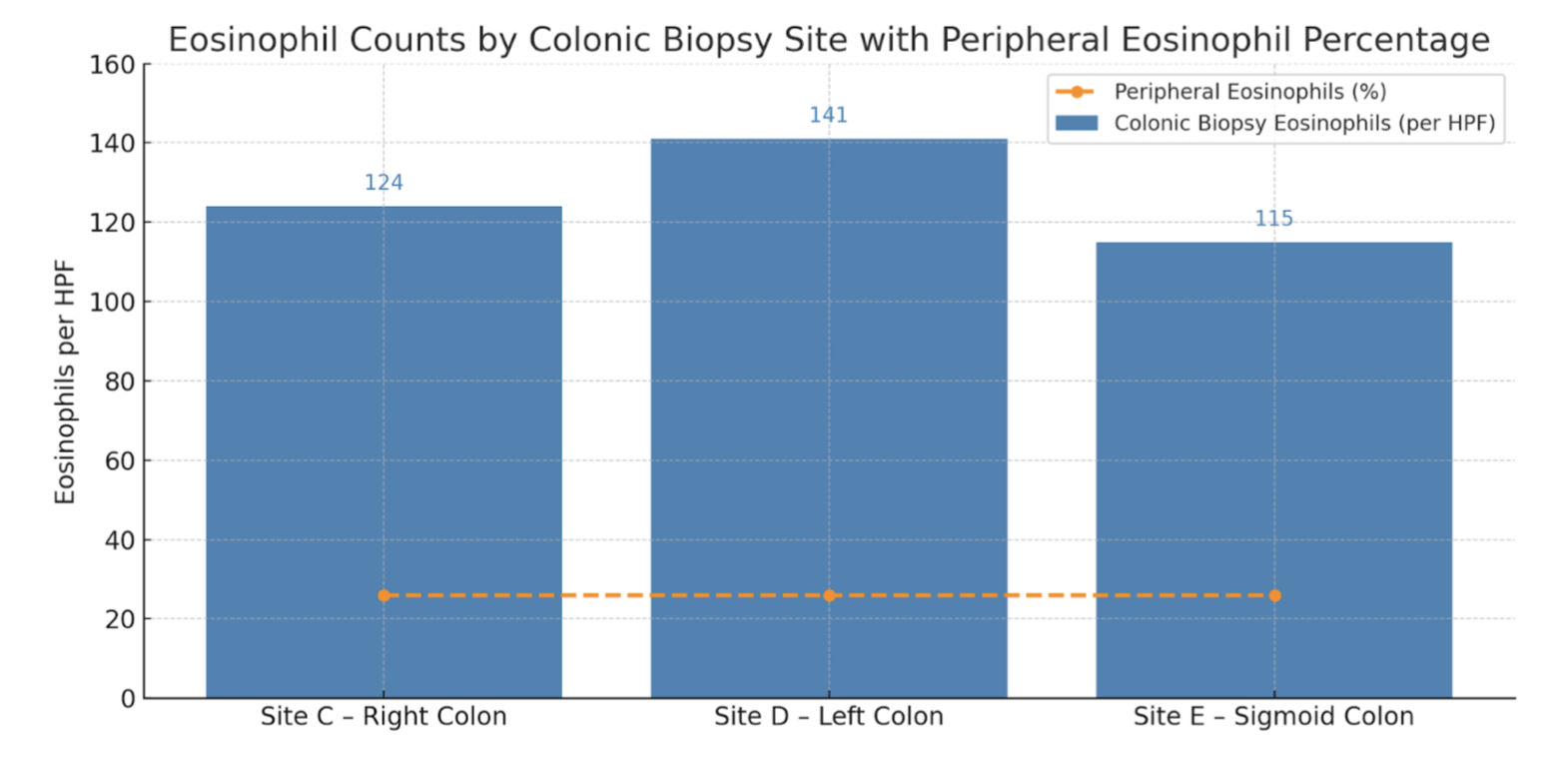
Figure: Table 1: Eosinophil counts from colonic biopsy sites and peripheral blood: Colonic biopsies revealed marked eosinophilic infiltration in the lamina propria: Site C – Right Colon (124 eosinophils/HPF), Site D – Left Colon (141 eosinophils/HPF), and Site E – Sigmoid Colon (115 eosinophils/HPF). A horizontal dashed line represents peripheral eosinophilia (26%), highlighting the coexistence of systemic and tissue-level eosinophilic inflammation. These findings supported the diagnosis of eosinophilic colitis.
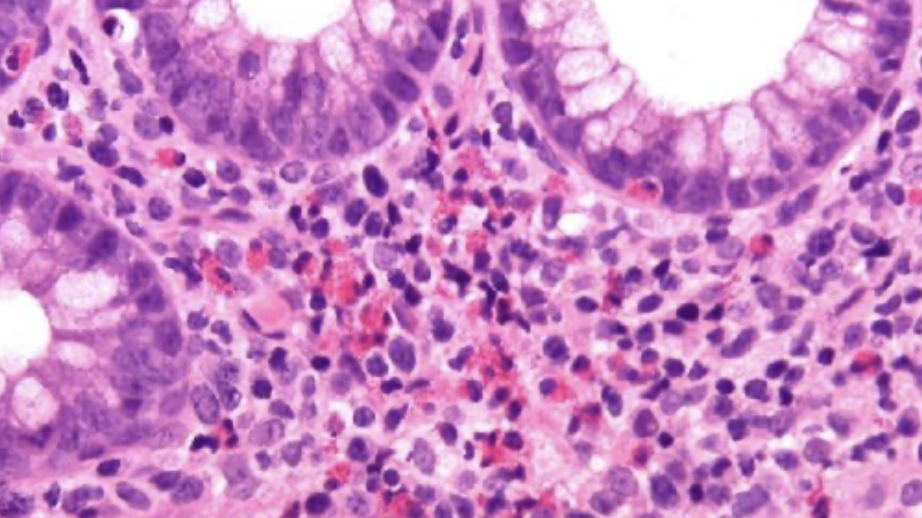
Figure: Image 1: Eosinophilic colitis. Presence of numerous eosinophils, in aggregate and sheets in the lamina propria and infiltrating the crypt epithelium. H&E magnification 40x.
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Zoe Post indicated no relevant financial relationships.
Atsushi Sakuraba indicated no relevant financial relationships.
Maham Lodhi indicated no relevant financial relationships.
Joseph Frasca indicated no relevant financial relationships.
Veena Nannegari indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Atsushi Sakuraba, MD, PhD1, Maham Lodhi, MD1, Joseph Frasca, MD1, Veena Nannegari, MD2. P5524 - Eosinophilic Colitis Following Roux-en-Y Gastric Bypass: A Rare Case of Postoperative Eosinophilic Gastrointestinal Disease in an Atopic Adult, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
