Tuesday Poster Session
Category: IBD
P5516 - Silent Perforation: A Case of Asymptomatic Bowel Perforation in Crohn’s Disease in a Patient With Autism Spectrum Disorder
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

McKenna Andrews, MD
East Tennessee State University
Kingsport, TN
Presenting Author(s)
McKenna Andrews, MD1, David W. Berry, DO2, Aamir-Ali Shaikh, BS, MPH3, Venkata Pulivarthi, MD2
1East Tennessee State University, Kingsport, TN; 2East Tennessee State University, Johnson City, TN; 3East Tennessee State University, Knoxville, TN
Introduction: Crohn’s disease (CD) is a chronic inflammatory bowel condition marked by recurrent inflammation, most commonly in the terminal ileum. Though its pathophysiology is multifactorial, involving genetic, environmental, and immune components, complications such as strictures, fistulas, abscesses, and bowel perforation are common. Up to 90% of CD patients ultimately require surgery, yet recurrence rates remain high. Bowel perforation, while life-threatening, can sometimes be managed non-operatively if clinically contained, especially in stable patients.
Such decisions are particularly challenging in nonverbal patients with autism spectrum disorder (ASD), where symptom reporting is limited. Clinicians must rely on surrogate markers like behavior changes, vital signs, or facial expressions, which are often subjective and may be misinterpreted. Corticosteroids remain a cornerstone of CD flare treatment but are controversial in suspected perforation due to risks of masking infection and impairing healing. This case highlights how careful clinical judgment and multidisciplinary oversight can guide successful conservative management in such complex presentations.
Case Description/
Methods: A 27-year-old nonverbal male with CD, ASD, and prior cholecystectomy to clinic with two weeks of decreased appetite, and persistently elevated heart rate and blood pressure. Physical exam findings were benign. Computed tomography (CT) imaging revealed terminal ileum wall thickening, fat stranding, and extraluminal air and fluid, suggestive of bowel perforation (Image 1). CRP was elevated at 64 mg/L. The patient was managed with bowel rest, intravenous (IV) fluids, methylprednisolone, and empiric Zosyn. Despite imaging findings, general surgery and gastrointestinal teams recommended conservative management given his stable exam and absence of peritoneal signs. Stool studies were negative, and the patient improved clinically with steroid therapy. He was discharged on a prednisone taper and remained stable on outpatient follow-up.
Discussion: This case illustrates the importance of individualized care in complex scenarios involving CD and ASD. Radiologic evidence of perforation typically prompts surgical intervention, yet our patient improved with medical management alone. In nonverbal patients, multidisciplinary collaboration is essential, as behavioral cues are easily misread. Ultimately, this case supports flexible, patient-centered strategies that integrate clinical, radiologic, and behavioral assessments.
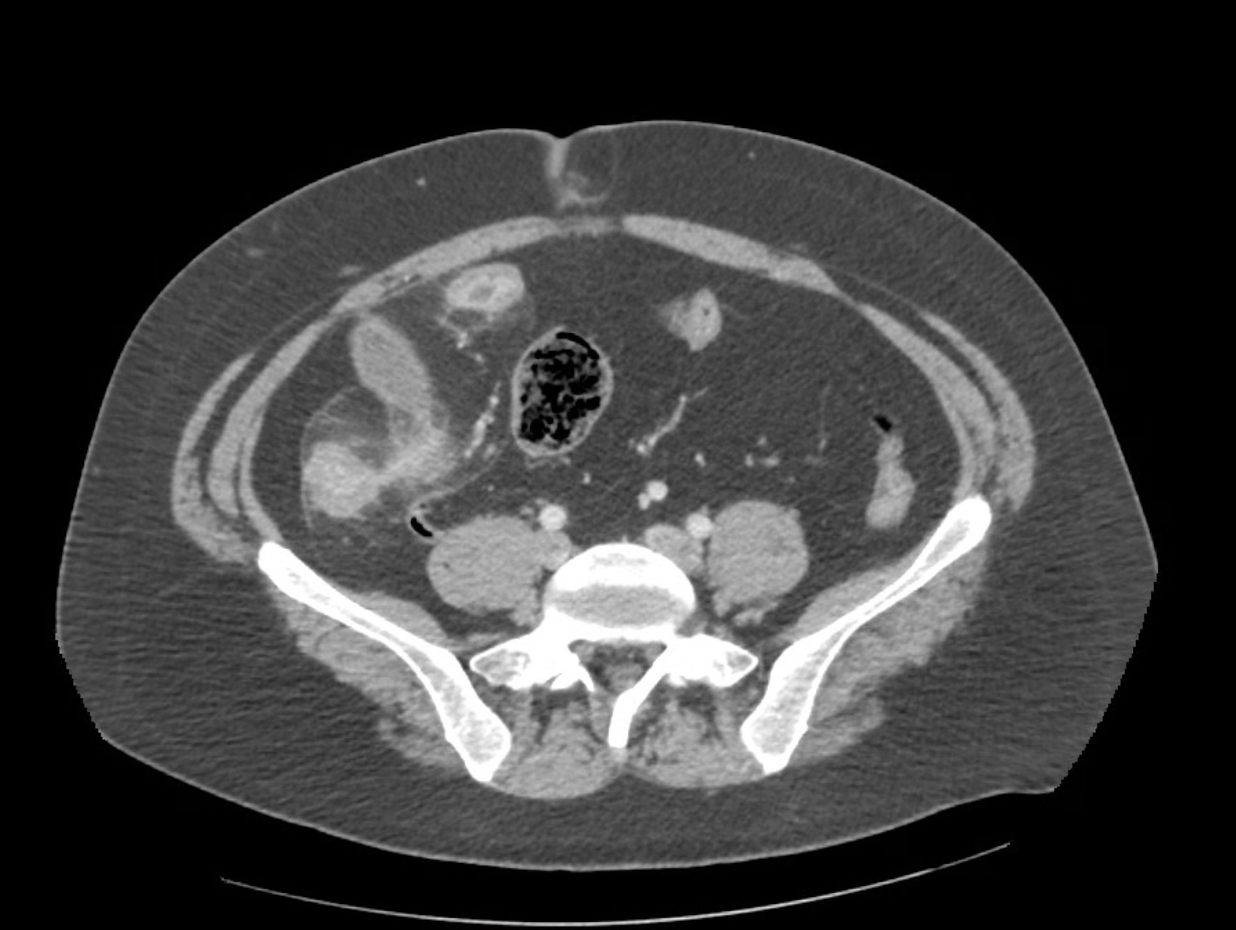
Figure: Image 1. Axial abdominal CT demonstrating terminal ileal wall thickening with surrounding fat stranding and the presence of extraluminal air and fluid, findings concerning for bowel perforation.
Disclosures:
McKenna Andrews indicated no relevant financial relationships.
David Berry indicated no relevant financial relationships.
Aamir-Ali Shaikh indicated no relevant financial relationships.
Venkata Pulivarthi indicated no relevant financial relationships.
McKenna Andrews, MD1, David W. Berry, DO2, Aamir-Ali Shaikh, BS, MPH3, Venkata Pulivarthi, MD2. P5516 - Silent Perforation: A Case of Asymptomatic Bowel Perforation in Crohn’s Disease in a Patient With Autism Spectrum Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1East Tennessee State University, Kingsport, TN; 2East Tennessee State University, Johnson City, TN; 3East Tennessee State University, Knoxville, TN
Introduction: Crohn’s disease (CD) is a chronic inflammatory bowel condition marked by recurrent inflammation, most commonly in the terminal ileum. Though its pathophysiology is multifactorial, involving genetic, environmental, and immune components, complications such as strictures, fistulas, abscesses, and bowel perforation are common. Up to 90% of CD patients ultimately require surgery, yet recurrence rates remain high. Bowel perforation, while life-threatening, can sometimes be managed non-operatively if clinically contained, especially in stable patients.
Such decisions are particularly challenging in nonverbal patients with autism spectrum disorder (ASD), where symptom reporting is limited. Clinicians must rely on surrogate markers like behavior changes, vital signs, or facial expressions, which are often subjective and may be misinterpreted. Corticosteroids remain a cornerstone of CD flare treatment but are controversial in suspected perforation due to risks of masking infection and impairing healing. This case highlights how careful clinical judgment and multidisciplinary oversight can guide successful conservative management in such complex presentations.
Case Description/
Methods: A 27-year-old nonverbal male with CD, ASD, and prior cholecystectomy to clinic with two weeks of decreased appetite, and persistently elevated heart rate and blood pressure. Physical exam findings were benign. Computed tomography (CT) imaging revealed terminal ileum wall thickening, fat stranding, and extraluminal air and fluid, suggestive of bowel perforation (Image 1). CRP was elevated at 64 mg/L. The patient was managed with bowel rest, intravenous (IV) fluids, methylprednisolone, and empiric Zosyn. Despite imaging findings, general surgery and gastrointestinal teams recommended conservative management given his stable exam and absence of peritoneal signs. Stool studies were negative, and the patient improved clinically with steroid therapy. He was discharged on a prednisone taper and remained stable on outpatient follow-up.
Discussion: This case illustrates the importance of individualized care in complex scenarios involving CD and ASD. Radiologic evidence of perforation typically prompts surgical intervention, yet our patient improved with medical management alone. In nonverbal patients, multidisciplinary collaboration is essential, as behavioral cues are easily misread. Ultimately, this case supports flexible, patient-centered strategies that integrate clinical, radiologic, and behavioral assessments.
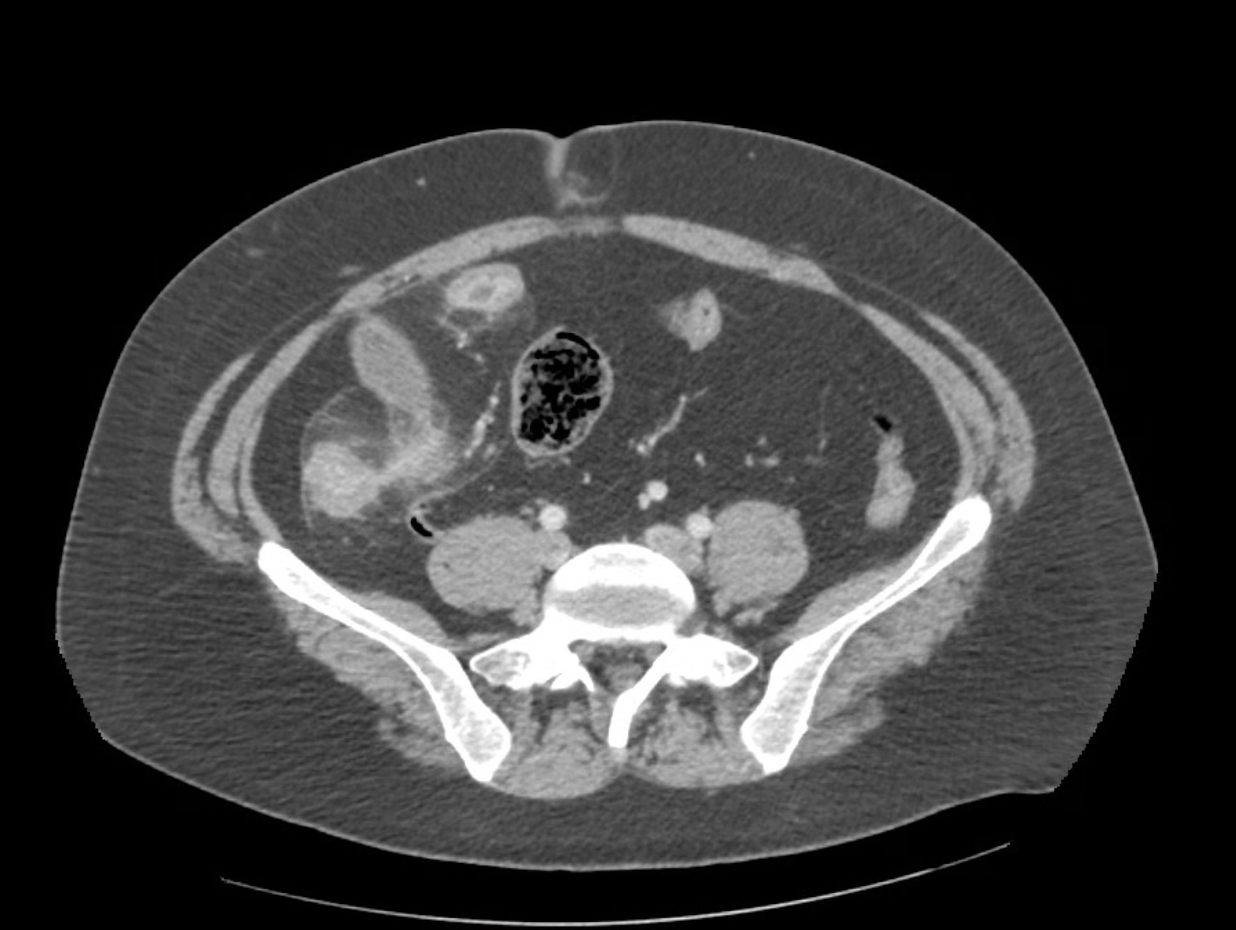
Figure: Image 1. Axial abdominal CT demonstrating terminal ileal wall thickening with surrounding fat stranding and the presence of extraluminal air and fluid, findings concerning for bowel perforation.
Disclosures:
McKenna Andrews indicated no relevant financial relationships.
David Berry indicated no relevant financial relationships.
Aamir-Ali Shaikh indicated no relevant financial relationships.
Venkata Pulivarthi indicated no relevant financial relationships.
McKenna Andrews, MD1, David W. Berry, DO2, Aamir-Ali Shaikh, BS, MPH3, Venkata Pulivarthi, MD2. P5516 - Silent Perforation: A Case of Asymptomatic Bowel Perforation in Crohn’s Disease in a Patient With Autism Spectrum Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
